Navigating the Complex World of Dementia and Seizures
Published on May 27, 2024
Updated on July 9, 2024
Published on May 27, 2024
Updated on July 9, 2024
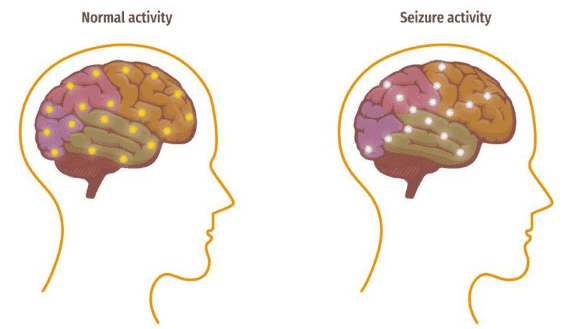
Table of Contents
Dementia is a condition that affects the mind, making it hard for people to remember things, think clearly, or take care of themselves. It can feel like a thick fog has settled over the brain, making everything more difficult. This isn’t just about forgetting where you put your keys; it’s about changes that can disrupt daily life. For those living with dementia, simple tasks like dressing or eating can become significant challenges.
Imagine watching a loved one slowly become a stranger or being that person who feels lost in a once-familiar world. That’s the heartache of dementia. It’s not just the person with the condition who suffers; families and caregivers also feel the weight of this change. It’s like watching a tapestry unravel, thread by thread, as memories and abilities slip away.
Now, let’s talk about seizures. When someone with dementia has a seizure, it’s like a storm in the brain. Electrical signals go haywire, causing different symptoms, like shaking or spacing out. Seizures can be scary and confusing, not just for the person who has them but also for those around them. They can happen without warning, turning an ordinary day upside down.
Understanding seizures in dementia is crucial because they can be a sign that the dementia is getting worse. They can also lead to other problems, like falls or injuries. Knowing what to look for and how to respond can make a big difference for nurses and caregivers. It’s about keeping the person safe and as comfortable as possible.
When we talk about dementia and seizures, we’re not just dealing with medical terms; we’re talking about people’s lives. It’s about preserving dignity, providing comfort, and connecting with the person behind the condition. It’s a journey that requires patience, empathy, and a deep understanding of the mind and the heart.
When we think about dementia, we often picture someone who has trouble remembering names or faces or who might get lost on their way home. But there’s another layer to this condition that isn’t talked about as much: seizures. Seizures in people with dementia are like unexpected storms that can confuse, cause fear, and cause additional health concerns.
It’s a two-way street between dementia and seizures. This means that having dementia can increase the risk of developing seizures and having seizures can increase the risk of developing dementia. It’s like a cycle where one condition can make the other more likely to happen. For example, changes in the brain caused by dementia may lead to seizures, and seizures can cause changes in the brain that might lead to dementia.
Dementia can make the brain more prone to seizures for several reasons. As dementia progresses, it causes more damage to brain cells. This damage can disrupt the normal electrical activity in the brain, which can lead to seizures. It’s like when a storm causes power lines to go down, and the electricity starts to act up. In the same way, when dementia damages the brain’s ‘wiring,’ it can cause the electrical signals to go haywire, resulting in a seizure.
Seizures can be particularly challenging in people with dementia because they can worsen confusion and memory problems. They can also be hard to recognize, especially if they don’t cause convulsions. Some seizures might cause a person to stare blankly or stop moving briefly. That’s why it’s so important for caregivers and nurses to know what to look for and how to help.
Understanding this connection is critical to providing the best care for someone with dementia. It’s about being prepared for the possibility of seizures and knowing how to respond. This knowledge can make a big difference in the life of someone with dementia, helping to keep them safe and as comfortable as possible.
When it comes to dementia, seizures are like uninvited guests that can show up without warning. They’re not the most well-known symptom of dementia, but they’re important to understand because they can affect a person’s health and safety.
Seizures can be broadly categorized into two types: generalized and focal.
Nonconvulsive seizures are tricky because they don’t have apparent signs like convulsions. They might cause subtle changes in behavior or awareness that can be easy to miss, especially in someone with dementia who may already have memory or behavior issues.
For example, a person might suddenly stop moving or talking or stare into space momentarily. These seizures can be brief, and the person might seem fine afterward, which makes them even more challenging to spot.
Caregivers and family members need to recognize these subtle signs because nonconvulsive seizures can still have a significant impact on a person’s health. They can lead to confusion, falls, or other injuries, and they can make dementia symptoms worse.
Understanding the different types of seizures and how to recognize them can help caregivers provide better care. It’s all about keeping a watchful eye and knowing what to look for so you can help keep your loved one safe and comfortable.
Caring for someone with dementia is like being a detective. It would help if you were observant, noting every detail, because sometimes the slightest change can be a clue to something bigger, like a seizure. Early identification of seizures and meticulous evidence gathering are crucial in managing dementia with seizures effectively.
Seizures can be sneaky, especially in someone with dementia. They might not always look like the dramatic fits we see on TV. Instead, they can be subtle, like a brief pause in movement or a sudden spell of confusion. Here are some signs to watch for:
Keeping a detailed record of any potential seizure activity is vital. Write down what you observe, no matter how insignificant it may seem. Note the incident’s date, time, duration, and any triggers you might have noticed, like lack of sleep or missed meals.
