Introduction
Overview of Palliative Sedation
Palliative sedation is a medical treatment used at the end of life to help patients who are experiencing severe symptoms that cannot be controlled with other therapies. It involves giving medications to make a patient relaxed and sleepy, reducing their awareness of distressing symptoms like pain, nausea, or difficulty breathing. The goal is to relieve suffering and ensure patients are comfortable in their final days or hours.
Importance of Comfort at End-of-Life
When someone nears the end of their life, comfort becomes the most essential part of their care. Being comfortable means that the person is not in pain, feeling anxious, or struggling to breathe. For many terminally ill patients, the last days and hours can be very challenging. Symptoms can become severe and complex to manage. By focusing on comfort, we can ensure that the person’s remaining time is as peaceful and pain-free as possible. This also helps their family and loved ones, providing them peace and ensuring their loved one is not suffering.
Purpose of the Article
This article aims to provide a comprehensive guide on palliative sedation for hospice nurses, caregivers, family members, and terminally ill patients. It will cover:
- What is palliative sedation, and how does it differ from other end-of-life care options?
- The ethical dilemmas that come with palliative sedation.
- How to know when it’s the right time to start palliative sedation.
- Recommended medication regimens that have worked well in the past.
- What nurses, caregivers, and family members should monitor to ensure palliative sedation is effective.
- Steps to take if palliative sedation is not working as planned.
By the end of this article, you will better understand palliative sedation, which will help you make informed decisions and provide compassionate care for your loved one or patient during their end-of-life journey.
Understanding Palliative Sedation
Definition and Purpose
Palliative sedation is a medical treatment used to help patients who are experiencing severe, uncontrollable symptoms at the end of their life. These symptoms can include extreme pain, constant nausea and vomiting, or severe difficulty breathing. When other treatments fail to improve these symptoms, palliative sedation can make the patient more comfortable.
The purpose of palliative sedation is to reduce a patient’s awareness of their suffering by using medications to make them tired or sleep. The goal is not to hasten death but to ensure that the patient’s final days or hours are as peaceful and pain-free as possible. This can relieve the patient, their family, and caregivers who want to see their loved one comfortable.
Differences between Palliative Sedation and Euthanasia
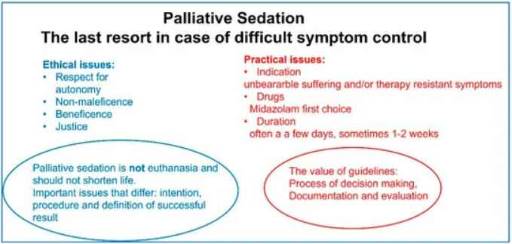
Palliative sedation and euthanasia are different in meaningful ways, and it’s crucial to understand these differences.
Palliative Sedation:
- Goal: The main goal is to relieve suffering by reducing the patient’s awareness of distressing symptoms.
- Process: Medications are given to make the patient sleepy or unconscious but not to cause death. The intent is to keep the patient comfortable until they pass away naturally.
- Ethical Consideration: Palliative sedation is ethically acceptable because it focuses on comfort, not ending life. The primary aim is to relieve unbearable suffering while respecting the natural dying process.
Euthanasia:
- Goal: The main goal is to end a person’s life to relieve suffering intentionally.
- Process: Medications are explicitly given to cause death.
- Ethical Consideration: Euthanasia is a much more controversial practice and is illegal in many places. It involves actively taking steps to end a person’s life, which raises complex ethical and legal questions.
In summary, palliative sedation is about making sure a terminally ill patient is comfortable and free from severe distress in their final moments, while euthanasia involves intentionally ending a life to stop suffering. Understanding these differences helps ensure that care decisions are made compassionately and per the patient’s and family’s wishes.
Ethical Dilemmas
Ethical Considerations
When considering palliative sedation, the ethical issues involved must be considered. Ethical considerations help ensure the decisions are respectful and compassionate toward the patient’s needs and wishes.
One of the primary ethical considerations is the intention behind using palliative sedation. The goal should always be to relieve unbearable suffering, not to hasten death. This focus on comfort is what makes palliative sedation different from euthanasia.
Another ethical consideration is fairness. All patients who need relief from severe symptoms should have access to palliative sedation if it’s appropriate for their situation. Decisions should be based on the patient’s needs, not on other factors like their background or financial situation.
Balancing Comfort and Consciousness
Balancing comfort and consciousness is a delicate part of palliative sedation. The aim is to reduce patient’s suffering while keeping them as comfortable as possible. This often means using just enough medication to make the patient comfortable but not so much that the patient is entirely unconscious if that’s not necessary.
Maintaining consciousness can be necessary for the patient and their family. It allows patients to communicate and interact with their loved ones, which can be meaningful in their final days or hours of life. However, if symptoms are too severe, more profound sedation may be necessary to relieve suffering. Finding this balance is crucial and requires careful consideration and ongoing assessment by healthcare professionals.
Family and Patient Consent
Getting consent from both the patient (if possible) and their family is a crucial step in the process of palliative sedation. Consent ensures that everyone involved understands and agrees with the plan to use palliative sedation.
This means discussing the options available for the patient and explaining how palliative sedation works, what it aims to achieve, and what it might feel like. Talking with their family or legal guardians is essential if the patient cannot consent.
