Methadone: A Compassionate Approach to Managing Terminal Pain
Published on May 5, 2024
Updated on June 7, 2025
Published on May 5, 2024
Updated on June 7, 2025
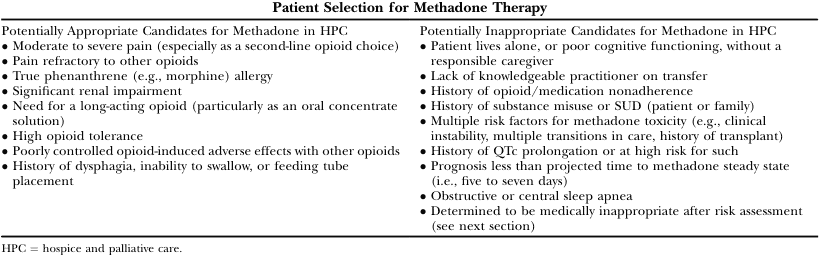
Table of Contents
Pain management stands as a beacon of relief and dignity in the quiet sanctity of hospice care, where every breath is a testament to life and its poignant finale. For professionals, family members, and caregivers, understanding the delicate balance between alleviating pain and maintaining consciousness is a profound responsibility. This article serves as a compassionate guide through the complexities of pain management, shedding light on the benefits and considerations of using methadone over morphine for those in the twilight of their journey.
Pain management in hospice is not merely a clinical task but an art that intertwines with the deepest threads of human compassion. It’s about creating a sanctuary where pain does not overshadow the remaining moments of connection and closure. Hospice care is holistic, addressing not just the physical symptoms but also the emotional and spiritual needs of patients and their families.
The goal is to manage pain effectively, allowing patients to engage with loved ones, reflect on their lives, and pass with dignity. This involves a multidisciplinary approach, utilizing medications, psychological support, and complementary therapies such as massage or aromatherapy to soothe the body and soul. Pain is subjective and personal, and its management must be tailored to the individual, respecting their wishes and the unique way they experience discomfort.
Morphine, a time-honored medication, has been the cornerstone of pain management in hospice care. Yet, methadone emerges as a compelling alternative, particularly for complex pain syndromes that morphine cannot fully address. Both drugs are opioids, but methadone’s pharmacological profile gives it certain advantages. It binds to multiple opioid receptors, offering broader pain relief, and has a longer duration of action, which can provide sustained comfort.
Methadone’s unique properties make it effective against various types of pain, including the challenging neuropathic pain often encountered in advanced illnesses. Moreover, its potential for fewer side effects and lower risk of tolerance makes it a valuable option in the hospice setting, where the quality of life is paramount.
As we delve deeper into these medications, we will explore their roles in pain management, the nuances of dosing and administration, and the circumstances under which methadone may not be the ideal choice. We aim to equip you with the knowledge and empathy required to navigate these decisions, ensuring comfort and peace for those at the end of life’s journey.
In the realm of hospice care, where the focus is on comfort and quality of life, methadone has emerged as a beacon of hope for many. Its use in pain management for terminally ill patients is gaining recognition for its effectiveness and versatility. Methadone, a medication with a storied history in treating opioid addiction, is now being appreciated for its unique properties in pain relief.
Methadone’s mechanism of action sets it apart from morphine and other opioids. As a full µ-opioid receptor agonist, methadone mimics the body’s natural opioids, providing relief from pain by releasing neurotransmitters involved in pain transmission. But methadone goes further; it also acts as an antagonist of the N-methyl-D-aspartate (NMDA) receptor, which plays a significant role in modulating pain. This dual action not only helps in managing various types of pain, including challenging neuropathic pain, but also reduces the development of tolerance to the medication, a common issue with long-term opioid use.
Methadone’s efficacy in pain relief is well-documented. Its ability to provide a more consistent and prolonged analgesic effect compared to morphine makes it a valuable option for patients in need of long-term pain management. The extended half-life of methadone means that patients require fewer doses throughout the day, which can significantly improve their comfort and quality of life. Additionally, methadone is effective in patients who have not found relief with other opioids, offering a chance for improved pain control and a reduction in adverse effects.
In hospice care, where every moment is precious, methadone offers a way to manage pain that respects the dignity and comfort of patients in their final days. It’s a choice that can make a meaningful difference, allowing patients to focus on their lives and loved ones rather than the pain they are experiencing.
Navigating the transition from oral morphine to oral methadone can be a complex process, requiring a thoughtful and patient-centered approach. The conversion is not a simple one-to-one switch, as methadone’s potency can vary depending on the existing dose of morphine. It’s essential to start with a conservative methadone dose, significantly, since methadone’s effects can accumulate over time due to its long half-life.
When converting from oral morphine to oral methadone, it’s crucial to consider the total daily dose of morphine. The conversion ratio can range from 4:1 to 12:1, with higher morphine doses requiring a more conservative approach to methadone dosing. For example, a patient receiving lower doses of morphine may have a conversion ratio closer to 4:1, while those on higher doses may require a ratio of 12:1 or even more conservative. It’s also essential to account for individual patient factors, such as age, organ function, and concurrent medications, which can influence the appropriate conversion ratio.
Even when methadone is the primary medication for pain management, breakthrough pain can still occur. In such cases, it may be appropriate to use morphine for breakthrough pain due to its quicker onset of action. Methadone can be used for breakthrough pain as well, but this requires careful consideration of the timing and dosage, as methadone’s long-lasting effects can increase the risk of accumulation and potential overdose.
Administering methadone in hospice settings demands vigilance and a commitment to best practices. This includes regular pain assessments, cautious dose titration, and close monitoring for side effects. Methadone should be started at a low dose and increased slowly, with adjustments made based on the patient’s response and any side effects experienced. It’s also vital to educate both caregivers and patients about the unique properties of methadone, including its delayed onset of peak effects and the potential for interactions with other medications.
In summary, methadone offers a valuable option for pain management in hospice care, but it requires a nuanced and individualized approach to dosing and administration. By adhering to these guidelines and ratios, hospice professionals can ensure patients receive the most effective and safe pain management possible.
Titration, the careful adjustment of medication to achieve the optimal balance of pain relief with minimal side effects, is a cornerstone of effective pain management in hospice care. For those entrusted with this delicate task, it is a blend of science and empathy, a measured approach that honors the dignity of the patient’s final journey.
Cautious titration is vital to avoid the pitfalls of overmedication. The goal is to provide enough medication to ease pain without causing undue sedation or other adverse effects that can diminish a patient’s quality of life. It’s a gentle ascent to comfort, guided by the ‘start low and go slow’ principle. This approach respects the body’s response to new medication levels and allows time for adjustment, ensuring that the patient remains alert and engaged as their condition permits.
Monitoring and adjusting the dosage is an ongoing process that requires vigilance and responsiveness to the patient’s needs. It involves regularly assessing pain levels, monitoring for signs of discomfort, and being attuned to the patient’s nonverbal cues. Adjustments should be made based on a comprehensive understanding of the patient’s pain experience, previous medication history, and current physiological state.
Maintaining open communication with family members and caregivers is essential, as well as educating them about what to expect and involving them in the monitoring process. This collaborative approach ensures that the patient’s comfort is managed with the utmost care and consideration, providing peace of mind for everyone involved in their care.
In summary, titration is a nuanced process that requires a thoughtful and informed approach. By titrating cautiously and monitoring closely, hospice professionals, family members, and caregivers can work together to ensure that patients receive the most comfortable and dignified care possible in their final days.
When caring for someone at the end of life, managing medication side effects is as crucial as managing pain itself. Methadone, while effective for pain relief, comes with its own set of side effects that hospice professionals, family members, and caregivers should be aware of and know how to manage.
Methadone can cause a variety of side effects, some more common than others. It’s essential to monitor for signs of nausea, vomiting, constipation, dizziness, and fatigue, as these are among the most frequently reported. These symptoms can often be managed by adjusting the medication regimen or by receiving additional treatments. Still, they should not be ignored as they can significantly impact a patient’s quality of life.
Constipation is a prevalent issue with methadone and other opioids, and it requires proactive management. Encouraging a diet high in fiber, maintaining adequate hydration, and using stool softeners or laxatives as needed can help mitigate this uncomfortable side effect.
Caregivers can take several proactive measures to manage methadone’s side effects effectively. Maintaining open communication with healthcare providers about new or worsening symptoms is essential. Keeping a detailed journal of the patient’s symptoms, medication times, and dietary habits can help identify patterns and triggers that may contribute to side effects.
It is crucial to seek medical attention immediately for more serious side effects, such as severe dizziness, difficulty breathing, or signs of an allergic reaction. Caregivers should also be educated on the potential for drug interactions and the importance of using methadone as prescribed, without deviation.
In summary, while methadone can be a practical component of pain management in hospice care, it is vital to be vigilant about monitoring and managing its side effects. Through careful observation and proactive measures, caregivers can help maintain the comfort and dignity of their loved ones during this sensitive time.
In the compassionate landscape of hospice care, methadone stands as a powerful ally in the battle against pain. However, it is not a universal remedy. There are circumstances where methadone may not be the best choice for managing a patient’s pain. Understanding these situations is crucial for ensuring the safety and well-being of those we care for.
Methadone, like all medications, comes with its own set of contraindications and cautions. It is unsuitable for everyone and can be harmful in certain medical conditions. For instance, patients with severe respiratory issues, such as asthma or chronic obstructive pulmonary disease (COPD), should avoid methadone due to the risk of respiratory depression. Those with gastrointestinal blockages may also face complications, as methadone can exacerbate these conditions.
Additionally, methadone’s interaction with other medications is a significant concern. It can interact with a variety of drugs, leading to potentially dangerous side effects or reduced effectiveness. Therefore, it’s imperative to review a patient’s entire medication profile before considering methadone.
When methadone is not an option, there are alternative pain management strategies that can be explored. These alternatives range from other pharmacological treatments to non-pharmacological approaches:
It’s important to remember that these alternatives should be tailored to each patient’s individual needs. What works for one person may not work for another, and a multidisciplinary approach is often the most effective. By understanding the limits of methadone use and the breadth of alternatives available, hospice professionals, family members, and caregivers can ensure that patients receive the most appropriate and compassionate care in their final days.
As we draw this discussion to a close, it’s essential to reflect on the role that methadone can play in hospice care and the empowerment of caregivers. The journey through terminal illness is fraught with challenges, but with the proper knowledge and support, it can also be a time of profound connection and dignity.
Methadone has a unique place in the pantheon of pain management, particularly within the sensitive confines of hospice care. Its ability to alleviate complex pain syndromes and provide lasting relief is invaluable. However, it’s essential to approach methadone with a balanced perspective, acknowledging both its potential benefits and its limitations. Methadone can offer a sense of solace to those in the throes of terminal pain, yet it demands a careful, educated approach to its administration and monitoring.
Caregivers are the unsung heroes in the narrative of terminal illness. Empowering them with knowledge, resources, and emotional support is crucial for enhancing the quality of life for the terminally ill. By providing caregivers with the tools they need to manage pain effectively, we improve the patient’s comfort and give caregivers a sense of agency during a time that can often feel overwhelming.
In essence, the use of methadone in hospice care, when handled with expertise and compassion, can be a powerful ally in our collective endeavor to provide comfort and dignity to those at the end of life’s journey. We carry this responsibility with great care, always striving to ensure that our actions honor the lives and legacies of those we serve.
Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors (PDF)
Chronic Pain Management: Dosing and Conversion Chart for Opioid Analgesics (PDF)
Methadone Treatment for Pain States
Methadone: A Compassionate Approach to Managing Terminal Pain
Methadone for pain in palliative care: the development of an online CME training tool
Safe and Appropriate Use of Methadone in Hospice and Palliative Care: Expert Consensus White Paper (PDF)
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
Pain Assessment in Hospitalized Older Adults With Dementia and Delirium
Pain Assessment in Dementia – International Association for the Study of Pain (IASP)
Pain Assessment in People with Dementia: AJN The American Journal of Nursing
Pain Assessment in Advanced Dementia Scale (PAINAD) – MDCalc
Uncontrolled Pain and Risk for Depression and Behavioral Symptoms in Residents With Dementia
Pain Assessment and Pharmacologic Management
Adult Nonverbal Pain Scale (NVPS) Tool for pain assessment
Assessing pain in patients with cognitive impairment in acute care
Pain Assessment in Advanced Dementia Scale (PAINAD)
Pain Assessment in Non-Communicative Adult Palliative Care Patients
Pain Assessment in People with Dementia
Tools for Assessment of Pain in Nonverbal Older Adults with Dementia: A State-of-the-Science Review
Understanding the physiological effects of unrelieved pain
Untreated Pain, Narcotics Regulation, and Global Health Ideologies
Bridges to Eternity: The Compassionate Death Doula Path book series: