Tag: Caregiver Journaling
Articles about the importance of caregiver journaling to promote improved comfort and patient centered care.
Articles about the importance of caregiver journaling to promote improved comfort and patient centered care.

Discover practical strategies for supporting a loved one with cognitive decline during doctor visits. From preparation to follow-up, learn how to communicate effectively, respect autonomy, and handle sensitive topics. This guide offers valuable tips for caregivers to ensure productive appointments and quality care for their loved ones.
Learn to recognize early dementia signs and explore care options, including hospice. This guide offers insights into dementia, practical care tips, and when to seek professional help.

Discover how to use the CUS tool and Caring Feedback Model to advocate for your loved one's health. This guide empowers caregivers to communicate effectively with healthcare providers, ensuring their concerns are heard and addressed.
Hospice care is a unique medical approach that prioritizes comfort and peace for the terminally ill rather than vital signs or curative treatments. It offers holistic support, addressing physical, emotional, and spiritual needs. This compassionate care improves the quality of life, dignity, and a peaceful end aligned with the patient's values.

Managing bowel problems in terminally ill patients is crucial for their comfort and dignity. This guide offers practical tips for caregivers and hospice nurses to address constipation, diarrhea, bowel obstruction, and ascites, ensuring patients' better quality of life.

Discover essential educational topics for hospice nurses during admission and follow-up visits. Learn how to effectively communicate with patients and families, manage symptoms, provide emotional support, and navigate end-of-life care. Enhance your skills to deliver compassionate, comprehensive hospice care.

Facing the reality of a loved one's terminal illness can be a challenging and emotional journey. As a hospice registered nurse case manager, I understand the importance of providing compassionate and clear information to empower patients, caregivers, and families. In this article, we'll explore how you, as a family member, can use your own observations and senses to recognize the signs that your loved one may be in the terminal stage of their illness. Remember, while medical professionals have their tools, your observations and intuition significantly matter.

This article will delve into common infections in geriatric patients, encompassing early, middle, and late-stage symptoms, preventive measures, and prevalent treatment approaches, particularly for patients facing a terminal illness prognosis of six months or less.
Receiving news that a loved one has reached the end-stage of a stroke can be overwhelming and emotionally challenging. As an experienced hospice nurse with years of experience, I understand how crucial it is for families to have accurate information about what to expect during this journey. In this article, we will explore the changes that may occur in a loved one with end-stage stroke and how you can best care for them throughout this process.
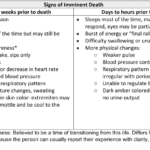
Recognizing end-of-life signs can be challenging. This guide outlines key symptoms indicating a terminally ill patient may have less than two weeks, offering crucial insights for caregivers and families.
Caring for a loved one with dementia can be a challenging journey, filled with complex emotions and difficult decisions. As families and caregivers, it's crucial to understand the nature of dementia and the various tools available to help assess and manage the condition. This article aims to provide a comprehensive guide to the seven most common memory tests used to evaluate if a person has dementia. These include the Alzheimer's Disease Assessment Scale-Cognitive (ADAS-Cog), Mini-Mental State Examination (MMSE), General Practitioner Assessment of Cognition (GPCOG), Montreal Cognitive Assessment (MoCA), Self-Administered Gerocognitive Exam (SAGE), Neuropsychological evaluation, and Short Test of Mental Status. Each of these tests offers unique insights into the cognitive abilities of an individual and can be instrumental in the early detection and management of dementia. By understanding these tests, you can better navigate the path of dementia care and ensure your loved one receives the best possible support.
As a hospice nurse, I understand the importance of documenting observational signs of discomfort in terminally ill patients. This guide covers recognizing physical and behavioral cues indicating discomfort, even if patients don't express it. It also highlights the benefits of journaling for families and nurses, with tips for effective documentation to enhance patient comfort and care.
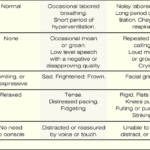
If you have a loved one with dementia, it can be difficult to know if they are in pain or discomfort. The Pain Assessment in Advanced Dementia Scale (PAINAD) is a tool that can help you determine if your loved one is uncomfortable. The Pain Assessment in Advanced Dementia Scale (PAINAD) is different from other pain assessment tools for people with dementia in several ways:

Heart failure is a complex medical condition that can impact the quality of life of patients, especially those in hospice care. As a hospice nurse, assessing the heart failure stage is crucial to providing appropriate care accurately. This article will explore the New York Heart Failure Classification System, its stages, and how to assess patients for their stages. Additionally, we will emphasize the importance of documentation in compliance with Medicare guidelines for terminally ill patients with heart failure.
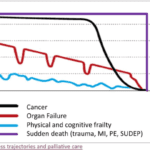
Explore the journey of functional decline in the natural dying process. This article provides insight for caregivers and families, emphasizing the importance of documenting changes to enhance care and decision-making in life’s final chapter.

Medication reconciliation plays a pivotal role in hospice care, ensuring terminally ill patients receive safe medication regimens. This process involves maintaining an accurate medication list to prevent adverse drug events. It's essential at various stages, including admission, recertification, and changes in condition. Healthcare professionals should be familiar with tools like the Beers Criteria and STOPP/START criteria to identify potentially inappropriate medications and prescribing omissions in older adults.
When a loved one is terminally ill, it can be a perplexing and emotional journey. Understanding the root cause of their declining health becomes paramount. It's a complex puzzle where family members often grapple with questions: Are the symptoms a result of medications prescribed, or are they intrinsic to the terminal disease? This article delves into the critical distinctions between medication side effects and the natural progression of terminal illnesses, offering insights to empower families and caregivers in making informed decisions about their loved one's care.

Serotonin syndrome is a potentially life-threatening condition caused by an excess of serotonin in the body. Detecting this condition early is crucial, but it can be particularly challenging when dealing with dementia patients due to communication barriers and the complexity of their symptoms. In this article, we will present three case studies that highlight the early detection and successful management of serotonin syndrome in patients with different types of dementia: Alzheimer's disease, vascular dementia, and Lewy Body Dementia.

Hospice nurses assess the status of the patient's journey towards the end of life every nursing visit. Situations where a reversible condition can drastically impact the patient and the hospice assessment can occur. If it is not caught, it is potentially mistreated, leading to increased discomfort and a faster death, often involving increased suffering. One of the common clues that someone is getting closer to dying is increased agitation and restlessness.
Are you aware of Serotonin Syndrome?
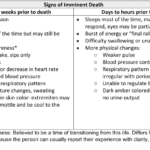
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.
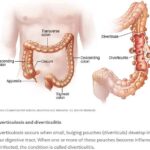
Caring for a loved one with a history of diverticulitis requires a combination of preventive measures, early detection of warning signs, and understanding the common signs and symptoms of this condition. Your role as a caregiver is crucial in providing support and assistance to ensure their well-being. In this comprehensive guide, we will explore essential aspects of caring for someone with diverticulitis, including prevention, early warning signs, and treatment options.
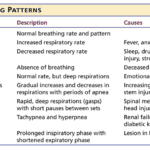
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.
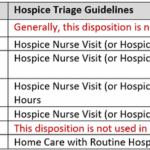
I understand the challenges that patients and families face when receiving hospice services. One common issue that arises is the need for after-hour calls, which can add stress to an already demanding situation. However, with proactive care and effective communication, dayshift hospice RN case managers can play a crucial role in reducing after-hour calls and providing better support to patients and their families. Here’s how:

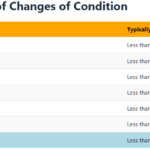
Recognizing the velocity of changes in a patient's condition is crucial for hospice nurses. By understanding the pace of changes in vital signs, symptoms, functionality, and more, nurses can anticipate needs, adjust care plans, and communicate the prognosis effectively with patients and families. The article provides guidelines on interpreting the velocity to estimate the time a patient has left.