Family members need to understand the purpose and process of palliative sedation as well. They should be allowed to ask questions and express their concerns. This helps ensure they are comfortable with the decision and understand that the primary goal is relieving the patient’s suffering.
Respecting the wishes of both the patient and their family is essential. If a patient has expressed wishes about their end-of-life care in advance, they should be honored as much as possible. Clear communication and compassionate support during these discussions can help everyone involved feel more at peace with the decision.
In summary, ethical dilemmas in palliative sedation involve careful consideration of intentions, fairness, the balance between comfort and consciousness, and obtaining informed consent from the patient and family. These considerations help ensure that palliative sedation is used appropriately and compassionately to relieve suffering at the end of life.
Indications for Palliative Sedation
Symptoms Indicating the Need for Palliative Sedation
Palliative sedation is considered when a terminally ill patient experiences symptoms that are so severe and distressing that other treatments can’t provide relief. Here are some of the primary symptoms that might indicate the need for palliative sedation:
Intractable or Fear of Air Hunger
Air hunger is an intense feeling of breathlessness or difficulty breathing. This can be extremely frightening and uncomfortable for patients. When air hunger cannot be relieved by medications like oxygen or other treatments, palliative sedation may be necessary to ease this sensation. Sometimes, just the fear of experiencing severe breathlessness in the future can cause significant anxiety, making sedation a compassionate option.
Intractable Nausea and Vomiting
Nausea and vomiting that do not respond to conventional treatments can make a patient’s final days very distressing. Constant nausea prevents patients from eating, drinking, or sleeping comfortably. If medications and other interventions fail to control these symptoms, palliative sedation can help to provide much-needed relief, allowing the patient to rest peacefully.
Intractable or Great Concern for Unmanaged Pain
Severe pain is one of the most common reasons for considering palliative sedation. When pain is so intense that it cannot be controlled with strong painkillers or other therapies, sedation may be the only way to ensure the patient’s comfort. Even the anticipation or great concern of experiencing unbearable pain can justify the use of palliative sedation if it causes significant anxiety and distress.
Intractable Terminal Restlessness and Agitation
Terminal restlessness and agitation refer to a state of severe anxiety, confusion, or agitation that some patients experience as they near the end of life. Physical discomfort, metabolic imbalances, or the progression of the disease itself can cause this. When these symptoms are uncontrollable and cause significant suffering, palliative sedation can help to calm and comfort the patient.
Emotional Distress
Sometimes, even when physical symptoms like pain, nausea, or difficulty breathing are well-managed, a patient might still experience severe emotional distress. This emotional distress can be just as troubling and overwhelming as physical pain. It may include feelings of extreme anxiety, depression, hopelessness, or fear of dying. In such cases, the patient’s mental and emotional suffering can significantly impact their quality of life, making it hard for them to find peace and comfort in their final days.
Assessing Emotional and Psychological Needs
It’s essential to assess the emotional and psychological needs of terminally ill patients regularly. This assessment can help determine the severity of their distress and identify the best ways to support them. Here are some steps to follow:
- Open Communication:
- Encourage patients to talk about their feelings and fears. Create a safe and supportive environment where they feel comfortable expressing themselves.
- Ask open-ended questions like, “How are you feeling today?” or “What are your biggest concerns right now?”
- Observing Behavior:
- Look for signs of emotional distress, such as crying, withdrawal, anger, or expressions of hopelessness.
- Take note if the patient seems more anxious, restless, or unable to find comfort in activities that previously brought them joy.
- Use Assessment Tools:
- Utilize standardized tools and questionnaires designed to measure anxiety, depression, and overall emotional well-being. These tools can provide a clearer picture of the patient’s emotional state.
- Involve Professionals:
- Collaborate with psychologists, psychiatrists, or counselors who specialize in palliative care. They can provide expert evaluations and suggest appropriate interventions.
- Family Involvement:
- Talk with family members to understand changes in the patient’s behavior and mood. They can offer valuable insights and support.
Requests from Patients or Power of Attorney for Palliative Sedation
When a patient or their power of attorney (POA) requests palliative sedation due to severe emotional distress, it’s crucial to approach the situation with sensitivity and empathy. Here’s how to handle such requests:
- Listen and Validate:
- Listen carefully to the patient’s or POA’s concerns and validate their feelings. Let them know that their emotional suffering is taken seriously and that you are there to help.
- Explore Alternatives:
- Before considering palliative sedation, explore other interventions that might alleviate emotional distress. These can include counseling, medications for anxiety or depression, spiritual support, and relaxation techniques.
- Discuss Palliative Sedation:
- If other methods are not effective and the distress is unbearable, discuss palliative sedation as a possible option. Explain what it involves, how it works, and what to expect.
- Ensure that the patient or POA understands that palliative sedation aims to relieve suffering by reducing consciousness, not to hasten death.
- Informed Consent:
- Obtain informed consent from the patient or POA. Make sure they understand the potential benefits and risks and that they are making an informed decision.
- Multidisciplinary Review:
- Consult with the healthcare team, including doctors, nurses, social workers, and chaplains, to review the case and ensure that palliative sedation is the most appropriate option for the patient’s needs.
- Ongoing Support:
- Please continue to provide emotional support to the patient and their family. Keep the lines of communication open and offer reassurance that their comfort and dignity are your top priorities.
By addressing emotional distress with compassion and thorough assessment, healthcare providers can help ensure that patients receive the best care, even when facing severe emotional challenges. When palliative sedation is deemed necessary, it should be approached thoughtfully and ethically, prioritizing the patient’s comfort and well-being.
Assessing Patient Needs and Desires
Before starting palliative sedation, assessing the patient’s needs and desires is crucial. This involves:
- Listening to the patient: Their input is vital if the patient can communicate. They should be asked about their symptoms, fears, and what they hope to achieve through sedation.
- Talking to the family: Family members can provide valuable insights into the patient’s condition, their wishes, and any advance directives or previously expressed preferences.
- Medical evaluation: Healthcare providers should conduct a comprehensive assessment to understand the severity of the symptoms and confirm that all other treatment options have been tried and found ineffective.
This thorough assessment ensures that palliative sedation is used appropriately and aligns with the patient’s values and wishes.
Clinical Guidelines
Healthcare providers follow specific clinical guidelines to ensure palliative sedation is used safely and effectively. These guidelines include:
- Eligibility: Confirm that the patient’s symptoms are intractable and cannot be managed with other treatments.
- Consent: Obtaining informed consent from the patient (if possible) or their legal representatives.
- Medication Selection: Choosing the appropriate medications for sedation. Common choices include benzodiazepines, barbiturates, and antipsychotics.
- Monitoring: Regularly monitor the patient to ensure the sedation is effective and adjust the dosage as needed.
- Communication: Maintaining open lines of communication with the patient’s family, keeping them informed about the patient’s condition and the sedation process.
- Documentation: Thoroughly documenting the decision-making process, the consent obtained, the medications used, and the patient’s response.
By following these guidelines, healthcare providers can ensure that palliative sedation is administered ethically, compassionately, and focused on relieving the patient’s suffering.
In summary, palliative sedation is indicated for severe, uncontrollable symptoms such as air hunger, nausea and vomiting, pain, and terminal restlessness. Assessing the patient’s needs and desires and following clinical guidelines ensures that this approach is used thoughtfully and effectively to provide comfort at the end of life.
Initiating Palliative Sedation
When to Start
Deciding when to start palliative sedation is a critical and sensitive decision that requires careful consideration. Palliative sedation should be considered when:
- Symptoms are unbearable: The patient is experiencing severe symptoms such as intense pain, constant nausea, uncontrollable vomiting, severe breathlessness, or terminal restlessness and agitation that cannot be managed with other treatments.
- All other treatments have failed: Before starting palliative sedation, healthcare providers should have tried all other possible treatments and found them ineffective in relieving the patient’s symptoms.
- The patient’s quality of life is severely affected: When the patient’s quality of life is severely compromised and they are suffering despite all available interventions, it might be time to consider palliative sedation.
Starting palliative sedation is a step taken to ensure the patient’s final moments are as peaceful and pain-free as possible. It’s crucial to involve the patient (if possible) and their family in the decision-making process to ensure that their wishes and concerns are addressed.
Pre-sedation Assessments
Before beginning palliative sedation, several assessments should be completed to ensure it is the appropriate course of action:
- Symptom Assessment: Conduct a thorough evaluation of the patient’s symptoms to confirm that they are severe, intractable, and causing significant distress.
- Medical History Review: Review the patient’s medical history, current medications, and any previous interventions attempted to manage symptoms. This helps understand why other treatments may have failed and ensures no overlooked options exist.
- Patient and Family Preferences: Discuss the patient’s wishes, values, and goals for end-of-life care. If the patient cannot communicate, talk to their family or legal representatives to understand the patient’s previously expressed desires or advance directives.
- Ethical and Legal Considerations: Ensure that the use of palliative sedation aligns with ethical guidelines and legal requirements. This includes obtaining informed consent from the patient or their legal representative.
- Team Consultation: Involve the healthcare team, including doctors, nurses, and palliative care specialists, in the assessment and decision-making process. This collaborative approach ensures that all aspects of patient care are considered.
Communication with Family and Caregivers
Effective and compassionate communication with the patient’s family and caregivers is crucial when initiating palliative sedation. Here’s how to approach these conversations:
- Explain the Process: Clearly explain palliative sedation, why it is being considered, and how it will be administered. Describe the goal of relieving the patient’s suffering and ensuring their comfort.
- Address Concerns: Listen to any concerns or fears the family or caregivers may have. Provide honest and straightforward answers to their questions. Reassure them that the primary aim is to make the patient comfortable.
- Discuss Expectations: Help the family understand what to expect during palliative sedation. This includes explaining how the patient may appear, how long the sedation may last, and the expected outcomes.
- Obtain Consent: Ensure informed consent is obtained from the patient (if possible) or their legal representative. This consent should include an understanding of the reasons for sedation, the medications to be used, and the potential effects.
- Provide Ongoing Support: Continue to offer emotional support and information throughout the process. Keep the family and caregivers updated on the patient’s condition and any adjustments made to the sedation plan.
- Encourage Presence: Encourage family members and caregivers to be present and spend time with the patient, even if the patient is sedated. Their presence can comfort and reassure both the patient and themselves.
