Category: Medications
Medications used for symptom management or otherwise
Medications used for symptom management or otherwise
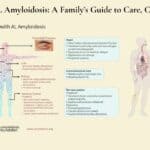
AL amyloidosis is an uncommon yet severe condition that impacts various organs. This detailed guide provides essential information for patients and their families regarding symptoms, disease progression, treatment options, and the timing of considering hospice care for their loved one.
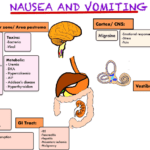
Nausea and vomiting are common and distressing symptoms in terminally ill patients. This comprehensive guide offers practical advice for caregivers and healthcare professionals on managing these symptoms, including pharmacological and non-pharmacological approaches, diet and lifestyle changes, and when to seek additional help.

Discover the advantages of low-dose dexamethasone in palliative care, including when to start, what to monitor, and guidelines for tapering off. Ensure optimal patient comfort and care.

This guide helps families of terminally ill patients comprehend absolute vs. relative risk reduction. It’s a resource for making educated choices about medication continuation, tapering, or cessation in collaboration with healthcare professionals.
Dementia can lead to aggressive behavior in elderly patients, causing distress for both them and their caregivers. This comprehensive guide explores the underlying causes of aggression, from sleep disturbances to medication side effects, and offers practical, empathetic strategies for managing these challenging situations and improving the quality of life for all involved.
Explore the complex world of dementia-related aggression and learn how to identify its underlying causes. This comprehensive guide offers insights into medication-related issues, pain management, and non-pharmacological interventions. Discover compassionate care strategies to support patients and caregivers on this challenging journey.
Dive into the world of Selective Serotonin Reuptake Inhibitors (SSRIs) and their role in treating depression. Discover the importance of medication half-life, the risks of serotonin syndrome, and why the chemical imbalance theory of depression is being challenged. Learn about the concerns of overprescription in older adults.

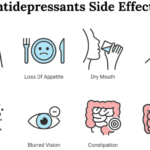
Medications like anticoagulants, antidepressants, and NSAIDs can cause harm to hospice patients. Learn how to balance comfort and safety with individualized care.
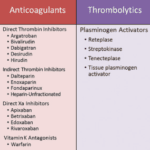
Anticoagulants can prevent blood clots but also cause bleeding risks for terminally ill patients. This article explains why these medications should be regularly reviewed for deprescribing, outlining factors like prognosis, preferences, and palliative care options to consider when making informed, compassionate choices aligned with the patient's goals.

This article aims to overview Pennsylvania medication technicians' training and certification process and discuss specific skills and knowledge needed to perform their duties effectively and safely.

Explore why side effects from medications can emerge after initial use and understand the critical need for vigilant monitoring and regular medication reconciliation to ensure patient safety and efficacy.
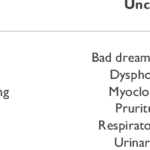
Learn about uncommon opioid side effects like myoclonus and hyperalgesia, and how they impact you and your family. This guide explains these conditions, offers tips for managing them, and highlights the role of hospice in providing comfort and support.

In this episode of Hospice Explained, host Marie Betcher, RN, interviews Nurse Peter Abraham. Peter shares his extensive experience in cardiac telemetry, skilled nursing, and rural home hospice care. They discuss the significance of early hospice enrollment, the challenges of caring for dementia and Parkinson's patients, and the impactful personal stories from Peter's career. Special focus is given to the educational resources on Peter's website, Compassion Crossing, which aims to support families, caregivers, and new hospice nurses. Peter emphasizes the importance of compassion and understanding in hospice care and reflects on how his faith informs his practice.
Discover how oral ketamine is emerging as a game-changer in palliative care, offering rapid relief for severe depression, anxiety, and emotional distress. This comprehensive guide explores its potential benefits, administration methods, and important considerations for patients and healthcare providers.

Explore comprehensive approaches to managing hallucinations in loved ones with dementia. This article covers pharmacological methods, focusing on Seroquel and non-drug strategies such as Naomi Feil's validation therapy. Learn how to validate feelings, de-escalate fear, and improve the quality of life for those experiencing cognitive impairment.

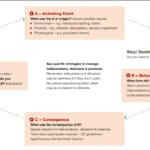
Discover effective strategies for managing end-of-life crises in hospice care. Learn how to recognize signs of distress, implement calming techniques, and provide compassionate support to patients and families. This guide offers practical tips for hospice nurses and caregivers to navigate challenging situations with confidence and empathy.
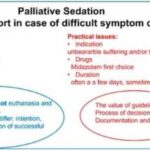
This guide covers the essentials of palliative sedation for hospice patients, including ethical dilemmas, timing, recommended medications, and monitoring effectiveness, ensuring comfort during the end-of-life journey.
This article delves into the intricate relationship between dementia and seizures, offering insights on identification, safety protocols, and advocacy for caregivers.
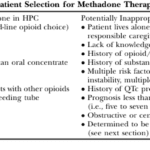
This article delves into the advantages of Methadone over Morphine for pain management in hospice settings. It covers dosage, titration, side effects, and scenarios where Methadone may not be the best choice. Ideal for hospice professionals and caregivers seeking compassionate pain relief options for the terminally ill.

Discover the potential side effects of dementia medications and how to support your loved one. Stay informed!
Learn effective strategies for managing hallucinations in terminally ill patients. This guide covers pharmacological and non-pharmacological methods to improve comfort and quality of life.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.
When a loved one is terminally ill, it can be a perplexing and emotional journey. Understanding the root cause of their declining health becomes paramount. It's a complex puzzle where family members often grapple with questions: Are the symptoms a result of medications prescribed, or are they intrinsic to the terminal disease? This article delves into the critical distinctions between medication side effects and the natural progression of terminal illnesses, offering insights to empower families and caregivers in making informed decisions about their loved one's care.

Serotonin syndrome is a potentially life-threatening condition caused by an excess of serotonin in the body. Detecting this condition early is crucial, but it can be particularly challenging when dealing with dementia patients due to communication barriers and the complexity of their symptoms. In this article, we will present three case studies that highlight the early detection and successful management of serotonin syndrome in patients with different types of dementia: Alzheimer's disease, vascular dementia, and Lewy Body Dementia.