Tag: Hospice Nurse
Articles about and for hospice nurses including tips and tricks to provide the best care the terminally ill patient deserves.
Articles about and for hospice nurses including tips and tricks to provide the best care the terminally ill patient deserves.
I understand the challenges that patients and families face when receiving hospice services. One common issue that arises is the need for after-hour calls, which can add stress to an already demanding situation. However, with proactive care and effective communication, dayshift hospice RN case managers can play a crucial role in reducing after-hour calls and providing better support to patients and their families. Here’s how:
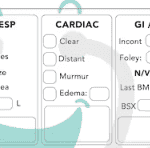
Hospice nurses play a vital role in providing quality care and comfort to terminally ill patients and their families. They must make accurate and timely assessments of the patient’s condition, needs, and preferences every visit. This article will outline the key aspects that hospice nurses should assess every visit, in addition to the standard physical assessment.

This article offers guidance for new visiting hospice nurses struggling with work-life balance. It covers strategies like maintaining a recertification journal, pre-charting before visits, assessing end-of-life status, educating families, and preparing for a "good death." By following these tips, nurses can take less work home while delivering focused, compassionate care.
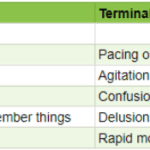
As an experienced hospice nurse, I understand how difficult it can be to distinguish between delirium and terminal restlessness. Both conditions can cause significant distress for the patient and their loved ones, and nurses must be able to tell the difference between them to provide the best possible care. In this article, I will share my knowledge and experience to help new hospice nurses understand the differences between delirium and terminal restlessness and how to rule out delirium.

Our primary focus for our patients is comfort at the end of life as hospice nurses. We work tirelessly to ensure that our patients receive the best possible care during their end-of-life journey. An aspect of that care that is often overlooked, but incredibly important is timely documentation.
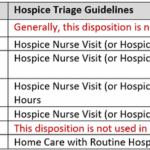
Documenting hospice visits at the bedside is crucial for several reasons. Not only does it help ensure that our patients are receiving the best possible care, but it also helps the hospice team as a whole and reduces issues when the caregiver must be involved in triage services. Here are just a few reasons why documenting hospice visits at the bedside is so important:
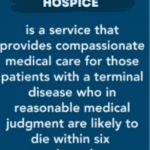
As an experienced hospice nurse, I understand how overwhelming and emotional it can be for terminally ill patients and their loved ones to navigate the hospice process. Hospice care is a compassionate and comprehensive approach to end-of-life care, designed to provide comfort, pain management, and emotional support to patients and their families. However, many people have questions about hospice eligibility and hospice recertification. In this article, I will provide a generalized guide to help you understand these important aspects of hospice care.

Hospice care offers a specialized service known as the Continuous Care Benefit. This unique care type provides crucial 24-hour support to patients who are going through an acute symptom crisis. In this article, we'll delve into what Continuous Care Benefit is, who's eligible for it, how it operates, why it's important, how to access it, and its duration.

I remember having some nurses tell me that nurses who go into hospice lose their critical thinking skills because they are dealing with people who are dying. Little did they know that hospice nurses often need to think far more critically than other nurses. Let’s outline some key critical thinking areas as a hospice nurse.
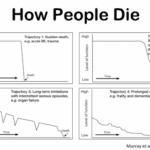
Admitting a patient to hospice services is a complex and sensitive process that requires careful assessment and communication. One of the challenges that hospice nurses face is to determine if the patient is close to the transitioning phase of dying, which is the final stage of life when death is imminent. This phase usually lasts for one to two weeks, and it is essential to prepare the family and provide a plan for increased hospice involvement during this time. However, on admission, hospice nurses do not have the luxury of having visited with the patient over the past several weeks to months to observe the changes that often signal that death is approaching. Therefore, they need to rely on other indicators to help them identify whether the patient is transitioning.
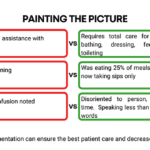
Hospice recertification is a crucial step in which the registered nurse case manager can help make the case for continued hospice eligibility. May I encourage my fellow hospice nurses to start using a template to ensure your recertification visits are consistent and that you are leading early in the documentation portion regarding what declines have occurred since admission and last recertification?
Faith and religion in the workplace: Yes, faith has a place in work, and when utilized to direct how one works and interacts with one's patients and families, it can result in a blessing that does not disrespect others.
This article came to be partly a response to one of my favorite YouTube nursing channels, where Nurse Katherine provides educational videos for new and experienced nurses. Her most recent episode at https://www.youtube.com/watch?v=N_lE9O1I3LQ asks the valid question relating to the place of “Religion, Beliefs, and the practice of Medicine | should & can they be combined?”
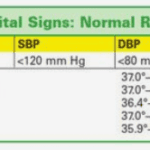
I don’t know about you, but every time I see a patient and their family for the first time and take their vitals as part of the nursing assessment, either after each vital or at the end of the vital checks, I’m asked something to the effect of “is that good?”
As you, my friendly readers, bloom as hospice nurses, you will learn that the vital sign portion of the assessment is just a smidge of the entire assessment as to whether someone is approaching the end of life, going through reversible or terminal restlessness, or just having a difficult day. Let me share how I educate families that get hyper-focused on vitals.

When I first started working in the field of hospice, my clinical manager told me (I’m paraphrasing), one day you will be able to walk into the room, and without getting a single vital sign, just by visual observation, be able to tell that the person is dying or will be shortly dying. That was about three years ago. Today, it’s almost chilling for me (as it is both a blessing and tremendous responsibility) to be able to share she told the truth, and that over time — if you give yourself patience and grace and take the time to listen, observe, and remember — you too will learn how to tell when someone is close to or otherwise is dying.
Please allow me to share some of my insight as to how I know a person has less than a month left to live, and often far less. First off, let’s go into the important discussion you should have with the family, friends, and the patient themselves that provides an overall background to the prognosis. That discussion should be centered around what types of decline (downward, negative) changes have been taking place in the patient’s life over the last six months making note as to whether the decline is minor, medium, or major and the frequency (once a month, once a week, etc.) of those changes.
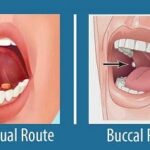
Your dying patient has lost their gag reflex as part of the dying process. One of the questions I implore you to ask yourself is what’s the safest route to administer liquid medications? Well, before even going to answer this question, unless contraindicated, make sure the patient’s head of the bed is at least at a 30 to 45-degree angle (I prefer the latter).
The buccal route is the safest route to administer liquid medications at the end of life in my experience. In practice, I strongly encourage you as well as the families we mutually teach to give any liquid medications on the side of the mouth least likely to have spillage — this depends on the position of the patient — and slowly over time giving the medication in 0.25 ml increments allowing for the absorption of the medication switching cheeks as applicable.

Navigating the final days of a loved one's life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.

People often say to me, "It must be challenging to work in hospice." Unfortunately, due to HIPAA regulations, I cannot share photos of the events that occur. However, let me share a poignant moment from today—a dying individual's final wish was to feel the warmth of the sun on their face one last time. And we made that wish come true. This seemingly simple gesture held immense significance for both the patient and their family.

One of the main challenges of new nurses is time management. In a hospital or nursing home setting, you often have coworkers to rescue you in a pinch in case you are overwhelmed; on top of having nearby coworkers, most orientation programs, as well as nursing schools, focus on time management skills in a facility setting. Yet what about time management as a visiting nurse — in home health or home hospice or both?
Let me share with you my wisdom and experience in time management in the field of a visiting nurses to hopefully help you have more time for life compared to work — a better work-life balance.

If you are a new nurse to hospice, one of the tasks you probably dread is doing an admission especially if you have scheduled visits the same day as the admission.
I would like to share with you some tips that when applied may help lower your stress level, and help you remain on time even in cases where you have three to four visits including recertification to do the same day.
Here are some ideas that may be beneficial to those of you who are relatively new visiting hospice nurses:

As an INFJ, I’m almost constantly introspective. Today, I was helping with an emergency where one of our wonderful on-call nurses was in a car accident. During my visit with a patient I admitted yesterday who is transitioning towards actively dying, I was in bewilderment in my mind about how comfortable and peacefully patient I am when I’m around the terminally ill and their family.