Category: Ethics
Articles about end-of-life ethical issues including ethical dilemmas
Articles about end-of-life ethical issues including ethical dilemmas

End-of-life doulas are transforming hospice care quality through specialized training and collaborative partnerships. Learn how these compassionate professionals enhance patient experiences, support families, and improve hospice satisfaction scores when properly integrated into care teams.

Dialysis is a choice, not a requirement for end-stage kidney disease. While this life support treatment can extend life, it significantly impacts quality of life through fatigue, time constraints, and physical challenges. You have the right to choose comfort care and hospice instead. Learn why discussing dialysis preferences should be part of every living will and how end-of-life doulas can help navigate these important decisions.

A terminal diagnosis sends shockwaves through the lives of patients and their loved ones. This article delves into the trauma experienced by all involved, examining the intricate challenges faced by hospice and palliative care providers in offering compassionate support while navigating the complex emotional landscape of end-of-life care.

Nursing students' fear of death significantly impacts their readiness for hospice care, affecting the quality of end-of-life services. With severe staffing shortages and insufficient mentorship, new nurses enter hospice unprepared. End-of-life doula education through programs like death doula schools provides crucial solutions.

Delve into the complexities of potentially inappropriate medications (PIMs) for older adults, especially those in hospice and palliative care. This comprehensive guide explores identification, risks, and alternatives to PIMs, providing valuable insights for healthcare professionals to enhance medication safety and quality of life for geriatric patients.

Every year, thousands die in emergency departments unprepared for death. Sudden death in hospitals can be especially shocking for patients and families who haven't planned ahead. This guide highlights why preparation is important and describes how end-of-life doulas can assist.

If you're 18 or older without an advance directive, you're putting yourself and your loved ones at risk. This comprehensive guide explains why every adult—regardless of age—should prioritize creating a thorough living will reviewed every 3-6 months, and how end-of-life doulas can help.

Discover how CaringBridge helps families and end-of-life doulas stay connected during health journeys. This free platform offers privacy controls, easy updates, and community support for chronic illness, terminal illness, and life transitions.
Primary caregivers often face difficult emotions of isolation when loved ones step back during a chronic or terminal illness. This article thoughtfully addresses these feelings, delves into the reasons for this distance, and provides constructive communication strategies to foster reconnection with hesitant family members. It also highlights alternative support avenues for caregivers, ensuring they feel valued and supported.
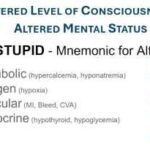
Discover essential techniques for hospice and palliative care nurses to identify subtle changes in patients' level of consciousness. This comprehensive guide covers assessment methods, red flags, and best practices for enhancing patient care—valuable insights for neurological nursing specialists and those aspiring to specialize in this field.
Ambiguous loss is a type of grief that happens when loss feels unclear or unfinished. Unlike traditional grief, this emotional pain lacks closure, making it harder to process. Learn to recognize the signs of ambiguous loss and discover practical healing strategies to help you move forward with hope.
Conflict happens in every relationship and setting. This practical guide teaches a proven 7-step approach developed by conflict resolution experts to recognize, prevent, and resolve disagreements compassionately. Learn essential de-escalation tools for better communication and stronger relationships.

When a family can't accept that their loved one is dying, it creates additional stress during an already challenging time. This article offers guidance on communicating with denial, supporting the patient, managing family dynamics, and finding professional help. Learn practical strategies to navigate this sensitive situation with compassion and understanding.

Caring for a terminally ill loved one at home is an incredibly challenging and emotional journey for family caregivers. This guide acknowledges the struggles you may face and offers compassionate solutions. It explores valuable resources, such as end-of-life doulas, PACE programs, and professional home care services, all designed to help ease your burden and provide support during this difficult time. You are not alone in this experience; there are ways to find relief and comfort as you navigate these profound challenges.
This comprehensive guide helps patients, families, and healthcare professionals confidently navigate POLST decisions. Learn the essential steps, understand your options, and ensure your end-of-life care wishes are honored through proper planning and communication.

This article delves into Utilization Behavior in dementia, offering practical advice for families and caregivers to create a safe environment and mitigate the challenges associated with this condition.

Discover the essentials of hiring caregivers for terminally ill patients. This guide covers caregiver qualifications, assessing understanding of terminal care, and practical hiring tips.
This comprehensive guide provides valuable insights on how to report and prevent elderly abuse in nursing homes. It serves as a resource for families, guardians, and loved ones to understand their roles and responsibilities in advocating for the elderly. Learn how to empower yourself and ensure the safety and well-being of your loved ones.
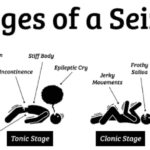
We understand that caring for a loved one in hospice can be a journey filled with compassion, love, and sometimes, uncertainty. When seizures are part of this journey, it’s natural to have concerns and questions. This guide is here to walk alongside you, offering knowledge and support as you navigate the complexities of seizure management in hospice settings.

Explore how extended hospice care for dementia patients benefits families and saves Medicare money despite regulatory challenges around six-month prognosis rules.

This guide helps families of terminally ill patients comprehend absolute vs. relative risk reduction. It’s a resource for making educated choices about medication continuation, tapering, or cessation in collaboration with healthcare professionals.

This article delves into the intricate dynamics of hospice nurses’ relationships with patients, examining the benefits and challenges of emotional investment versus professional detachment.

This article delves into the challenges faced by family caregivers in hospice and palliative care, offering practical strategies and resources to support them in their indispensable roles.
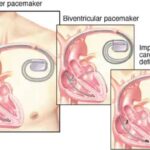
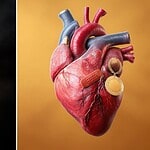
Learn about the differences between pacemakers and ICDs, their functions, and the implications for patients and caregivers. Discover why pacemakers should stay on, and ICDs should be turned off at the end of life for comfort and dignity.