By starting palliative sedation at the right time, conducting thorough pre-sedation assessments, and communicating effectively with family and caregivers, healthcare providers can ensure that the process is handled with compassion and respect for the patient’s dignity and comfort.
Medication Regimens
Common Medications Used
Palliative sedation involves the use of medications that help reduce a patient’s awareness of severe symptoms, making them more comfortable in their final days or hours. While morphine concentrates can work, and I’ve used it three times with success alongside Lorazepam and Haloperidol, here are some common types of medicines used in palliative sedation nationwide:
Benzodiazepines
Benzodiazepines are a group of medications that help reduce anxiety, relax muscles, and induce sleep. They are often used in palliative sedation because they can calm the patient and relieve symptoms like severe anxiety and agitation.
- Examples: Midazolam, Lorazepam, Diazepam
- How They Work: These medications enhance the effect of a neurotransmitter in the brain called GABA, which promotes relaxation and reduces activity in the nervous system.
Barbiturates
Barbiturates are another class of medications used for sedation. They are potent sedatives that can help make the patient unconscious or deeply asleep, which helps relieve severe symptoms.
- Examples: Phenobarbital, Pentobarbital
- How They Work: Barbiturates depress the central nervous system, leading to sedation and unconsciousness.
Antipsychotics
Antipsychotics are sometimes used in palliative sedation to control symptoms like severe agitation, delirium, and terminal restlessness. They can help calm the patient and provide a more peaceful state.
- Examples: Haloperidol, Chlorpromazine
- How They Work: These medications affect neurotransmitters in the brain, helping to stabilize mood and reduce severe agitation.
Dosage Guidelines
The dosage of these medications can vary based on the patient’s needs, weight, age, and overall health. Healthcare providers must start with the lowest effective dose and adjust as needed. Here are some general guidelines:
- Benzodiazepines:
- Midazolam is often started at 1-2 mg/hour and adjusted based on the patient’s response.
- Lorazepam: The initial dose might be 1-2 mg every few hours as needed, with adjustments for continuous infusion if necessary.
- Barbiturates:
- Phenobarbital: The starting dose might be around 60-120 mg, followed by additional doses every 30 minutes until desired sedation is achieved, then maintenance doses as needed.
- Pentobarbital: Initial doses can vary but are usually given as a continuous infusion to maintain sedation.
- Antipsychotics:
- Haloperidol: The initial dose might be 0.5-2 mg, with repeated doses every few hours as needed.
- Chlorpromazine: The starting dose might be 25-50 mg every 6-8 hours, with adjustments based on the patient’s response.
Administration Methods
The method of administering these medications can also vary. Here are the standard methods used:
- Oral (PO): The simplest method is to take the medication by mouth, but it may not be suitable if the patient has difficulty swallowing or is experiencing severe nausea and vomiting.
- Subcutaneous (SubQ): Medications can be injected under the skin. This method is often used for continuous infusions and is less invasive than intravenous administration.
- Intravenous (IV): Administering medications directly into the vein provides rapid relief and is useful for patients needing immediate symptom control. This method is commonly used for continuous infusions of medications like Midazolam or Phenobarbital.
- Rectal: In some cases, medications can be administered rectally if other methods are not feasible. This method can be helpful for patients who cannot swallow or have obstructed gastrointestinal tracts.
By carefully selecting the appropriate medications, adjusting dosages based on the patient’s response, and choosing the proper administration method, healthcare providers can effectively manage severe symptoms and provide comfort through palliative sedation. This approach ensures that the patient’s final moments are as peaceful and pain-free as possible, honoring their dignity and relieving the patient and their loved ones.
Monitoring Effectiveness
Signs that Palliative Sedation is Working
When palliative sedation is used, it’s crucial to monitor the patient to ensure that it is effective and that the patient is comfortable. Here are signs that palliative sedation is working:
- Reduced Awareness of Symptoms: The patient appears unaware of pain, discomfort, or other distressing symptoms. They are less responsive to external stimuli, indicating that the medication relieves them.
- Calm and Relaxed Appearance: The patient looks peaceful and relaxed. There is no evidence of agitation, restlessness, or distress. They may be sleeping quietly and deeply.
- Stable Vital Signs: The patient’s vital signs, such as heart rate, blood pressure, and respiratory rate, are stable and comfortable. Extreme fluctuations can indicate discomfort or distress.
- Positive Feedback from Family: Family members notice and report that the patient appears more comfortable and at peace. Their observations are valuable in assessing the patient’s condition.
Regular Assessments and Adjustments
Continuous monitoring and assessment are crucial to ensure that palliative sedation remains effective. Here’s how healthcare providers can manage this:
- Frequent Check-ins: Regularly check the patient’s vital signs, level of sedation, and overall comfort. Based on the patient’s condition, this should be done every few hours or as needed.
- Adjusting Dosages: Based on the assessments, the dosage of the sedative medication may need to be adjusted. The dosage can be increased if the patient shows signs of discomfort or increased awareness of symptoms. Conversely, if the patient is too profoundly sedated, the dosage can be decreased to maintain the appropriate level of comfort.
- Collaborative Approach: The healthcare team, including doctors, nurses, and palliative care specialists, should work together to assess the patient’s condition and make any necessary adjustments. This team approach ensures comprehensive care.
