How to Use the Pain Assessment in Advanced Dementia Scale (PAINAD) to Determine Discomfort in Your Loved One with Dementia
Published on October 13, 2023
Updated on April 23, 2024
Published on October 13, 2023
Updated on April 23, 2024
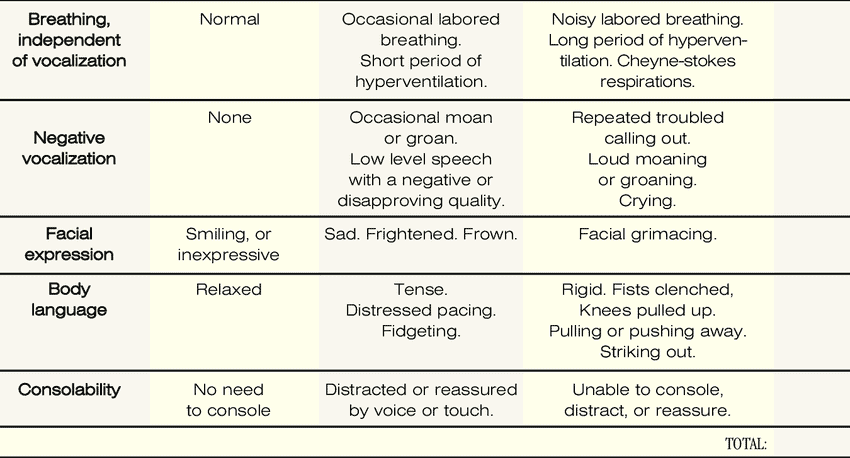
Table of Contents
If you have a loved one with dementia, it can be difficult to know if they are in pain or discomfort. The Pain Assessment in Advanced Dementia Scale (PAINAD) is a tool that can help you determine if your loved one is uncomfortable. The Pain Assessment in Advanced Dementia Scale (PAINAD) is different from other pain assessment tools for people with dementia in several ways:
Other pain assessment tools may rely on self-reporting, which is often challenging for those with advanced dementia. Additionally, they might be complex and time-consuming. The PAINAD’s focus on observable behaviors and ease of use makes it a valuable tool for assessing pain in patients with advanced dementia.
Each area is scored from 0 to 2, resulting in a total score ranging from 0 to 10. A higher score suggests more severe discomfort or pain, while a score between 0 and 2 indicates comfort.
Before using the PAINAD scale, you must observe your loved one for five minutes. During this time, look for behaviors that might indicate discomfort or pain. These behaviors include:
After observing your loved one for five minutes, you can use the PAINAD scale to score their behaviors. The scale uses a score of 0-2 for each behavior, with a total score ranging from 0-10. Here’s how to score each behavior:
Once you have scored your loved one’s behaviors, you can interpret their score. A score of zero (0) means no pain. A score of 1-3 indicates mild discomfort. A score of 4-7 indicates moderate discomfort. A score of 8-10 indicates severe discomfort. Providers should be notified of severe discomfort.
| PAINAD Score | Pain Severity | Recommendations |
|---|---|---|
| 0 | None | None |
| 1-3 | Mild | Nothing to Acetaminophen (Tylenol) |
| 4-7 | Moderate | Opioid / Breakthrough Pain Medication |
| 8-10 | Severe | Call your provider! Opioid / Breakthrough Pain Medication |
You are visiting your grandmother, who has dementia, at her nursing home. You notice that she is smiling and relaxed. She usually breathes and does not make any noises. She does not seem to have any pain in her face or body. She is happy to see you and responds to your voice and touch. You use the PAINAD scale to score her pain as follows:
The total score is 0, which means she has no pain. You are glad that she is comfortable and enjoy spending time with her.
You are helping your father, who has dementia, with his morning routine. He has arthritis and sometimes has pain in his joints. You notice that he is breathing harder than usual and occasionally moans. He looks sad and frowns when you touch his arms or legs. He is tense and fidgets with his hands. He is distracted by your voice and touch but still seems unhappy. You use the PAINAD scale to score his pain as follows:
The total score is 3, which means he has mild pain. You decide to give him his pain medication and massage his joints gently. You hope that his pain will improve soon.
You are taking your mother, who has dementia, to the dentist. She has a toothache and needs a filling. You notice that she is breathing rapidly and deeply. She makes a low-level speech with a negative or disapproving quality. She looks frightened and grimaces when the dentist examines her mouth. She is rigid and pulls away from the dentist. She is unable to console, distract, or reassure. You use the PAINAD scale to score her pain as follows:
The total score is 4, which means she has moderate pain. You ask the dentist to give her some local anesthesia and explain what he is going to do. You hold her hand and talk to her calmly. You hope that the procedure will be over soon and that her pain will go away.
You are watching your husband, who has dementia, at home. He has a urinary tract infection and needs antibiotics. You notice that he is breathing noisily and laboriously. He cries out loud and repeats troubled phrases. He looks angry and facially grimaces. He is rigid and strikes out at you when you try to help him. He is unable to console, distract, or reassure. You use the PAINAD scale to score his pain as follows:
The total score is 7, which means he has severe pain. You call his doctor and ask for advice. You give him his pain medication and try to keep him comfortable. You hope the infection will clear up soon and his pain will subside.
You are accompanying your sister, who has dementia, to the hospital. She has fallen and broken her hip. You notice she is breathing in a rhythmic pattern of very deep to shallow respirations with periods of no breathing. She screams and cries loudly. She looks in agony and facially grimaces. She is rigid and clenches her fists and knees. She is unable to console, distract, or reassure. You use the PAINAD scale to score her pain as follows:
The total score is 10, which means she has severe pain. You alert the hospital staff and ask for immediate help. You give her your support and sympathy. You hope that she will get the treatment she needs and that her pain will be relieved.
The Pain Assessment in Advanced Dementia Scale (PAINAD) is a useful tool for determining if your loved one with dementia is uncomfortable. By observing your loved one’s behaviors and scoring them on the PAINAD scale, you can better understand their level of discomfort and take steps to address it. Remember, discomfort and pain should be treated similarly when it comes to maintaining the comfort of your loved one.
Assessing Pain in the Nonverbal Patient
Discomfort is a different type of pain, but pain nonetheless
Pain Assessment in Hospitalized Older Adults With Dementia and Delirium
Pain Assessment in Dementia – International Association for the Study of Pain (IASP)
Pain Assessment in People with Dementia: AJN The American Journal of Nursing
Pain Assessment in Advanced Dementia Scale (PAINAD) – MDCalc
Uncontrolled Pain and Risk for Depression and Behavioral Symptoms in Residents With Dementia
Pain Assessment and Pharmacologic Management
Adult Nonverbal Pain Scale (NVPS) Tool for pain assessment
Assessing pain in patients with cognitive impairment in acute care
Pain Assessment in Advanced Dementia Scale (PAINAD)
Pain Assessment in Non-Communicative Adult Palliative Care Patients
Pain Assessment in People with Dementia
Tools for Assessment of Pain in Nonverbal Older Adults with Dementia: A State-of-the-Science Review
Understanding the physiological effects of unrelieved pain
Untreated Pain, Narcotics Regulation, and Global Health Ideologies
The Importance of Caregiver Journaling
Reporting Changes of Condition to your Hospice Provider
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death