End-of-Life Determinations for Newly Admitted Patients
Published on February 4, 2023
Updated on May 26, 2024
Published on February 4, 2023
Updated on May 26, 2024
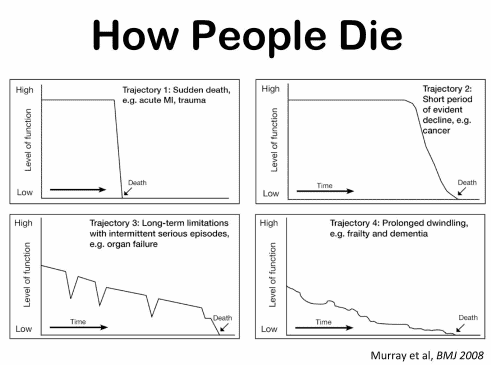
Table of Contents

Admitting a patient to hospice services is a complex and sensitive process that requires careful assessment and communication. One of the challenges that hospice nurses face is to determine if the patient is close to the transitioning phase of dying, which is the final stage of life when death is imminent. This phase usually lasts for one to two weeks, and it is essential to prepare the family and provide a plan for increased hospice involvement during this time. However, on admission, hospice nurses do not have the luxury of having visited with the patient over the past several weeks to months to observe the changes that often signal that death is approaching. Therefore, they need to rely on other indicators to help them identify whether the patient is transitioning.
In this article, we will provide some tips to incorporate into your nursing practice to recognize if the person you are admitting may be in the transitioning phase of dying. These signs are based on clinical experience and observation and may vary from patient to patient. However, they can serve as general guidelines to alert you of the possibility of a fast death.
Some of the signs of the transitioning phase are:
In conclusion, hospice nurses need to be aware of the signs of the transitioning phase of dying, which is the final stage of life when death is imminent. These signs can help them determine if the patient they are admitting may be in the transitioning phase or not and plan accordingly for increased hospice involvement and family support. While there should be a post-admission visit within 24 to 48 hours of the admission if you have any concerns the patient may go fast, try to schedule a visit within 24 hours with consideration for even a 3rd visit in a row as it is better to be safe than to miss the opportunity to help the family and caregivers prepare for what may be a fast death.
Multiple Articles on Tips for Nurses
Tips for new nurse — Terminal Restlessness
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death