Is my loved one starving or being dehydrated to death?
When a loved one nears the end of life, it’s natural to worry about their nutrition and hydration. This article explains why they may not need food or water and how you can provide comfort during this time.
-

Managing Aspiration Risks in Hospice Care: A Guide for Families
This article is crafted with heartfelt understanding and care, recognizing the challenges you face as caregivers and family members of terminally ill loved ones. Our goal is to empower you with knowledge and practical advice to manage the risk of aspiration pneumonia, a common yet often preventable complication in hospice care. -
Managing Dysphagia for Comfort: A Guide for Families
Caring for a loved one with dysphagia during their end-of-life journey can be challenging, but with the proper knowledge and support, you can provide them with comfort and dignity. Dysphagia, or difficulty swallowing, is a common symptom in terminally ill patients and can lead to complications if not managed properly. In this guide, we will provide you with essential information on managing dietary changes and what to expect and offer helpful tips and tricks to ensure your loved one’s comfort. -

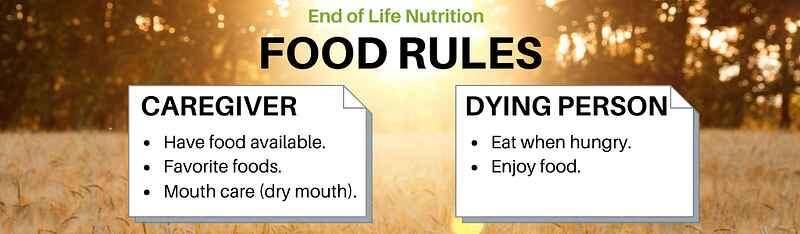
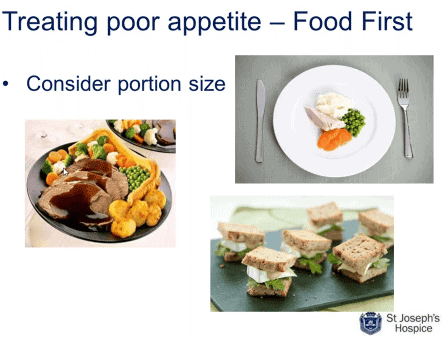
Nourishing with Care: Feeding a Terminally Ill Loved One
Discover compassionate approaches to nourishing terminally ill loved ones. Learn about appetite changes, feeding techniques, and the importance of emotional support during meals. This guide offers practical tips for caregivers to ensure comfort and dignity while addressing nutritional needs in end-of-life care. -

To Wake or Not to Wake: A Dilemma for Caregivers of Dementia Patients in the Final Stage
Caregivers of dementia patients in the final stage face a challenging dilemma: whether to wake their loved ones or let them sleep. This article explores the pros and cons of each approach, offering guidance on making this difficult decision while prioritizing comfort and dignity in end-of-life care. -

Tube Feeding on Hospice — Increased Risk of Your Loved One Suffering
Considering tube feeding for a loved one in hospice? This intervention may not improve quality of life and can lead to discomfort, reduced mobility, and complications. Learn about the risks and make informed decisions for their end-of-life care. -
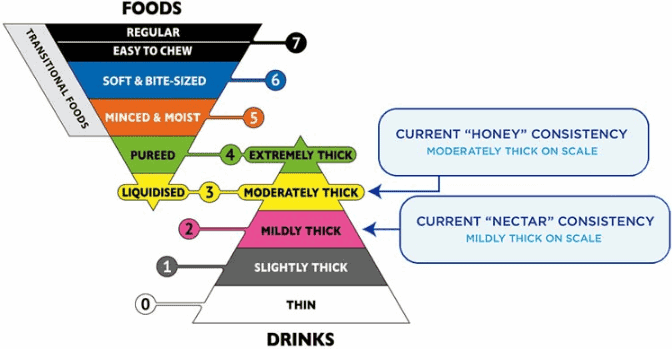
Understanding Changes in Diet Texture for the Terminally Ill
Navigating the dietary needs at life’s end can be complex. This guide explores the progression of diet textures and liquid consistencies, ensuring comfort and safety for the terminally ill. Learn to adapt meals for loved ones as they approach this delicate phase. -
Understanding Nutrition Changes in Hospice: Nourishing Comfort and Peaceful End-of-Life Journey
Explore the natural shift in nutritional needs during hospice care. This guide offers insights into managing reduced calorie intake, ensuring comfort and dignity in the end-of-life journey. -
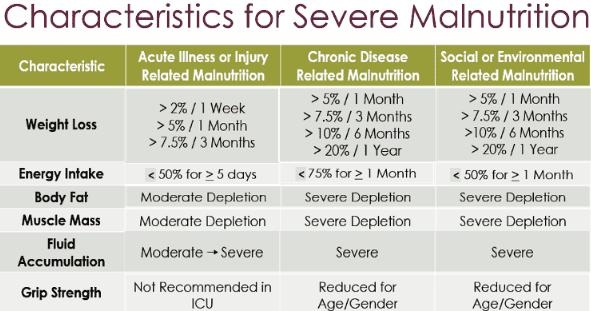
Understanding Protein-Calorie Malnutrition: A Guide for Families
Explore our guide on protein-calorie malnutrition (PCM), a condition hindering proper health for the terminally ill. Learn to recognize symptoms, provide care, and understand the end-of-life journey with our compassionate, informative support for families. -

Understanding the Role of IV Fluids at the End of Life
Explore the delicate balance of IV fluid use at life’s end. This article discusses the hospice approach, potential risks, and prioritizing comfort over invasive measures. A must-read for families facing tough decisions in palliative care.