- Communication with Family: Inform the patient’s family about the patient’s condition and any adjustments made to the sedation regimen. This helps maintain trust and reassures them that their loved one is cared for compassionately.
Managing Side Effects
While palliative sedation aims to make the patient comfortable, it can sometimes cause side effects. It’s important to identify and manage these side effects promptly:
- Respiratory Depression: Sedative medications can slow down breathing. Monitoring the patient’s respiratory rate is crucial. If breathing becomes too slow or shallow, the dosage may need to be adjusted, or additional interventions might be required.
- Excessive Sedation: If the patient is too deeply sedated, they might not respond at all to external stimuli. The goal is to achieve a level of sedation that relieves suffering without eliminating responsiveness unless it is necessary for comfort. Adjusting the medication dosage can help balance this.
- Cardiovascular Effects: Some sedative medications can affect heart rate and blood pressure. Regular monitoring ensures that any significant changes can be addressed quickly. This may involve adjusting the sedative dose or adding medications to manage these effects.
- Skin and Comfort Issues: Patients sedated for extended periods may be at risk for skin breakdown or bedsores. Regularly repositioning the patient and using special mattresses can help prevent these issues.
- Gastrointestinal Issues: Sedation can sometimes lead to constipation or other gastrointestinal problems. Ensuring proper hydration and using medications to manage these symptoms can help keep the patient comfortable.
By carefully monitoring the effectiveness of palliative sedation and being vigilant about managing side effects, healthcare providers can ensure patients remain comfortable and free from distress. This approach focuses on the physical aspects of care and provides emotional support to the patient’s family, reinforcing that their loved one is cared for with compassion and respect.
Troubleshooting and Adjustments
What to Do if Sedation is Not Effective
Sometimes, despite the best efforts, palliative sedation may not initially work as intended. Here are steps to take if sedation is not effective:
- Reassess the Patient: Conduct a thorough reassessment of the patient’s symptoms and overall condition. Check for any changes that might have occurred since the sedation was started.
- Review Medication Dosages: Ensure that the dosages are appropriate for the patient’s level of discomfort. If the current medication is not providing adequate relief, increase the dosage or switch to a different one.
- Check for Underlying Issues: Look for any underlying issues affecting sedation’s effectiveness. This can include factors like metabolic imbalances, infections, or other medical conditions that must be addressed.
- Consult the Healthcare Team: Discuss the situation with the healthcare team, including doctors, nurses, and palliative care specialists. They can provide insights and recommendations for adjusting the treatment plan.
- Adjust the Sedation Plan: Based on the reassessment and team consultation, make necessary adjustments to the sedation plan. This might involve changing the type of medication, adjusting the dosage, or modifying the administration method.
Alternative Approaches
If standard palliative sedation is not adequate, there are alternative approaches that can be considered:
- Combination Therapy: Sometimes, a combination of medications can be more effective than a single drug. This might involve combining sedatives with pain relievers or other symptom management medications.
- Non-Pharmacological Methods: Integrating non-pharmacological methods can enhance the effectiveness of palliative sedation. These methods can include:
- Comfort Measures: Ensure the patient is comfortable, use soft bedding, and maintain a calm environment.
- Relaxation Techniques: Gentle music, aromatherapy, or soft lighting can help create a soothing atmosphere.
- Emotional Support: Emotional support and reassurance can significantly impact the patient’s comfort level. Family presence and a gentle touch can be very comforting.
- Advanced Sedation Techniques: In some cases, more advanced sedation techniques might be necessary. This could include using higher levels of sedation or specialized medications under close medical supervision.
- Hospice and Palliative Care Consultation: Engaging a palliative care specialist or a hospice care team can provide additional expertise and support. They can offer new perspectives and strategies for managing complex symptoms.
Support for Caregivers and Family Members
Supporting caregivers and family members is crucial when palliative sedation is used. Here’s how to provide this support:
- Provide Clear Information: Keep family members informed about the patient’s condition and the purpose of palliative sedation. Explain how the medications work and what to expect.
- Encourage Open Communication: Allow family members to express their concerns and ask questions. Listen actively and provide honest, compassionate answers.
- Offer Emotional Support: Recognize this is a difficult time for family members. Offer emotional support through regular check-ins, counseling services, or support groups. Sometimes, just being there to listen can make a big difference.
- Involve Them in Care: Encourage family members to participate in caring for their loved one if they feel comfortable. This can include simple tasks like holding the patient’s hand, talking to them, or helping with comfort measures.
- Respect Their Wishes: Respect the wishes and cultural beliefs of the family. This includes honoring any specific rituals or practices they want to observe during this time.
- Prepare for the End: Help family members prepare for the end-of-life process. Guide what to expect as the patient’s condition changes and offer resources for coping with grief and loss.
By taking these steps, healthcare providers can ensure that patients and their families receive compassionate and comprehensive care during palliative sedation. This holistic approach helps maintain dignity and comfort for the patient while offering essential support to those who love them.
Legal and Regulatory Considerations
Legal Framework in the United States
Palliative sedation is a medically accepted practice in the United States, but it is governed by specific legal and regulatory guidelines to ensure it is used appropriately and ethically. Understanding these guidelines is crucial for healthcare providers, caregivers, and family members.
