How Hospice RN Case Managers Can Reduce After-Hour Calls
Published on May 26, 2023
Updated on May 22, 2024
Published on May 26, 2023
Updated on May 22, 2024
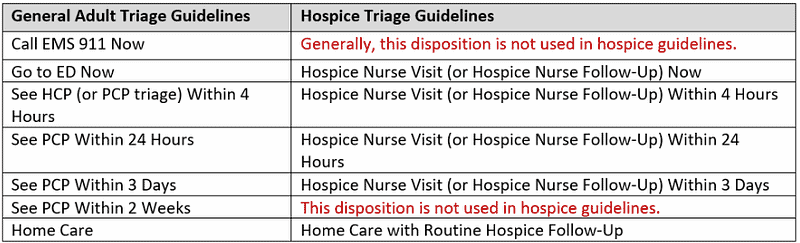
Table of Contents
I understand the challenges that patients and families face when receiving hospice services. One common issue is the need for after-hour calls, which can add stress to an already demanding situation. However, with proactive care and effective communication, dayshift hospice RN case managers can be crucial in reducing after-hour calls and providing better support to patients and their families. Here’s how:
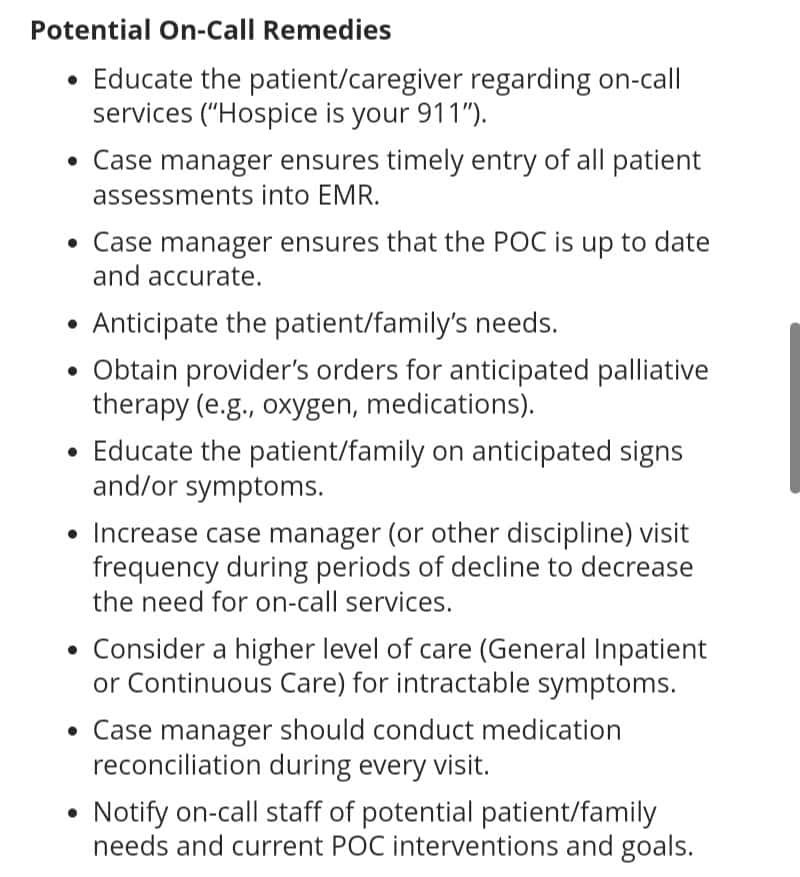
Take the time to educate patients and families: One of the main reasons for after-hour calls is a lack of understanding about the patient’s condition or the appropriate actions to take. As a dayshift hospice RN case manager, you can dedicate time during your visits to thoroughly educate patients and families about the patient’s specific needs, symptoms to watch for, and steps to take when certain situations arise. This proactive approach can empower them to handle situations independently, reducing the need for after-hour calls.
Provide comprehensive care instructions: Ensure patients and families have clear and concise instructions covering various aspects of their loved one’s condition. This may include information on medication administration, managing pain or discomfort, handling emergencies, and contacting the appropriate resources. Written materials or handouts can serve as a helpful reference, reinforcing what you discuss during your visits.
Empowering patients and families is crucial in reducing after-hour calls. When individuals feel confident in managing certain situations, they are less likely to seek immediate assistance. RN case managers can empower patients and families by equipping them with the necessary knowledge, resources, and support.
To empower patients and families effectively:
Build a strong rapport with patients and families: Establishing trust and a good relationship with patients and families is critical to reducing after-hour calls. Take the time to listen to their concerns, address their questions, and provide empathetic support. Building trust and being approachable will make them more comfortable contacting you during regular hours instead of resorting to after-hour calls.
Encourage open communication: Make it clear to patients and families that you support them and that their concerns are valid. Encourage them to contact you during regular hours if they have any questions or if their loved one’s condition changes. Let them know that their calls will be prioritized and that you will provide timely responses. By fostering open communication, you can address their needs promptly, reducing the likelihood of after-hours calls.
To build trust and establish relationships effectively, RN case managers can:
Involve the entire hospice interdisciplinary team: Collaborate closely with the interdisciplinary team involved in the patient’s care, including physicians, social workers, and counselors. Regularly communicate and share updates to ensure everyone is on the same page regarding the patient’s condition, care goals, and any care plan changes. By working together, you can proactively address issues during the day and prevent emergencies or crises that might lead to after-hour calls.
Anticipate and address potential issues: Use your experience as a hospice nurse to anticipate and proactively address potential issues. For example, if a patient is experiencing escalating pain, work with the physician to adjust the pain management plan before it becomes an after-hours emergency. By avoiding potential problems, you can help prevent after-hours calls and ensure the patient’s comfort and well-being.
Here’s how RN case managers can enhance care planning and coordination:
One primary reason for after-hours calls is the management of distressing symptoms. Hospice RN case managers are crucial in assessing and managing symptoms during regular business hours, ensuring patients receive appropriate interventions promptly. By addressing symptoms proactively, they can minimize severe symptoms requiring after-hours calls.
Proactive symptom management should be a priority. Addressing symptoms before they escalate can reduce the need for urgent after-hour interventions. Consider the following approaches:
Assess the need for medication refills and supplies every visit and check that any previous orders came in or are otherwise en route within a reasonable timeline for arrival. This helps the patient maintain consistent comfort, reduces anxiety among the patient and family, and reduces calls to triage for items easily handled during the scheduled visit.
Remember that it is prevalent for patients and families to forget what medications and supplies are covered/provided by hospice and those from other sources. Therefore, it is in everyone’s best interest during your visits to regularly check on those items not covered by the hospice to see if they are getting low and educate the family on how to restock those items.
Your role as an RN Case manager is crucial in providing proactive care and support to patients and their families. You can significantly reduce after-hour calls by thoroughly educating patients and families, establishing trust and open communication, and engaging in collaborative care planning and proactive symptom and medication/supply management. This not only helps alleviate stress for patients and families but also allows you to provide more focused and timely care during your scheduled shifts.
Remember, each patient and family are unique, and their needs may vary. Flexibility, compassion, and adapting your approach to suit individual circumstances are vital to providing exceptional hospice.
What Hospice Nurses should assess every visit
Preparing for a Good Death: Topics to Cover with Hospice Patients and Their Families
The importance of caregiver journaling for the patient and family
Triage of After-Hours Hospice Calls
A Descriptive, Retrospective Study of After-hours Calls in Hospice and Palliative Care
Utilization of after-hours telephone support in a home-based hospice service