Tag: Hospice Care
Articles about hospice care including how to manage comfort at end of life.
Articles about hospice care including how to manage comfort at end of life.

As a hospice registered nurse case manager, I'm here to provide you with information, support, and guidance through this grim time. In this article, we'll explore what to expect over the course of the disease, the changes you might observe in your loved one, and how to provide the best care from the onset of the illness until the end of life.
Navigating the tender journey of hospice care, Compassion Crossing offers guidance on addressing the pivotal question of “when?”—a beacon for caregivers seeking solace and understanding in life’s final chapter.
The purpose of this article is to provide you with some information and guidance about AAAs and how they can be managed in hospice patients.
Dealing with a loved one in end stage coma can be an emotionally challenging and overwhelming experience. As an experienced nurse with years of experience, I understand the importance of providing compassionate care and support during this difficult journey. In this article, we will explore what to expect during the course of the disease, changes you might see in your loved one, and essential tips for caring for them from onset until death.
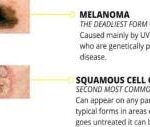
Discover essential information about squamous cell carcinoma, including its causes, symptoms, and treatment options. This comprehensive guide offers valuable insights for families and caregivers, helping you navigate the challenges of supporting a loved one diagnosed with this form of skin cancer.

Explore the complexities of hospice care for terminally ill patients with multiple diagnoses. Learn how to distinguish between related and unrelated conditions, understand Medicare coverage, and navigate the challenges of providing comprehensive care while adhering to hospice regulations and ethical standards.

Dementia gets worse over time, and as caregivers, we want to support our loved ones through every stage. In the severe stages of dementia, a person's body may begin to fail significantly. Here are seven ways to promote their quality of life during this challenging time.
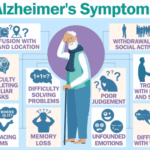
Discover essential guidance for caring for a loved one with Alzheimer's disease, from early symptoms to end-of-life care. Learn about communication strategies, safety measures, and self-care tips for caregivers. This comprehensive guide offers support and practical advice for navigating the challenges of Alzheimer's caregiving.

LATE, a newly recognized form of dementia affects memory and behavior in older adults. Learn about its symptoms, diagnosis, and how it differs from Alzheimer's. Discover practical tips for caregivers to provide compassionate support and improve the quality of life for loved ones with LATE.

Identifying when a patient may benefit from hospice care is a critical yet often challenging task. For caregivers, including Certified Nursing Assistants (CNAs) and Medical Technicians (Med Techs), visual observation can be a powerful tool for recognizing signs that suggest a hospice referral might be appropriate.
This guide is tailored to assist caregivers in personal care facilities in identifying these signs through visual observation methods, helping provide compassionate and timely end-of-life care.
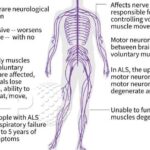
Discover the essentials of ALS, from its symptoms and progression to treatment options and support strategies. This comprehensive guide empowers families facing an ALS diagnosis with knowledge and practical advice, helping them navigate the challenges and provide the best care for their loved ones.
If you are caring for a terminally ill patient in hospice, you know how challenging it can be to manage their medications. You want to make sure they are getting the best possible care, but you also want to avoid unnecessary or harmful drugs that may worsen their quality of life or cause adverse effects.
That’s where medication reconciliation and deprescribing come in. Medication reconciliation is the process of reviewing and updating the patient’s medication list to ensure accuracy and completeness. Deprescribing is the process of reducing or stopping medications that are no longer needed, effective, or appropriate for the patient’s condition and goals of care.

Memory care admission can be a challenging journey, especially when a family member is grappling with dementia. This transition demands logistical considerations and a deep understanding of the emotional and psychological aspects. As an experienced hospice nurse, I've encountered numerous families navigating this path, and here's a guide to compassionately help your loved one with dementia transition to a memory care unit.
Receiving news that a loved one has reached the end-stage of a stroke can be overwhelming and emotionally challenging. As an experienced hospice nurse with years of experience, I understand how crucial it is for families to have accurate information about what to expect during this journey. In this article, we will explore the changes that may occur in a loved one with end-stage stroke and how you can best care for them throughout this process.

If you are a caregiver for someone with dementia who has lost trunk control, you may wonder how you can help them. Repositioning is one way you can help. Repositioning means moving or turning the person to a different position. It can help improve the person’s comfort, skin health, and blood flow. It can also prevent or treat pressure ulcers, contractures, falls, and infections.
In this article, we will share some tips for repositioning dementia patients who have lost trunk control. These tips are based on the latest research and best practices. We hope these tips will help you provide better care for your loved one.

This article provides hospice nurses with practical and evidence-based strategies to discuss end-of-life care with families
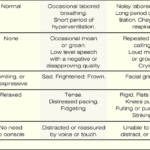
The PAINAD scale is a comprehensive tool that assesses and manages pain in older adults with dementia and delirium. It focuses on observable signs of pain rather than patient self-report, making it particularly useful for individuals who cannot communicate their discomfort
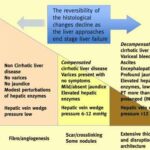
Having a loved one diagnosed with liver disease can be a challenging and emotional journey for both the patient and their family. As an experienced hospice nurse with years of experience in hospice care, I understand the importance of providing compassionate and informative support during this grim time. In this article, we will explore what to expect over the course of liver disease, the changes that may occur in your loved one, and how to provide the best care from onset until the end of life.

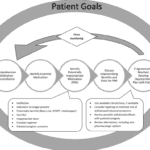
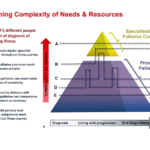
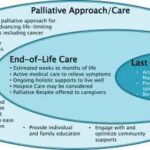
Discover hospice care, eligibility, benefits, provider choice, costs, services, and more. Learn how hospice addresses physical, emotional, spiritual, and social needs and how to prepare for and manage them. Find out about the roles of the hospice team and the primary caregiver and the signs of approaching death. Empower yourself with the knowledge to make informed decisions about compassionate end-of-life care.
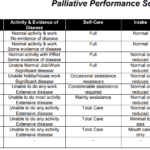
Explore the Palliative Performance Scale (PPS) and its crucial role in end-of-life care. Learn how this tool helps hospice professionals assess patient decline, predict life expectancy, and provide tailored care. Understand the significance of PPS changes in the final six months and how they guide compassionate care decisions.
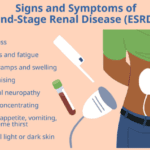
If your loved one has been diagnosed with End Stage Renal Failure, it's natural to feel overwhelmed and unsure about what to expect during the disease. As an experienced hospice nurse with years of experience, I am here to guide you through this journey with compassion and empathy. In this article, we will cover what end-stage renal Failure is, the changes you may observe in your loved one, and how to provide the best care from onset until the end of life.
Explore the compassionate approach of hospice nursing assessments, emphasizing patient comfort and dignity over conventional hospital metrics. This article delves into the personalized care that defines hospice evaluations, ensuring a serene transition for patients and families.

Losing a loved one to a terminal illness is an incredibly challenging experience. It's a journey filled with emotions, uncertainties, and the need for profound empathy. One crucial aspect of this journey is saying goodbye to your dying loved one and permitting them to pass peacefully. In this article, we'll explore the significance of these acts, which bring comfort to the terminally ill and aid in the grieving process for those left behind. We'll also share three case studies to illustrate the importance of these actions.

Losing a loved one is an incredibly challenging and emotional experience, and witnessing someone's final moments can be overwhelming, especially if you have never been through it before. As a hospice nurse with years of experience, I understand the importance of providing guidance and support during this time. In this article, I want to help prepare you for what to expect during the death visit and explain the role of the hospice registered nurse in the pronouncement process.