Key Legal Principles
- Distinction from Euthanasia: Palliative sedation is legally distinct from euthanasia. While euthanasia involves actively ending a patient’s life, palliative sedation aims to alleviate suffering by reducing consciousness. The primary intent is comfort, not hastening death.
- Informed Consent: Obtaining informed consent is a legal requirement. This means that the patient (if capable) or their legal representative must fully understand the nature of palliative sedation, its purpose, potential risks, and benefits before agreeing to it.
- Best Interest of the Patient: Decisions about palliative sedation must be made with the patient’s best interest in mind. This includes considering their wishes, values, and quality of life.
- Medical Necessity: Palliative sedation should be considered a last resort when other treatments have failed to effectively manage severe symptoms.
Documentation and Reporting
Proper documentation and reporting are essential components of administering palliative sedation. This helps ensure legal compliance and provides a clear record of care decisions.
Essential Documentation Elements
- Patient Assessment: Detailed records of the patient’s symptoms, medical history, and previous treatments. This should include the severity and intractability of symptoms leading to the decision for palliative sedation.
- Informed Consent: Documentation of the informed consent process, including discussions with the patient or their legal representative. This should detail what was explained about palliative sedation and any questions or concerns raised.
- Sedation Plan: A clear plan outlining the medications, dosages, administration methods, and monitoring protocols. This should also include criteria for adjusting the sedation levels.
- Monitoring Records: Continuous documentation of the patient’s condition during sedation. This includes vital signs, level of consciousness, and any side effects or complications observed.
- Family Communication: Records of conversations with family members, including their understanding and agreement with the sedation plan. This helps ensure transparency and supports the family’s emotional needs.
- Team Consultations: Notes on discussions with the healthcare team, including input from doctors, nurses, and palliative care specialists. This collaborative approach ensures comprehensive care.
Patient Rights
Patients have specific rights regarding palliative sedation; respecting these rights is fundamental to providing compassionate and ethical care.
Key Patient Rights
- Right to Comfort: Patients have the right to be free from severe pain and suffering. Palliative sedation is a means to ensure this comfort at the end of life.
- Right to Informed Consent: Patients (or their legal representatives) can receive all relevant information about their treatment options, including the risks and benefits of palliative sedation, before consenting.
- Right to Participate in Decision-Making: Patients should be involved in decisions about their care as much as possible. This includes having their wishes and preferences respected regarding the use of palliative sedation.
- Right to Dignity: Patients have the right to die with dignity. Palliative sedation can help ensure that the end-of-life experience is peaceful and respectful.
- Right to Privacy: Patients’ medical information and the details of their care should be kept confidential. Only those directly involved in the patient’s care should have access to this information.
- Right to Compassionate Care: Patients and their families can receive compassionate and empathetic care from healthcare providers. This includes emotional support and clear communication throughout the process.
Understanding palliative sedation’s legal and regulatory considerations is crucial for ensuring its ethical and effective use. By adhering to the legal framework, maintaining thorough documentation, and respecting patient rights, healthcare providers can ensure that palliative sedation is administered to prioritize patients’ comfort and dignity while supporting their families during a challenging time.
Support for Nurses, Caregivers, and Families
Emotional Support Strategies
Providing care for a terminally ill loved one or patient can be emotionally draining. It’s essential to have strategies to manage these emotions and support each other through the process.
For Nurses and Caregivers
- Self-Care: Self-care is essential. This includes eating well, getting enough sleep, and taking breaks. Make time for relaxing and rejuvenating activities like reading, walking, or listening to music.
- Seek Professional Support: Talking to a counselor or joining a support group can provide a safe space to express your feelings and receive emotional support. Many organizations offer support services specifically for healthcare providers.
- Mindfulness and Relaxation Techniques: Meditation, deep breathing exercises, and yoga can help reduce stress and improve emotional well-being. Practicing mindfulness for a few minutes each day can make a big difference.
- Peer Support: It can be very comforting to connect with colleagues who are going through similar experiences. Share your feelings, experiences, and coping strategies with each other.
For Families
- Emotional Expression: Encourage family members to discuss their feelings and share their experiences. Bottling up emotions can lead to increased stress and anxiety. Open, honest communication can be very healing.
- Spend Time Together: Spending quality time together can comfort and strengthen family bonds. Engage in activities that everyone enjoys and create positive memories.
- Accept Help: Don’t be afraid to accept help from friends, extended family, or community organizations. Practical help with chores, meals, or caregiving tasks can lighten your load and provide much-needed relief.
- Remember to Grieve: It’s natural to feel grief and sadness during this time. Allow yourself to grieve and seek support from others who understand what you are going through. Grieving is a healthy part of the process and can help you cope better in the long run.
Resources and Training
Access to the right resources and training can significantly improve the quality of care and emotional stress management.
For Nurses
- Continuing Education: Regular training and palliative and end-of-life care workshops can enhance your skills and knowledge. Many organizations offer online courses and certifications in palliative care.
- Clinical Guidelines: Familiarize yourself with clinical guidelines and best practices for palliative sedation and symptom management. These guidelines can provide a framework for making informed decisions and delivering high-quality care.
- Support Networks: Join professional organizations and networks focusing on palliative and hospice care. These networks often provide valuable resources, discussion forums, and professional development opportunities.
For Families and Caregivers
- Educational Materials: Many hospices and palliative care organizations provide educational materials and guides on end-of-life care. These can help you understand what to expect and how to manage various aspects of caregiving.
- Workshops and Support Groups: Participating in workshops and support groups can provide practical tips and emotional support. These groups often offer a safe space to share experiences and learn from others.
- Online Resources: Numerous websites and online communities are dedicated to hospice and palliative care. These resources can offer information, support, and connections to other caregivers and families.
Communicating with Healthcare Providers
Effective communication with healthcare providers is crucial for ensuring the best care for your loved one and managing stress and concerns.
- Be Honest and Open: Share all relevant information about the patient’s symptoms, preferences, and concerns. Don’t hesitate to ask questions or express any worries you may have.
- Schedule Regular Updates: Regularly scheduled meetings or calls with the healthcare team can inform you about the patient’s condition and care plan. This helps prevent misunderstandings and ensures everyone is on the same page.
- Clarify Roles and Responsibilities: Understanding who is responsible for different aspects of care can help avoid confusion and ensure that all needs are met. This includes knowing who to contact in case of an emergency or urgent question.
- Express Your Needs: Let the healthcare team know if you need more support or resources. They can often provide additional help or connect you with services that make your caregiving role more manageable.
- Document Important Information: Keep a notebook or digital record of essential conversations, instructions, and contact information. This can be a valuable reference and help ensure nothing important is overlooked.
By implementing these emotional support strategies, utilizing available resources and training, and maintaining open communication with healthcare providers, nurses, caregivers, and families can provide the best possible care for their loved ones and manage the emotional challenges of end-of-life care. This holistic approach helps ensure everyone feels supported and capable during this difficult time.
Case Studies
Case Study 1: Severe Pain and Palliative Sedation
Background: Mrs. Johnson, a 68-year-old woman with advanced pancreatic cancer, was admitted to hospice care. Despite aggressive pain management, she continued to experience excruciating pain that significantly impacted her quality of life.
Initial Assessment:
- Symptoms: Severe abdominal pain, unrelieved by high doses of opioids and other pain medications.
- Emotional State: Anxious and distressed due to constant pain.
- Family Concerns: Her family was deeply concerned about her suffering and sought alternative solutions to ease her pain.
Intervention: The hospice team decided to initiate palliative sedation to alleviate Mrs. Johnson’s suffering. After obtaining informed consent from Mrs. Johnson and her family, the team started her on a low dose of midazolam, a benzodiazepine known for its sedative properties.
Outcome:
- Initial Response: Mrs. Johnson’s pain significantly decreased, and she appeared more relaxed and comfortable.
- Monitoring: The hospice team closely monitored her vital signs and level of consciousness, adjusting the medication dosage as needed.
- Family Support: The family was regularly updated on her condition and felt reassured that she was no longer in pain.
Troubleshooting:
- Challenge: After 24 hours, Mrs. Johnson showed signs of restlessness and intermittent pain.
- Adjustment: The team slightly increased the midazolam dosage and added a low dose of haloperidol to address potential agitation.
- Final Outcome: Mrs. Johnson’s symptoms were effectively managed, and she remained comfortable until her peaceful passing a few days later.
Case Study 2: Emotional Distress and Request for Palliative Sedation
Background: Mr. Smith, a 75-year-old man with end-stage lung disease, was under hospice care. Although his physical symptoms were well-managed, he experienced severe emotional distress, including anxiety and a fear of suffocation.
Initial Assessment:
- Symptoms: Intense anxiety and fear, particularly at night, despite the absence of severe physical symptoms.
- Emotional State: He expressed feelings of hopelessness and a desire for relief from his emotional suffering.
- Family Concerns: His daughter, who held his power of attorney (POA), was deeply concerned about his mental state and requested palliative sedation.
Intervention: After a thorough assessment and discussion with the multidisciplinary team, the decision was made to proceed with palliative sedation. Mr. Smith and his daughter were informed about the process, and consent was obtained.
Outcome:
- Initial Response: A low dose of lorazepam, another benzodiazepine, was administered to help alleviate his anxiety.
- Monitoring: Regular assessments were conducted to monitor Mr. Smith’s emotional state and level of sedation.
- Family Support: The hospice team provided emotional support and regular updates to his daughter.
Troubleshooting:
- Challenge: Mr. Smith’s anxiety was not fully relieved after the initial dose.
- Adjustment: The team increased the lorazepam dose and added a small dose of phenobarbital to enhance the sedative effect.
- Final Outcome: Mr. Smith’s anxiety was significantly reduced, allowing him to experience a sense of peace in his final days. His daughter was grateful for the care provided and the relief it brought to her father.
Case Study 3: Intractable Nausea and Palliative Sedation
Background: Mrs. Martinez, a 62-year-old woman with advanced ovarian cancer, suffered from intractable nausea and vomiting. Despite various antiemetic medications, her symptoms persisted, severely affecting her quality of life.
Initial Assessment:
- Symptoms: Persistent nausea and vomiting, unrelieved by standard treatments.
- Emotional State: Mrs. Martinez was exhausted and expressed a desire for relief, even if it meant sedation.
