Importance of Medication Reconciliation in Hospice Care
Published on September 30, 2023
Updated on October 4, 2024
Published on September 30, 2023
Updated on October 4, 2024
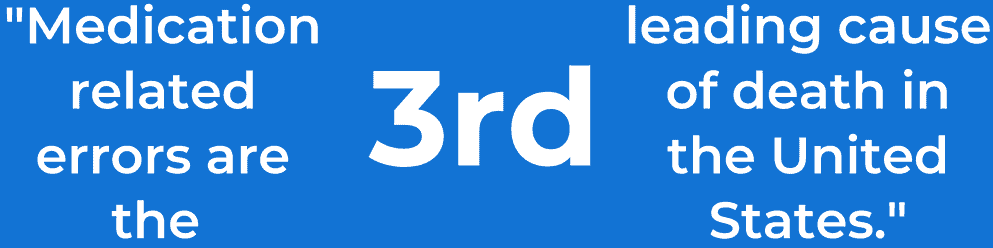
Table of Contents
Medication reconciliation plays a pivotal role in hospice care, ensuring that terminally ill patients receive the most appropriate and safe medication regimens. This process involves creating and maintaining an accurate list of patients’ medications to prevent adverse drug events and enhance their overall well-being. This article will delve into the importance of medication reconciliation, including its recommended frequency and the reconciliation process.
Medication reconciliation is essential at various stages of hospice care, including admission, recertification, changes of condition, medication changes, respite, revocation, and discharge for cause or failure to decline. Here’s why it matters:
In terms of highlighting why medication reconciliation matters so much, I currently have a case where the patient who went into a facility able to walk and talk is now dying because the facility made a change of the PRN morphine to a routine without notifying hospice or the family. It was caught through medication reconciliation in addition to observation and assessment of the patient who is actively dying because of the medication decisions made by the facility.
Medication reconciliation should be performed at several points during a patient’s hospice care, including:
Medication reconciliation involves maintaining a single list documenting a patient’s current medications. This list should be continually updated to reflect changes accurately. Here’s a simplified step-by-step process:
The Beers Criteria is a list of medications that are potentially inappropriate for use in older adults due to the substantial risk of adverse drug reactions. The STOPP/START criteria is a tool for identifying potentially inappropriate medications and potential prescribing omissions in older adults. Healthcare professionals should be familiar with these criteria and use them to guide medication reconciliation in hospice care.
The Beers Criteria is a list of medications that are potentially inappropriate for use in older adults due to their substantial risk of adverse drug reactions. The latest version of the AGS Beers Criteria was written in 2019 to assist practicing clinicians in outpatient, acute, and institutional settings. It includes medications evaluated in five main categories: drugs to avoid, drugs to use with caution, drug-drug interactions, medications to avoid in particular clinical situations, and dosage according to kidney function. The Beers Criteria is a tool used to identify high-risk medications prescribed to older adults with the intent of de-prescribing medications that may lead to adverse drug reactions. By implementing the Beers Criteria into the medication reconciliation process, the primary objective is to increase the number of charts for geriatric patients that have been reviewed for potentially inappropriate medication use. The Beers Criteria serves as standard guidance for clinicians to prevent potentially inappropriate prescribing in patients aged 65.
The Beers Criteria is a list of medications that are potentially inappropriate for use in older adults due to their substantial risk of adverse drug reactions. Here are some examples of medications that are included in the Beers Criteria:
It is important to note that the Beers Criteria is not comprehensive and that healthcare professionals should use their clinical judgment when prescribing medications to older adults.
The STOPP/START criteria are a tool used to identify potentially inappropriate medications and potential prescribing omissions in older adults. The criteria consist of two parts:
The STOPP/START criteria are used as a tool for clinicians to review potentially inappropriate medications in older adults and have been endorsed as a best practice by some organizations. The criteria are used in medication reconciliation to identify medications that may need to be adjusted or discontinued to prevent adverse drug reactions and improve patient outcomes. Several studies have shown that using the STOPP/START criteria can improve medication appropriateness in older adults. The criteria have been used to review the medication profiles of community-dwelling, acute care, and long-term care patients. The criteria have also been effective in preventing polypharmacy in older adults.
The STOPP/START criteria are a tool used to identify potentially inappropriate medications and potential prescribing omissions in older adults. Here are some examples of medications that are included in the STOPP/START criteria:
It is important to note that the STOPP/START criteria are not comprehensive and that healthcare professionals should use their clinical judgment when prescribing medications to older adults. They should also consider a person’s general health, all underlying medical conditions, or circumstances that may lead a healthcare provider to choose a specific medication.
The Beers Criteria and the STOPP/START criteria are both tools used in medication reconciliation to identify potentially inappropriate medications and potential prescribing omissions in older adults. However, there are some critical differences between the two tools:
The STOPP/START criteria are considered more comprehensive and sensitive in assessing potentially inappropriate medications than the Beers Criteria. They offer more benefits than the Beers criteria in improving patient outcomes and medication therapy. However, the Beers Criteria are still widely used in the United States and are considered standard guidance for clinicians to prevent potentially inappropriate prescribing in patients 65 years and older.
The STOPP/START criteria is considered more comprehensive in assessing potentially inappropriate medications (PIMs) than the Beers Criteria. The STOPP/START criteria are more sensitive to assessing potentially inappropriate medications and potential prescribing omissions in older adults. The STOPP/START criteria consider the patient’s clinical status, comorbidities, and other medication appropriateness factors. On the other hand, the Beers Criteria focuses on medications that are potentially inappropriate for use in older adults due to their substantial risk of adverse drug reactions. However, it is important to note that neither tool is perfect, and healthcare professionals should use their clinical judgment when prescribing medications to older adults.
The Beers Criteria and the STOPP/START criteria are useful tools for medication reconciliation for older adults. However, neither tool is perfect, and healthcare professionals should use their clinical judgment when prescribing medications to older adults. They should also consider a person’s general health, all underlying medical conditions, or circumstances that may lead a healthcare provider to choose a specific medication. The choice of tool may depend on the healthcare setting, the patient population, and the healthcare professional’s familiarity with the tool.
Serotonin syndrome is a potentially life-threatening condition that can occur when a patient takes medications that increase serotonin levels in the brain. Some common medications that can cause serotonin syndrome include:
Other medication-induced syndromes that can hasten death or increase discomfort during the dying process include:
Healthcare professionals should be aware of these medication-induced syndromes and take steps to prevent them in hospice patients.
In conclusion, medication reconciliation is a crucial process in hospice care that can help prevent medication errors, reduce the risk of adverse drug reactions, and improve patient outcomes. Healthcare professionals should perform medication reconciliation at several points during a patient’s hospice care and be familiar with the Beers Criteria and STOPP/START criteria. They should also be aware of common medications that can cause serotonin syndrome and other medication-induced syndromes that can hasten death or increase discomfort during the dying process.
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Patient Safety and Quality: An Evidence-Based Handbook for Nurses: Medication Reconciliation
The Role of the Nurse in the Management of Medicines During Transitional Care: A Systematic Review
Inappropriate Medication in the Geriatric Population
Understanding the Beers Criteria Is Essential
Beers Criteria for Potentially Inappropriate Medication Use in Older Adults
Medication Reconciliation Victory After an Avoidable Error
The basics of the STOPP/START criteria
Implementing the STOPP/START criteria to prevent polypharmacy in older adults
Explicit criteria as clinical tools to minimize inappropriate medication use and its consequences
Designing the Medication Reconciliation Process
Medication Reconciliation | PSNet
Overcoming the pitfalls of medication reconciliation
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death