Category: Ethics
Articles about end-of-life ethical issues including ethical dilemmas
Articles about end-of-life ethical issues including ethical dilemmas

Caring for a terminally ill loved one at home is an incredibly challenging and emotional journey for family caregivers. This guide acknowledges the struggles you may face and offers compassionate solutions. It explores valuable resources, such as end-of-life doulas, PACE programs, and professional home care services, all designed to help ease your burden and provide support during this difficult time. You are not alone in this experience; there are ways to find relief and comfort as you navigate these profound challenges.
This comprehensive guide helps patients, families, and healthcare professionals confidently navigate POLST decisions. Learn the essential steps, understand your options, and ensure your end-of-life care wishes are honored through proper planning and communication.

This article delves into Utilization Behavior in dementia, offering practical advice for families and caregivers to create a safe environment and mitigate the challenges associated with this condition.

Discover the essentials of hiring caregivers for terminally ill patients. This guide covers caregiver qualifications, assessing understanding of terminal care, and practical hiring tips.
This comprehensive guide provides valuable insights on how to report and prevent elderly abuse in nursing homes. It serves as a resource for families, guardians, and loved ones to understand their roles and responsibilities in advocating for the elderly. Learn how to empower yourself and ensure the safety and well-being of your loved ones.
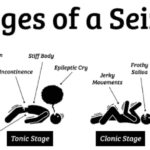
We understand that caring for a loved one in hospice can be a journey filled with compassion, love, and sometimes, uncertainty. When seizures are part of this journey, it’s natural to have concerns and questions. This guide is here to walk alongside you, offering knowledge and support as you navigate the complexities of seizure management in hospice settings.

Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules.

This guide helps families of terminally ill patients comprehend absolute vs. relative risk reduction. It’s a resource for making educated choices about medication continuation, tapering, or cessation in collaboration with healthcare professionals.

This article delves into the intricate dynamics of hospice nurses’ relationships with patients, examining the benefits and challenges of emotional investment versus professional detachment.

This article delves into the challenges faced by family caregivers in hospice and palliative care, offering practical strategies and resources to support them in their indispensable roles.
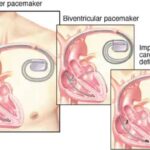
Learn about the differences between pacemakers and ICDs, their functions, and the implications for patients and caregivers. Discover why pacemakers should stay on, and ICDs should be turned off at the end of life for comfort and dignity.

Hospice care is often seen as the final chapter, but sometimes, it leads to unexpected recoveries. This article explores stories of resilience and healing in hospice care, reminding us that hope and recovery can still be part of the journey.

This comprehensive guide empowers families to navigate care plan meetings for terminally ill loved ones. Learn the significance of these meetings, how to prepare, communicate your loved one's needs, and advocate for their best interests. Gain insights into recognizing when meetings are necessary and the benefits of regular care planning. Equip yourself with the knowledge to ensure your loved one receives personalized, dignified care aligned with their wishes.

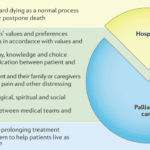
When a loved one is facing a serious illness, it can feel like standing at a crossroads. Each path represents a different way to care for them in their time of need. It’s a moment filled with tough choices and deep emotions. This article thoroughly explains hospice care, its philosophy, and the benefits it provides to patients and families facing terminal illness. Learn about the decision-making process, the hospice experience, and how to navigate this difficult choice with dignity and love.
Dive into the world of Selective Serotonin Reuptake Inhibitors (SSRIs) and their role in treating depression. Discover the importance of medication half-life, the risks of serotonin syndrome, and why the chemical imbalance theory of depression is being challenged. Learn about the concerns of overprescription in older adults.
Discover the truth behind the myth that medications can keep terminally ill patients alive indefinitely. This article explores the psychological factors behind this belief and its consequences while providing compassionate strategies to cope with the reality of losing a loved one while ensuring quality end-of-life care.

Delve into the world of blood-based biomarkers for dementia detection. This article examines the science behind these tests, their potential to revolutionize early diagnosis, and the complex ethical considerations surrounding their use. Discover how these tests might shape the future of Alzheimer's care and research.
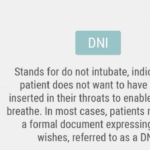
If you or your loved one has a severe illness, you may have heard about do not resuscitate (DNR) orders. This medical order tells the health care team what to do if the patient’s heart stops beating or they stop breathing. It is an incredibly crucial decision that can affect the quality and length of life. However, there are many myths and misunderstandings about DNR orders that can make it hard to choose what is best for you or your loved one. In this article, we will explain what DNR orders means and why it is important to understand it. We will also debunk the top ten myths about DNR orders and share the facts that can help you make an informed and respectful choice.

You may think that CPR is a miracle that can save anyone’s life, but that is not always the case. CPR is not practical for terminally ill patients, and it can cause more harm than good. In fact, studies show that only about 5% of terminally ill patients who receive CPR survive to leave the hospital. Many of them suffer from brain damage, broken ribs, or infections because of CPR.
This article aims to help you understand the truth about CPR for terminally ill patients. We will debunk ten common myths you may have heard or believed about CPR and provide you with accurate and reliable information. We will also help you make informed and respectful decisions about CPR for your loved one based on their wishes and values.

A groundbreaking skin test has emerged as a potential game-changer in the early detection of Parkinson's disease and related disorders. This article explores the science behind the test, its accuracy, and the ethical implications of early diagnosis. Discover how this innovative approach could revolutionize Parkinson's treatment and patient care.
Choosing between full code and DNR for terminally ill patients can be challenging. This article explains the differences, benefits, and drawbacks of helping caregivers and families make informed decisions.
Hospice care is often misunderstood. A common myth suggests that once a patient with a terminal illness enters hospice, they lose control over their care. This article aims to dispel this misconception and highlight the central role of patient and family autonomy in hospice settings. It's important to note that this discussion primarily applies to patients receiving care at home or in non-facility settings, as facility-based patients may have less control over their care decisions.

Explore the complex decision of using antibiotics in end-of-life care. This article weighs the potential benefits against risks, considering comfort, quality of life, and ethical concerns. Learn how to make informed choices with your healthcare team for compassionate, patient-centered care in life's final stages.

Shielding children from death deprives them of understanding this natural part of life, leading to emotional and psychological consequences. This article explores why exposing children to the dying process is essential for their development and highlights the role of hospice care in supporting families during this time.