- Family Concerns: Her husband and children were distressed by her suffering and supported her decision for palliative sedation.
Intervention: The hospice team discussed the option of palliative sedation with Mrs. Martinez and her family. After obtaining consent, they started her on a low dose of propofol, a sedative often used for severe symptoms.
Outcome:
- Initial Response: Mrs. Martinez’s nausea and vomiting decreased significantly, and she appeared more comfortable.
- Monitoring: Continuous monitoring was conducted to ensure her symptoms were managed and her sedation level was appropriate.
- Family Support: The family received regular updates and was encouraged to spend time with Mrs. Martinez, providing emotional support.
Troubleshooting:
- Challenge: Mrs. Martinez developed mild respiratory depression, a potential side effect of propofol.
- Adjustment: The team adjusted the propofol dosage and added antiemetic ondansetron to maintain symptom control while minimizing sedation.
- Final Outcome: Mrs. Martinez’s symptoms were well-managed, and she remained comfortable until she passed away peacefully surrounded by her family.
These case studies illustrate the compassionate application of palliative sedation in various scenarios. Each case required careful assessment, ethical consideration, and thoughtful adjustments to ensure the patient’s comfort and dignity. By sharing these stories, we hope to provide insights and guidance for hospice nurses, caregivers, families, and terminally ill patients facing similar challenges.
Conclusion
Recap of Key Points
In this article, we have explored the essential aspects of palliative sedation, a compassionate approach to alleviating severe symptoms in terminally ill patients. Here are the key points we covered:
- Understanding Palliative Sedation: It is a medical practice used to relieve unbearable suffering by reducing consciousness, distinct from euthanasia.
- Ethical Dilemmas: It involves careful consideration of the patient’s comfort, maintaining a balance between consciousness and relief from distress, and obtaining informed consent from the patient or their family.
- Indications for Palliative Sedation: It is considered for symptoms such as intractable air hunger, nausea and vomiting, unmanaged pain, and terminal restlessness when other treatments fail. Emotional distress — even in the light of all medical symptoms being managed — is also a type of extreme suffering that is an indication for palliative sedation if the patient or power of attorney is requesting this option of care.
- Initiating Palliative Sedation: This involves determining the right time to start, conducting pre-sedation assessments, and communicating clearly with family and caregivers.
- Medication Regimens: Common medications include benzodiazepines, barbiturates, and antipsychotics, with specific guidelines for dosage and administration.
- Monitoring Effectiveness: Regular assessments ensure the sedation works, adjusts as needed, and manage any side effects.
- Troubleshooting and Adjustments: If sedation is ineffective, consider reassessing the patient, reviewing medication, and exploring alternative approaches. Support for caregivers and family members is also essential.
- Legal and Regulatory Considerations: It is crucial to adhere to the legal framework, document, and report accurately, and respect patient rights.
- Support for Nurses, Caregivers, and Families: Emotional support strategies, access to resources and training, and effective communication with healthcare providers are critical to holistic care.
Encouragement for Compassionate Care
Providing care for a terminally ill loved one or patient is a profound responsibility that requires compassion, empathy, and dedication. Whether you are a nurse, caregiver, or family member, your efforts significantly impact the patient’s comfort and dignity. Remember to care for yourself, seek support, and take breaks when needed. Compassionate care alleviates physical symptoms and provides emotional and psychological support to the patient and their loved ones.
Final Thoughts on Palliative Sedation
Palliative sedation is a vital tool in end-of-life care, offering relief from unbearable suffering and ensuring that patients can spend their final moments in peace and comfort. While it comes with complex ethical and practical considerations, when used appropriately, it upholds the dignity and wishes of the patient.
For nurses and caregivers, it is essential to stay informed, communicate effectively, and approach each case with empathy and respect. Understanding and participating in the care process can bring peace and closure to families. By working together, we can ensure the end-of-life journey is as gentle and compassionate as possible.
In conclusion, palliative sedation is a compassionate practice aimed at relieving the most severe symptoms in terminally ill patients. It requires careful ethical consideration, precise medical management, and robust support systems for caregivers and families. By adhering to best practices and maintaining open communication, we can provide the highest quality of care, ensuring comfort and dignity for those at the end of life.
Resources
Palliative Sedation in the Home Setting
Does palliative sedation ease suffering during end-of-life care?
Palliative Sedation: Myth vs. Fact
Palliative sedation: A safety net for the relief of refractory and intolerable symptoms at the end of life
Palliative Sedation at the End of Life: Patterns of Use in an Israeli Hospice
Palliative Sedation—The Last Resort in Case of Difficult Symptom Control: A Narrative Review and Experiences from Palliative Care in Switzerland
Palliative Sedation in Patients With Terminal Illness
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Caregiver Support Book Series
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
The Caregiver’s Guide to Cancer: Compassionate Advice for Caring for You and Your Loved One (Caregiver’s Guides)
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Peace in the Face of Cancer
A Handbook of caring for someone with cancer: Instructions for the Support Person or Caregiver Helping a Loved One Survive Cancer
Co-Surviving Cancer: The Guide for Caregivers, Family Members and Friends of Adults Living with Cancer
Things I Wish I’d Known: Cancer Caregivers Speak Out
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
The Last Hours of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare