Understanding Lewy Body Dementia: A Guide for Families
Published on October 2, 2023
Updated on July 12, 2024
Published on October 2, 2023
Updated on July 12, 2024
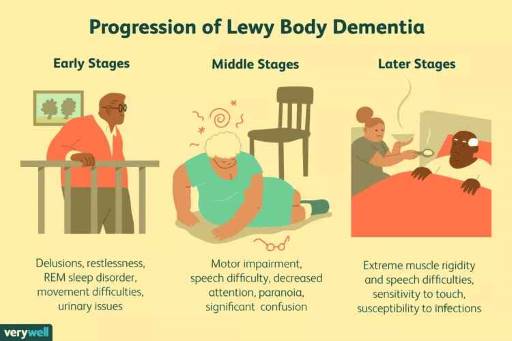
Table of Contents
Lewy Body Dementia (LBD) is a complex and challenging condition that affects millions of individuals worldwide. As a hospice nurse with years of experience, I understand the importance of providing families with clear and compassionate information about what to expect when a loved one is diagnosed with LBD. This article will discuss LBD, its common symptoms and progression, and practical tips for providing care and support throughout the journey, from onset until the end of life.

Lewy Body Dementia is a progressive brain disorder characterized by abnormal protein deposits called Lewy bodies in the brain. These deposits disrupt the normal functioning of brain cells, leading to cognitive, physical, and behavioral changes. LBD is a challenging condition as it shares symptoms with other neurodegenerative disorders like Alzheimer’s and Parkinson’s disease, making diagnosis and management complex.
Lewy Body Dementia (LBD) exhibits unique characteristics that set it apart from other forms of dementia. To provide clarity, let’s explore the key distinctions between LBD and two common forms of dementia: Alzheimer’s disease and vascular dementia:
1. Presence of Lewy Bodies
2. Motor Symptoms
3. Visual Hallucinations
4. Fluctuations in Cognitive Function
5. Psychiatric Symptoms
6. Response to Medications
Lewy Body Dementia (LBD) differs from other types of dementia due to the presence of Lewy bodies, motor symptoms resembling Parkinson’s disease, prominent visual hallucinations, fluctuations in cognitive function, and psychiatric symptoms.
The progression of Lewy Body Dementia can vary from person to person, but it generally follows these stages:
Providing care for someone with LBD requires patience, compassion, and understanding. Here are some practical tips to support your loved one throughout their journey:
Remove hazards and install handrails to prevent falls: People with LBD may have trouble walking or balancing, and they may fall easily. You can make your home safer by removing things that they could trip over, such as rugs, cords, or clutter. You can also install handrails or grab bars in the bathroom, bedroom, and stairs to help them get up or down. You can also use a bed rail or a low bed to prevent them from falling out.
Ensure proper lighting to reduce visual hallucinations: People with LBD may see things that are not there, especially in the dark or in dim light. You can help them by ensuring enough light in the rooms they use, such as lamps, nightlights, or windows. You can also avoid using mirrors, shiny objects, or patterns that may confuse them or make them see things.
Maintain a consistent daily schedule to help reduce anxiety and confusion: People with LBD may feel more calm and secure if they have a routine that they can follow. You can help them by keeping a consistent schedule for their meals, medications, activities, and bedtime. You can also use a calendar, a clock, or a whiteboard to remind them of the date, time, and what they need to do. You can also avoid changing their environment or caregivers too often, which may confuse or make them anxious.
Use simple, clear language and give one-step instructions: People with LBD may have trouble understanding or remembering what you say, or they may get distracted easily. You can help them by using simple, clear language and speaking slowly and calmly. You can also give them one-step instructions at a time and repeat them if needed. You can also use gestures, pictures, or objects to help them understand. You can also avoid arguing, correcting, or criticizing them, which may upset or make them feel bad. Be patient and allow time for the person to process information.
Encourage activities that your loved one enjoys and can still participate in safely: People with LBD may still enjoy doing things they used to like, such as listening to music, reading, gardening, or playing games. You can help them by finding activities that match their interests, abilities, and mood. You can also adapt the activities to make them easier or safer for them, such as using large-print books, puzzles, or cards or using tools with larger handles or buttons. You can also join them in the activities or praise them for their efforts, which may make them feel happy and valued.
Join support groups to connect with others facing similar challenges: Caring for someone with LBD can be stressful and lonely. You can find support and comfort by joining support groups to meet other caregivers who understand what you are going through. You can also learn from their experiences, tips, and resources. You can find support groups online, by phone, or in person. You can also ask your doctor, social worker, or local Alzheimer’s Association for help.
Educate yourself about LBD to better understand and manage the symptoms: LBD is a complex and unpredictable disease that can affect different people in different ways. You can learn more about LBD by reading books, articles, or websites that explain what LBD is, how it affects the brain and the body, and what treatments are available. You can also ask your doctor, nurse, or pharmacist any questions about LBD or the medications your loved one takes. You can also attend workshops, seminars, or webinars that teach you more about LBD and how to care for someone with LBD.
Take breaks and ask for help when needed: Caring for someone with LBD can be physically and emotionally exhausting. It would help if you also cared for yourself to stay healthy and strong. You can do this by taking breaks from caregiving, such as walking, taking a nap, or doing something you enjoy. You can also ask for help from your family, friends, neighbors, or professionals, such as home health aides, respite care, or adult day care. You can also use meal delivery, transportation, or housekeeping services to make your life easier.
Prioritize your physical and emotional well-being: Caring for someone with LBD can affect your health and happiness. You can protect your well-being by eating well, sleeping enough, exercising regularly, and seeing your doctor when needed. You can also manage stress using relaxation techniques like breathing, meditation, or yoga. You can also express your feelings by talking to someone you trust, such as a friend, a counselor, or a support group. You can also seek professional help if you feel overwhelmed, depressed, or anxious.
Lewy body dementia (LBD) is a progressive disease that affects the brain and causes problems with memory, thinking, movement, behavior, and mood. People with LBD may experience visual hallucinations, fluctuations in alertness, sleep disorders, and Parkinson ’s-like symptoms. LBD can also affect the autonomic nervous system, which controls blood pressure, heart rate, digestion, and other bodily functions.
As LBD progresses, the person may need more care and support from family members and health professionals. Hospice care focuses on comfort and quality of life for people with terminal illnesses and their families. It can be provided at home, a hospice facility, or a nursing home.
Some signs and symptoms that may indicate hospice care is appropriate for someone with LBD are:
Hospice care can provide many benefits for people with LBD and their families. Hospice care can:
Hospice care does not give up on the person with LBD or their family. It is a compassionate and holistic approach to care that honors the person’s dignity, values, and wishes. Hospice care can help the person with LBD, and their family makes the most of the time they have left together.
As LBD progresses, palliative and hospice care can play a crucial role in ensuring comfort and dignity for your loved one. Hospice care focuses on managing symptoms and providing emotional support during the final stages of life. Here are some considerations for end-of-life care:
Have open and honest conversations about your loved one’s preferences for care: People with LBD may not be able to make decisions or communicate their wishes when they are very sick or dying. You can help them by talking to them about what they want and don’t want for their care while they can still tell you. You can also help them make an advance directive, a document that describes what the doctors and nurses should do if they can’t speak for themselves. You can also choose someone to be their healthcare proxy, who can decide for them if they can’t.
Hospice professionals will work to keep your loved one comfortable and pain-free: People with LBD may have pain, trouble breathing, nausea, or other symptoms that make them suffer. You can help them by asking for hospice care, a special care that focuses on making people feel better and not curing their disease. Hospice professionals are doctors, nurses, social workers, and volunteers coming to your home or where your loved one lives. They will give your loved one medicines and treatments to ease their pain and symptoms. They will also support you and your family.
Hospice teams can provide counseling and spiritual guidance for both the patient and family: People with LBD and their families may have many emotions and questions as they face the end of life. You can help them by asking for emotional and spiritual support from the hospice team. They can provide counseling, listening, and advice to help you cope with your feelings and fears. They can also help you find meaning and peace in your situation. They can respect your beliefs and values and help you with your spiritual needs.
Spend quality time with your loved one, sharing memories and providing comfort: People with LBD may still enjoy being with their family and friends, even if they can’t talk or recognize them. You can help them by spending quality time with them, holding their hand, hugging them, or playing their favorite music. You can also share memories, stories, or photos with them and tell them how much you love and appreciate them. You can also comfort them by keeping them warm, clean, and dry and by giving them food and water if they can swallow.
Remember, you are not alone in this journey. Contact healthcare professionals, support groups, and hospice teams to ensure your loved one receives the best care and support.
Understanding Lewy Body Dementia is crucial for families and caregivers to navigate the challenges effectively. A comprehensive approach is essential for recognizing symptoms, implementing care strategies, and preparing for the end of life. Families can provide compassionate care throughout the journey by prioritizing safety, effective communication, and seeking support.
Lewy Body Dementia Symptoms, Diagnosis, and Treatment
Mayo Clinic Lewy Body Dementia
Cleveland Clinic Lewy Body Dementia
Lewy Body Dementia Support Groups
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Lewy Body Dementia (Video)
Trivia Games – Caregiver Activities for Alzheimer’s and Dementia
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Holistic Nurse: Skills for Excellence book series
Dementia Home Care: How to Prepare Before, During, and After
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death