Significant Signs a Terminally Ill Patient may be Close to Dying
Published on November 1, 2023
Updated on July 6, 2024
Published on November 1, 2023
Updated on July 6, 2024
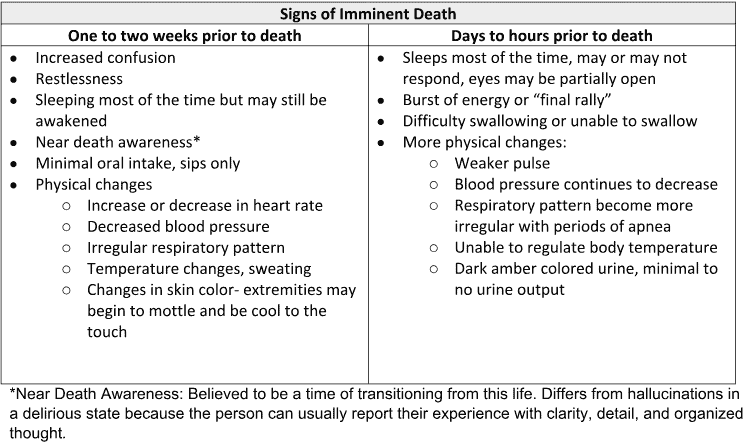
Table of Contents
There are typical visible/audible signs that a person may have less than two weeks to live. Sometimes, when we are so close to someone, we may miss the forest for the trees. Please allow me to go over some significant signs that a person with a terminal illness may have two weeks or less to live.
One of the most noticeable signs that a person may have less than two weeks to live is a sudden onset of symptoms within 24 hours. These symptoms may include (family members seeing these signs should reach out to their hospice provider’s 24×7 number):
These symptoms are typically tell-tale signs that, outside of an infection, the disease progression has taken a sudden turn, such that the patient may die at any moment and up to two weeks later. They indicate that the patient’s vital organs, such as the heart, lungs, kidneys, liver, and brain, are shutting down and failing. They also indicate that the patient is experiencing a lot of physical and emotional distress and needs more care and support.
| Frequency of Change | Typically Means Death Within |
|---|---|
| One every 4 to 8 weeks | Less than 6 months |
| Every 3 to 4 weeks | Less than 3 months |
| Every 1 to 2 weeks | Less than 2 months |
| Once every week | Less than 1 month |
| Several times per week | Less than 2 Weeks |
| Every day | Less than 1 Week |
| Several times per day | Less than 72 hours |
Suppose the patient is determined to be at a point of dying anytime within two weeks or less. In that case, the hospice nursing frequency should be adjusted to optimally support the patient and family as the patient heads towards a good death.
Recognizing the signs that a terminally ill patient may be close to dying is crucial for providing optimal end-of-life care. The visible and audible signs such as generalized discomfort, dysphagia, lethargy, restlessness, skin mottling, dusky complexion, hyperventilation, and multiple falls within a short period can indicate that the patient may have two weeks or less to live. These signs, along with changes in appearance, sleep patterns, and vital signs, are important indicators of the patient’s condition.
As a hospice registered nurse case manager, it’s essential to be vigilant in assessing these signs and symptoms and to work closely with caregivers and the hospice team to provide the necessary support and care for the patient and their family. Understanding these signs can help adjust the nursing frequency to ensure patients receive the best care as they approach the end of life.
By being aware of these significant signs and symptoms, caregivers, family members, and healthcare professionals can work together to ensure that the terminally ill patient’s final days are as comfortable and peaceful as possible. This knowledge empowers everyone involved to provide compassionate, person-centered care, essential in the journey towards a good death.
Remember, each patient’s experience is unique, and individual factors, such as their specific illness and treatments, can influence their signs and symptoms as they approach death. Therefore, it’s essential to approach each situation with empathy, understanding, and a commitment to providing the best possible care for the patient and their loved ones.
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death