Tag: Comfort Care
Articles about comfort care for the terminally ill patient seeing a good death.
Articles about comfort care for the terminally ill patient seeing a good death.

This detailed guide provides insights into the transition from palliative care to hospice, offering practical advice and emotional support to patients, caregivers, and family members during this critical phase.

Discover compassionate care techniques that address depression and anxiety in dementia without relying on antidepressants. This article delves into holistic approaches that enhance quality of life and promote mental well-being in dementia care.

This comprehensive guide provides essential insights into recognizing and addressing delirium in terminally ill individuals. It’s an invaluable resource for nurses, caregivers, and families, offering practical advice and empathetic support.

Palliative wound care plays a crucial role in enhancing the quality of life for terminally ill patients receiving hospice care. As a new hospice nurse or caregiver, understanding wound management is essential. In this article, we’ll explore evidence-based practices, practical tips, and resources to empower you in providing compassionate wound care.

This article delves into the intricate dynamics of hospice nurses’ relationships with patients, examining the benefits and challenges of emotional investment versus professional detachment.

Geriatric fractures can profoundly affect the elderly, potentially leading to a terminal prognosis. This article discusses the emotional and physical challenges, the importance of hospice care, and the role of caregivers in providing end-of-life support.

This comprehensive guide simplifies Medicare Hospice Benefits for caregivers and family members. Learn about eligibility, services, finding providers, and more. Empower yourself with the knowledge to make informed decisions about hospice care.

Discover practical strategies and tools in "Aphasia Unveiled: Communication Aids for Caregivers." These aids, such as whiteboards, picture catalogs, and tablet software, are designed to empower you with the capability and confidence to support your loved ones with aphasia.

Hospice nurses' presence visits provide vital emotional support and companionship for terminally ill patients and their families. Learn how these visits offer comfort, dignity, and peace during end-of-life care.

Deciding between home care and facility care for a terminally ill loved one requires careful consideration of medical, emotional, and practical factors to ensure comfort and dignity.
Caring for a loved one with terminal metabolic encephalopathy requires compassion and understanding. This guide provides insights into recognizing symptoms, adapting care strategies, and supporting the patient and caregiver through this challenging journey.

Hospice care is often seen as the final chapter, but sometimes, it leads to unexpected recoveries. This article explores stories of resilience and healing in hospice care, reminding us that hope and recovery can still be part of the journey.

In-home hospice care offers a sanctuary of comfort and support for terminally ill loved ones and their families. It brings medical care, emotional solace, and practical help to your doorstep, allowing patients to spend their final days in the warmth of home. Learn how hospice care can provide personalized support, ensuring dignity and quality of life.

Explore the role of oxygen saturation in hospice care, where comfort takes precedence over numbers. Learn how hospice teams prioritize quality of life, interpret vital signs differently, and make ethical decisions about oxygen use. Discover a compassionate approach focused on dignity and peace.

When a loved one is facing a serious illness, it can feel like standing at a crossroads. Each path represents a different way to care for them in their time of need. It’s a moment filled with tough choices and deep emotions. This article thoroughly explains hospice care, its philosophy, and the benefits it provides to patients and families facing terminal illness. Learn about the decision-making process, the hospice experience, and how to navigate this difficult choice with dignity and love.

Dementia is a word we use to describe a significant change in the brain that makes it hard for people to remember things, think clearly, make decisions, or even control their emotions. It’s like a fog that slowly creeps in, affecting how a person thinks, feels, and lives daily. It’s not just one disease but a group of symptoms that can be caused by different diseases, including Parkinson’s and Alzheimer’s.
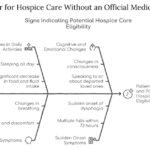
This article aims to provide information and guidance on qualifying for hospice care without an official medical diagnosis. We will explain hospice care, how to access it without a physician’s consent, what to expect, and how to make the most of it.

Hospice care focuses on comfort rather than curative treatments. In emergencies, calling 911 can lead to invasive procedures and disrupt hospice care. This article explores why contacting your hospice provider first is crucial and offers guidance on alternatives to calling 911.

If you are caring for a loved one with pulmonary fibrosis, you may have many questions and concerns about their condition and how to support them best. You may also feel overwhelmed, stressed, or isolated by the challenges and responsibilities of caregiving. You are not alone. Many people face similar situations and emotions when caring for someone with chronic and progressive lung disease.
This article will help you understand pulmonary fibrosis and how it affects your loved one and yourself. It will also provide practical and helpful information on providing the best care for your loved one and yourself.
Explore the complex world of dementia-related aggression and learn how to identify its underlying causes. This comprehensive guide offers insights into medication-related issues, pain management, and non-pharmacological interventions. Discover compassionate care strategies to support patients and caregivers on this challenging journey.
Discover the truth behind the myth that medications can keep terminally ill patients alive indefinitely. This article explores the psychological factors behind this belief and its consequences while providing compassionate strategies to cope with the reality of losing a loved one while ensuring quality end-of-life care.

Medications like anticoagulants, antidepressants, and NSAIDs can cause harm to hospice patients. Learn how to balance comfort and safety with individualized care.
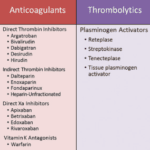
Anticoagulants can prevent blood clots but also cause bleeding risks for terminally ill patients. This article explains why these medications should be regularly reviewed for deprescribing, outlining factors like prognosis, preferences, and palliative care options to consider when making informed, compassionate choices aligned with the patient's goals.

This article discusses the importance of quarterly medication reconciliation for terminal patients and their families. It explains the benefits, such as improving patient safety, quality of life, symptom management, and the challenges and solutions. It also addresses the need to re-evaluate certain medications, like donepezil and memantine, for patients with dementia as their disease progresses.