Category: Symptom Management
Articles relating to managing symptoms of terminally ill patients with the goal of maintaining comfort through the natural dying process.
Articles relating to managing symptoms of terminally ill patients with the goal of maintaining comfort through the natural dying process.

Lymphedema is a chronic condition that affects millions of people worldwide, especially those who have undergone cancer treatment or have other lymphatic disorders. It occurs when the lymphatic system, which drains excess fluid and waste from the tissues, is damaged or blocked. The most common symptom of lymphedema is swelling of the affected limb, which can range from mild to severe. Lymphedema can have a significant impact on the quality of life of patients with serious illnesses, such as cancer, heart failure, or chronic kidney disease. In this article, we will discuss hospice best practices for the management of lymphedema, with a focus on the needs and preferences of terminally ill patients, family members, and caregivers.

This article aims to overview Pennsylvania medication technicians' training and certification process and discuss specific skills and knowledge needed to perform their duties effectively and safely.

Explore the complex decision of using antibiotics in end-of-life care. This article weighs the potential benefits against risks, considering comfort, quality of life, and ethical concerns. Learn how to make informed choices with your healthcare team for compassionate, patient-centered care in life's final stages.

Explore why side effects from medications can emerge after initial use and understand the critical need for vigilant monitoring and regular medication reconciliation to ensure patient safety and efficacy.
Learn about uncommon opioid side effects like myoclonus and hyperalgesia, and how they impact you and your family. This guide explains these conditions, offers tips for managing them, and highlights the role of hospice in providing comfort and support.

In this episode of Hospice Explained, host Marie Betcher, RN, interviews Nurse Peter Abraham. Peter shares his extensive experience in cardiac telemetry, skilled nursing, and rural home hospice care. They discuss the significance of early hospice enrollment, the challenges of caring for dementia and Parkinson's patients, and the impactful personal stories from Peter's career. Special focus is given to the educational resources on Peter's website, Compassion Crossing, which aims to support families, caregivers, and new hospice nurses. Peter emphasizes the importance of compassion and understanding in hospice care and reflects on how his faith informs his practice.

Hospice nurses are crucial in comforting and supporting patients nearing death and their families. This article explores what to expect from hospice care, focusing on patient assessments, educational discussions, and addressing common family concerns.
Discover how oral ketamine is emerging as a game-changer in palliative care, offering rapid relief for severe depression, anxiety, and emotional distress. This comprehensive guide explores its potential benefits, administration methods, and important considerations for patients and healthcare providers.

Discover how "poop muffins" and "power pudding" can help maintain regular bowel movements. These fiber-rich recipes are especially beneficial for those experiencing constipation, including the elderly and individuals on certain medications. Learn how to make these tasty, digestive-friendly treats at home.

Understanding bowel movements in terminally ill patients is crucial for their comfort and dignity. This guide offers practical tips for caregivers and hospice nurses to manage constipation, diarrhea, and other bowel issues, ensuring patients' better quality of life.

Explore comprehensive approaches to managing hallucinations in loved ones with dementia. This article covers pharmacological methods, focusing on Seroquel and non-drug strategies such as Naomi Feil's validation therapy. Learn how to validate feelings, de-escalate fear, and improve the quality of life for those experiencing cognitive impairment.

End-of-life wound care is crucial for patient comfort and dignity. This guide covers practical tips for preventing infection, managing symptoms, and supporting caregivers during this sensitive time. Learn how to make wound care a compassionate part of hospice and palliative care.

Discover effective strategies for managing end-of-life crises in hospice care. Learn how to recognize signs of distress, implement calming techniques, and provide compassionate support to patients and families. This guide offers practical tips for hospice nurses and caregivers to navigate challenging situations with confidence and empathy.
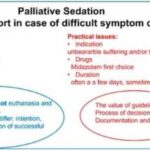
This guide covers the essentials of palliative sedation for hospice patients, including ethical dilemmas, timing, recommended medications, and monitoring effectiveness, ensuring comfort during the end-of-life journey.

Managing bowel problems in terminally ill patients is crucial for their comfort and dignity. This guide offers practical tips for caregivers and hospice nurses to address constipation, diarrhea, bowel obstruction, and ascites, ensuring patients' better quality of life.
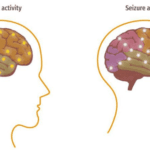
This article delves into the intricate relationship between dementia and seizures, offering insights on identification, safety protocols, and advocacy for caregivers.
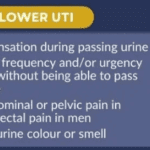
This comprehensive guide helps caregivers understand why urinary tract infections (UTIs) are prevalent in dementia patients. It provides practical advice on prevention, early detection, and effective treatment strategies. Empower yourself with the knowledge to provide the best care for your loved ones.
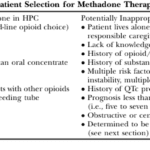
This article delves into the advantages of Methadone over Morphine for pain management in hospice settings. It covers dosage, titration, side effects, and scenarios where Methadone may not be the best choice. Ideal for hospice professionals and caregivers seeking compassionate pain relief options for the terminally ill.

This article is crafted with heartfelt understanding and care, recognizing the challenges you face as caregivers and family members of terminally ill loved ones. Our goal is to empower you with knowledge and practical advice to manage the risk of aspiration pneumonia, a common yet often preventable complication in hospice care.

If you or someone you love is facing a terminal illness, you may feel overwhelmed by the physical, emotional, and spiritual challenges that come with it. You may wonder how to cope with the pain, the fear, the grief, and the loss of control. You may also want to find ways to make the most of the time you have left and to leave a lasting legacy for your loved ones.
Music therapy is a form of therapy that can help you and your family deal with these issues. It involves using music and musical activities to improve the health and well-being of people of all ages and backgrounds. Music therapy can help you express your feelings, communicate with others, relax your body and mind, cope with pain and stress, enhance your spiritual connection, and create a meaningful life story.

Discover how Lion’s Mane, Magnesium Glycinate, Vitamins D3, K2, B1, Folate, C, and MTC Oil can play a role in dementia care. This article delves into the latest research and expert insights on natural supplements that support cognitive function and overall brain health.

Explore the use of ashwagandha and CBD to ease anxiety in dementia patients. Learn about dosages, safety precautions, and real-life stories.
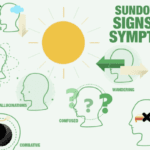
Sundowning, or "late-day confusion," is a challenging experience for individuals with dementia and their caregivers. This phenomenon, occurring in the late afternoon or evening, brings about increased confusion, anxiety, and agitation. Caregivers need to comprehend sundowning and offer compassionate care to ensure the well-being of their loved ones. This article delves into effective pharmacological and non-pharmacological strategies to manage sundowning and create a safe environment.

Discover the potential side effects of dementia medications and how to support your loved one.