Here’s what you should document:
Reporting this information to healthcare providers is just as important as documenting it. It helps doctors and nurses understand the pattern and frequency of seizures, essential for diagnosis and treatment planning. Don’t hesitate to share your observations, as they can make a significant difference in the care and comfort of your loved one with dementia.
Caring for someone with dementia who experiences seizures can be a complex task, but understanding the treatment options can provide a pathway to better management and care.
Antiepileptic drugs (AEDs) are commonly used to treat seizures in patients with dementia. One such medication is levetiracetam, widely known as Keppra. Levetiracetam works by stabilizing the electrical activity in the brain, which can help prevent seizures. It is well-tolerated in elderly patients, including those with cognitive impairment, and can be effective in reducing seizure frequency.
Here are some points to consider when managing medications:
Strong partnerships with healthcare providers are essential in managing dementia and associated seizures. Here’s how caregivers can work effectively with medical teams:
By staying informed and involved in the treatment process, caregivers can help ensure that their loved ones with dementia receive the best possible care.
Please note that while gabapentin is commonly used for neuropathic pain and seizures, it can have side effects in the elderly, including dizziness, drowsiness, balance issues, and swelling of extremities. Additionally, there’s potential for cognitive impairment, kidney function concerns, and increased fall risk, which is why it is not included in this treatment discussion.
Caring for someone with dementia who experiences seizures means being prepared for both the expected and the unexpected. It’s about creating a safe space where seizures can be managed with compassion and expertise.
When a seizure starts, it’s essential to stay calm and focused. Here’s what you can do:
Remember, do not try to hold the person down or put anything in their mouth. These actions can cause more harm than good.
After a seizure, the person may feel confused and tired. This is known as the postictal state. Here’s how to help:
Managing seizures in someone with dementia requires a blend of knowledge, quick thinking, and a gentle touch. By following these steps, you can provide the care and support needed during these challenging moments.
When caring for someone with dementia, it’s crucial to understand how their blood sugar levels can affect their health, especially when it comes to seizures. Hypoglycemia, or low blood sugar, can be a severe issue that may lead to seizures, which can be particularly dangerous for individuals with dementia.
The brain relies on glucose as its primary source of energy. When blood sugar levels drop too low, the brain doesn’t get the proper fuel to function properly. This can lead to a range of symptoms, from mild confusion to severe seizures. In people with diabetes, severe hypoglycemic events can lead to seizures, which can be fatal if left untreated. It’s like running a car without enough gas; eventually, it will stall, and in the case of the brain, this can result in a seizure.
Preventing hypoglycemic events is critical to avoiding seizures. Here are some strategies that can help:
If a seizure does occur due to hypoglycemia, it’s essential to act quickly:
By understanding the connection between hypoglycemia and seizures and taking steps to prevent and respond to these events, caregivers can help ensure the safety and well-being of individuals with dementia.
Advocating for a loved one with dementia is about being their voice, mainly when they can’t express their needs and wishes themselves. It’s a role that requires strength, patience, and a lot of heart.
Effective communication with doctors and nurses is vital to ensure your loved one receives the best care possible. Here are some tips to help you communicate more effectively:
Making sure your loved one’s needs are met involves more than just medical care. It’s about ensuring they have quality of life and dignity. Here’s how you can help:
Remember, advocating for your loved one is a powerful act of love. It can make all the difference in their journey with dementia.
Caring for someone with dementia is a journey that’s often filled with love, challenges, and the need for a strong support network. Knowing where to find help and how to access resources can make all the difference.
Support groups are like lighthouses in the stormy seas of caregiving. They provide a place to share experiences, find comfort, and learn from others who understand what you’re going through. These groups can be found in various areas:
Professional resources can offer ongoing support and guidance for caregivers. These resources include:
Remember, you’re not alone as a caregiver. A community of support is ready to help you provide the best care for your loved one while also taking care of yourself.
Caring for a loved one with dementia who also experiences seizures is a profound act of love and dedication. It’s a role that comes with challenges but is filled with moments of deep connection and meaning.
Comprehensive care is about seeing the whole picture. It’s not just about treating seizures or managing dementia symptoms; it’s about nurturing the person’s overall well-being. This kind of care recognizes that every aspect of the patient’s health is interconnected.
For dementia patients with seizures, comprehensive care might include:
You are the strongest advocate for your loved one as a caregiver or family member. Your role is crucial in navigating the healthcare system and ensuring they receive the care and respect they deserve.
Here’s some encouragement for you in your advocacy journey:
Your efforts make a world of difference. With each act of care, appointment, and decision, you provide more than just medical care—love, comfort, and dignity. Keep going, knowing that what you do is genuinely invaluable.
Silent Seizures: A Surprising Phenomenon in Alzheimer’s Disease
Dementia with non-convulsive seizures: a case report (PDF)
The Bi-Directional Association Between Dementia and Epilepsy
What is the link between seizures and dementia?
Alzheimer’s Disease, Dementia Linked to Increased Seizure Risk
Tips for Seizure Observation and Recording (PDF)
Levetiracetam Improves Cognition in Patients With Alzheimer’s Disease and Epilepsy
Blood sugar may play a key role in dementia risk in stroke survivors
Do Low Blood Sugar Cause Seizures?
Diabetic Seizure: What Happens and What to Do
Trivia Games – Caregiver Activities for Alzheimer’s and Dementia
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Holistic Nurse: Skills for Excellence book series
Dementia Home Care: How to Prepare Before, During, and After
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
How Do I Know You? Dementia at the End of Life
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage