Introduction
When you turn 18, you gain the legal right to make your own medical decisions. Whether you’re a college freshman, a new parent in your thirties, or approaching retirement, that fundamental adult responsibility remains unchanged. Yet while most of us diligently handle other adult tasks—paying bills, voting, maintaining insurance—there’s one critical responsibility that too many adults completely overlook.
Adult Responsibility: More Than Paying Bills and Voting
True adult responsibility extends far beyond managing your finances or participating in elections. It means taking control of your future, especially when you might not be able to speak for yourself. Consider Sarah, a healthy 25-year-old teacher who suffered a traumatic brain injury in a car accident, or Robert, a 45-year-old father who had an unexpected stroke during his morning jog. Both were vibrant, healthy adults who never imagined they’d be unable to communicate their medical wishes.
Every adult—regardless of age, health status, or life stage—faces the possibility of medical incapacity. This reality doesn’t discriminate between the 22-year-old recent graduate starting their first job and the 65-year-old enjoying an active retirement. Heart attacks, accidents, sudden illnesses, and unexpected diagnoses can happen to anyone at any time.
The Shocking Truth: Most Adults Lack Proper Advance Directives
Here’s the reality that might surprise you: fewer than 40% of American adults have any form of advance directive. Even more concerning, many of those with outdated documents no longer reflect their current wishes, family situation, or state of residence.
Think about how much your life has changed in the past few years. Perhaps you’ve:
- Started or ended a significant relationship
- Changed jobs or moved to a different state
- Experienced health changes or new diagnoses
- Had children or become responsible for aging parents
- Shifted your personal values or spiritual beliefs
If your advance directive has not kept pace with these changes, it may not truly represent your current wishes when you need them most.
Why This Should Be Among Your First Adult Priorities
An advance directive isn’t just a legal document—it’s your voice when you can’t speak. Without proper planning, your loved ones may face agonizing decisions during already stressful medical emergencies. They might disagree about what you would want, leading to family conflict at the worst possible time. Even worse, medical professionals may be legally required to provide treatments you would never choose, simply because no one knows your preferences.
Creating and maintaining a current, comprehensive advance directive should rank alongside other essential adult responsibilities like:
- Maintaining health insurance
- Creating an emergency fund
- Updating your will or estate planning
- Regular medical and dental checkups
The difference is that advance directives protect both you and your loved ones from unnecessary suffering and difficult decisions. They ensure your personal values guide your medical care, even when you can’t communicate them yourself.
The best time to create your advance directive is now—while you’re healthy, thinking clearly, and able to have thoughtful conversations with your loved ones. Whether you’re 18 or 80, single or married, healthy or managing chronic conditions, taking control of your medical future is one of the most caring things you can do for yourself and those who love you.
The Universal Need: Why Every Adult Requires an Advance Directive
Life is Unpredictable at Any Age
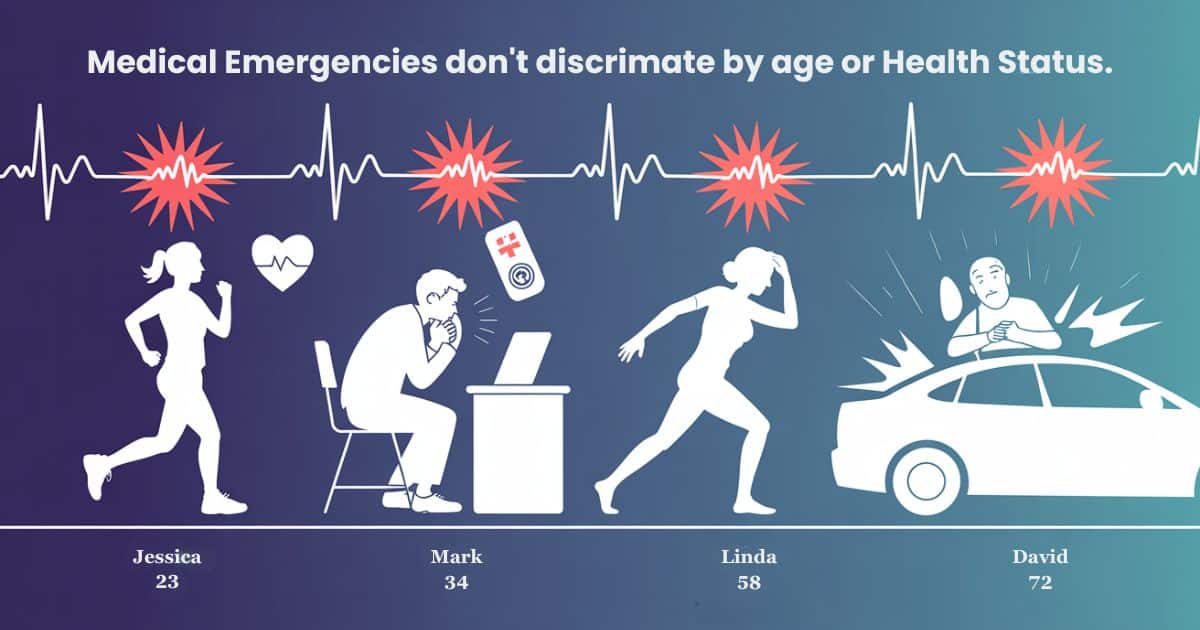
Medical Emergencies Don’t Discriminate by Age or Health Status
Life can change in an instant, and medical crises don’t check your birth certificate first. Consider these real-world scenarios that happen every day across America:
- Jessica, a 23-year-old marathon runner, collapsed during her morning training run due to an undiagnosed heart condition.
- Mark, a 34-year-old software engineer and father of two, suffered a severe allergic reaction that left him unconscious for weeks.
- Linda, a 58-year-old yoga instructor in excellent health, experienced a massive stroke while teaching her evening class.
- David, a 72-year-old retiree, was involved in a multi-car accident while driving to visit his grandchildren.
Each of these individuals considered themselves healthy and active. No one is expected to lose the ability to make medical decisions suddenly. Yet each found themselves—or their families—facing complex medical choices without clear guidance about their wishes.
Young Professionals, Parents, and Seniors All Face Risks
Every life stage brings unique vulnerabilities that make advance directives essential:
Young Adults (18-30s):
- Sports injuries and accidents during active lifestyles
- Mental health crises requiring hospitalization
- Complications from routine medical procedures
- Sudden onset of chronic conditions like diabetes or autoimmune diseases
Parents and Mid-Career Adults (30s-50s):
- Work-related stress leading to heart attacks or strokes
- Cancer diagnoses during routine screenings
- Accidents while traveling for business or family activities
- Autoimmune conditions that can flare unexpectedly
Older Adults (60+):
- Progressive conditions like dementia or Parkinson’s disease
- Increased surgical risks during routine procedures
- Multiple chronic conditions that can suddenly worsen
- Higher likelihood of falls and fractures leading to complications
Real Stories: When the Unexpected Happens
Maria, a 28-year-old nurse, always helped others plan for medical emergencies but never created her own advance directive. When she developed sudden, severe pneumonia that required life support, her parents and boyfriend disagreed about her treatment preferences. Without clear documentation of her wishes, her family spent precious days arguing instead of focusing on her recovery.
Tom, a 45-year-old contractor, suffered a traumatic brain injury at a job site. His wife knew he valued his independence above all else, but his teenage children wanted “everything possible” done to save their father. The family’s disagreement created lasting rifts during an already devastating time.
These stories repeat themselves in hospitals across the country every single day. The common thread isn’t age, health status, or lifestyle—it’s the absence of clear, documented medical wishes.
The Cost of Waiting
Family Conflicts Over Medical Decisions
When you don’t have an advance directive, your loved ones become unwilling decision-makers during the worst possible circumstances. Family members often discover they have vastly different ideas about what you would want:
- Your spouse might prioritize comfort care while your parents insist on aggressive treatment
- Adult children may disagree among themselves about life-sustaining treatments
- Religious differences within families can create additional tension
- Blended families may struggle with who has the legal authority to decide
These conflicts don’t just cause temporary stress—they can permanently damage family relationships. Siblings may never speak again after disagreeing about a parent’s care. Spouses might resent in-laws who overruled their judgment. Children may carry guilt for years about decisions they were forced to make.
Financial Burden of Prolonged Care Without Clear Wishes
Medical care without clear guidance often defaults to the most expensive option: doing everything possible. This approach can quickly become financially devastating:
- Life-sustaining treatments in intensive care can cost thousands of dollars per day
- Long-term care facilities for patients in vegetative states can exceed $100,000 annually
- Families may exhaust savings, retirement funds, and college accounts
- Medical bankruptcy affects hundreds of thousands of American families each year
Consider the hidden costs beyond medical bills:
- Family members taking unpaid leave from work to make daily medical decisions
- Travel and accommodation expenses for out-of-town relatives
- Legal fees if family members disagree and seek court intervention
- The emotional and financial stress can devastate entire families for generations
Emotional Trauma for Loved Ones Making Impossible Choices
Perhaps the heaviest cost of waiting is the emotional burden placed on your loved ones. Without your clear guidance, they face agonizing questions:
- “Would Mom want to live this way?”
- “Did Dad ever talk about being on life support?”
- “Are we giving up too soon, or holding on too long?”
The psychological impact extends far beyond the immediate crisis:
- Guilt and second-guessing can last for years after your recovery or death
- Anxiety and depression among family members who questioned their decisions
- Post-traumatic stress from making life-and-death choices without guidance
- Relationship damage occurs when family members blame each other for difficult decisions
Your children, spouse, parents, or siblings never asked to become medical decision-makers. By creating a comprehensive advance directive, you lift this impossible burden from their shoulders and allow them to focus on what matters most: supporting you and each other during a difficult time.
The universal need for advance directives isn’t about age, health, or lifestyle—it’s about taking responsibility for your own medical future while protecting the people you love from unnecessary anguish. Every adult, from recent college graduates to great-grandparents, deserves the peace of mind that comes with proper planning.
The 3-6 Month Rule: Keeping Your Directive Current
Why “Current” Matters More Than “Complete”
Having an outdated advance directive can be worse than having none at all. Your advance directive from five years ago might reflect a completely different person—someone with different relationships, health status, living situation, and values. When medical professionals and family members follow outdated instructions, they may be honoring wishes that no longer represent who you are today.
Life Changes That Require Updates Across All Adult Stages
Your advance directive should grow and change as you do. Think about how much your life has evolved in recent years. The preferences you had as a single 25-year-old might drastically differ from your wishes as a married 30-year-old parent. Similarly, the medical choices that seemed right when you were healthy at 50 may change after receiving a chronic illness diagnosis at 55.
Regular reviews every 3-6 months ensure your directive stays aligned with your current reality. This isn’t about major overhauls each time—often it’s simple updates like contact information, healthcare proxy changes, or refining your preferences based on new life experiences.
Career Changes, Marriages, Divorces, and New Relationships
Relationship changes create some of the most critical updates needed in advance directives:
New Marriages or Partnerships:
- Your spouse typically becomes your default healthcare proxy under state law
- Previous designations of parents or siblings may need updating
- Financial responsibility for medical decisions shifts to your partner
- Insurance coverage and benefits may change significantly
Divorces and Separations:
- Remove your ex-spouse immediately from all healthcare decision-making roles
- Update emergency contacts and beneficiary information
- Reconsider who you trust to make difficult medical choices
- Review any shared financial responsibilities for medical care
New Serious Relationships:
- Decide whether your partner should have decision-making authority
- Consider how your family might react to your partner making medical choices
- Update contact information and relationship status with healthcare providers
Health Status Changes and New Diagnoses
Your medical reality directly impacts your advance directive preferences. A diabetes diagnosis might change your feelings about artificial nutrition. A family history of dementia might prompt you to add specific cognitive decline instructions. Cancer survivorship could shift your perspective on aggressive treatments versus comfort care.
Key health changes requiring immediate updates:
- New chronic conditions like diabetes, heart disease, or autoimmune disorders
- Mental health diagnoses that might affect decision-making capacity
- Family medical history discoveries that change your risk factors
- Medication allergies or adverse reactions discovered during treatment
- Previous hospitalizations that gave you insight into your treatment preferences
Moving to Different States With Varying Laws
State laws governing advance directives vary significantly across the country. What’s legally valid in California might not meet requirements in Texas. Each time you move, you need to verify your directive meets your new state’s legal standards.
Common state-by-state differences include:
- Number of witnesses required for document signing
- Whether witnesses can be related to you or named in your will
- Notarization requirements and acceptable alternatives
- Specific language is required for certain medical decisions
- Recognition of directives created in other states
Professional tip: When relocating, contact an end-of-life doula in your new state to review your existing documents and identify any necessary updates before you need medical care.
Common Life Transitions Requiring Updates
Young Adults: College, First Jobs, Serious Relationships
The transition from teenager to independent adult creates multiple opportunities for advance directive updates:
Starting College (18-22):
- Update emergency contacts as you become more independent from your parents
- Consider campus health services and local hospital preferences
- Address potential mental health crises common during college years
- Include preferences about family notification during medical emergencies
First Jobs and Career Launches (22-28):
- New employer health insurance may change your preferred hospitals and doctors
- Career-related travel might require broader geographic healthcare considerations
- Financial independence changes who pays for medical decisions
- Student loan debt might influence preferences about expensive treatments
Serious Dating Relationships (20s-30s):
- Decide when a romantic partner should have input on medical decisions
- Update emergency contacts to include significant others
- Consider how your family might react to a partner making healthcare choices
- Address potential conflicts between family and partner preferences
Mid-Life Adults: Marriage, Children, Career advancement, Aging Parents
Midlife brings complex relationships and responsibility changes that directly impact medical decision-making:
Marriage and Partnership:
- Legally designate your spouse as the primary healthcare decision-maker
- Combine or coordinate advance directives with your partner’s wishes
- Address potential religious or cultural differences in medical preferences
- Update all medical providers and insurance companies with new information
Becoming Parents:
- Consider how medical decisions affect your children’s future
- Address preferences for life-sustaining treatment when you have dependents
- Designate backup caregivers for minor children during medical crises
- Update financial considerations to include children’s needs and education costs
Career Advancement and Geographic Mobility:
- Executive positions might consist of travel to areas with different medical facilities
- Higher income levels might change your perspective on expensive treatments
- Increased stress levels could impact your risk for certain medical conditions
- Corporate insurance plans may offer different healthcare options
Caring for Aging Parents:
- Your own medical preferences may evolve as you witness your parents’ healthcare decisions
- Increased understanding of long-term care costs and quality issues
- Experience with family medical decisions that inform your own wishes
- Time constraints from caregiving that affect your availability for medical appointments
Older Adults: Retirement, Health Changes, Loss of Spouse
Later-life transitions often bring the most significant advance directive updates:
Retirement Transitions:
- Medicare enrollment changes healthcare provider options and coverage
- Fixed incomes might influence preferences about expensive treatments
- More time for medical appointments, but potentially reduced access to employer benefits
- Geographic relocation to retirement communities or different climates
Progressive Health Changes:
- New diagnoses like diabetes, heart disease, or osteoporosis affect treatment preferences
- Medication interactions become more complex with multiple prescriptions
- Mobility limitations might change preferences about rehabilitation and recovery
- Cognitive changes could affect your ability to make future medical decisions
Loss of Life Partners:
- Immediate update of the healthcare proxy to adult children or other trusted individuals
- Reconsider treatment preferences without your primary support person
- Address preferences for social isolation and depression, which are common after spousal loss
- Update financial considerations for medical care as a single person
The key to successful advance directive maintenance isn’t perfection—it’s consistency. Set a recurring reminder every three months to review your document, even if no significant changes seem necessary. Significant life shifts often add to substantial changes in your medical preferences over time. By staying current, you ensure that your advance directive truly represents your wishes when you need it most.
Beyond Basic Living Wills: What Complete Coverage Looks Like
Most people think an advance directive is just about “pulling the plug.” That’s only the beginning. A truly comprehensive advance directive addresses dozens of medical scenarios you might never have considered—from pain management preferences to social media access during extended illness. The goal is to create a complete picture of your values and wishes that guides medical professionals and loved ones through any situation.
The Foundation Decisions
Quality of Life vs. Prolonging Life: Defining What Matters to You
This is the most personal decision in your entire advance directive. What makes life meaningful to you? For some adults, simply being alive—regardless of mental capacity—holds immense value. For others, the ability to recognize loved ones, communicate, or maintain independence defines a life worth living.
Consider these real-world scenarios across different life stages:
Young Adult Perspective (20s-30s):
- Would you want life support if it meant never returning to your career or athletic activities?
- How important is your ability to travel, socialize, or pursue hobbies?
- What role does physical appearance play in your self-image and quality of life?
Mid-Life Adult Considerations (40s-50s):
- Would you want aggressive treatment if it meant missing your children’s important milestones?
- How do your responsibilities as a caregiver for aging parents affect your medical choices?
- What level of cognitive function would you need to continue meaningful relationships?
Older Adult Reflections (60s+):
- After a full life, what experiences would make continued living worthwhile?
- How important is maintaining your role as family patriarch or matriarch?
- What level of physical independence would you require to feel fulfilled?
Key questions to address in your directive:
- Define what “meaningful recovery” means to you personally
- Specify circumstances where you would want treatment stopped
- Identify non-negotiable aspects of quality of life that matter most
- Address how your values might change if you develop dementia or other cognitive decline
Pain Management Philosophy: Maximum Comfort vs. Mental Clarity
Your pain management preferences reveal deep personal values about consciousness, communication, and comfort. Some adults prioritize staying alert enough to interact with family, even if it means experiencing some discomfort. Others want maximum pain relief, regardless of how it affects their mental clarity.
Your directive should address:
Aggressive Pain Management:
- Use whatever medications are necessary to keep you comfortable
- Prioritize comfort over consciousness during end-of-life care
- Accept that strong pain medications might hasten death
- Focus on palliative care rather than curative treatments
Moderate Pain Management:
- Balance comfort with the ability to communicate with loved ones
- Take enough pain medication to function but remain alert
- Adjust medication levels based on your ability to interact meaningfully
- Maintain some level of consciousness for important conversations
Minimal Intervention:
- Use pain medication only when absolutely necessary
- Prioritize mental clarity over physical comfort
- Accept higher levels of discomfort to remain fully aware
- Focus on non-medication pain management techniques when possible
Communication Preferences: When You Can’t Speak for Yourself
How do you want medical information handled when you cannot participate in conversations? These preferences become crucial during extended illnesses, surgical recoveries, or progressive conditions affecting your communication ability.
Family Communication Guidelines:
- Who should receive medical updates and in what detail?
- Should children be included in medical discussions regardless of age?
- How should medical information be shared with extended family and friends?
- What role should your religious or spiritual community play in your care?
Social and Professional Considerations:
- Should your employer be notified about your medical condition?
- How much privacy do you want regarding your illness or treatment?
- What level of social media sharing is acceptable about your condition?
- Should friends and colleagues be encouraged or discouraged from visiting?
Medical Intervention Specifics
Artificial Nutrition and Hydration: Feeding Tubes and IV Fluids
These interventions can sustain life for months or years when you cannot eat or drink naturally. Your preferences about artificial nutrition and hydration require careful consideration of various scenarios and your personal values about quality of life.
Feeding Tubes (Percutaneous Endoscopic Gastrostomy or PEG tubes):
- Surgically placed tubes that deliver nutrition directly to your stomach
- Can maintain life indefinitely for people in vegetative states or with severe dementia
- Consider your preferences for temporary feeding during recovery vs. permanent nutrition support
- Address comfort care alternatives that focus on small amounts of food for pleasure rather than sustenance
Intravenous Fluids:
- Can prevent dehydration and maintain basic body functions
- Less invasive than feeding tubes, but still requires ongoing medical intervention
- Decide whether you want IV fluids during end-of-life care or prefer the natural dying process
- Consider comfort measures like moistened mouth swabs instead of IV hydration
Dialysis and Organ Support: Long-Term Life-Sustaining Treatments
These interventions can extend life significantly but require ongoing medical commitment and lifestyle changes. Your advance directive should address both emergency situations and long-term treatment preferences.
Dialysis for Kidney Failure:
- It can sustain life for years when the kidneys stop functioning
- Requires multiple weekly treatments at medical facilities
- Consider whether you want dialysis initiated during emergency situations
- Address preferences for trying dialysis temporarily vs. committing long-term
Heart Support Devices:
- Mechanical devices that can maintain heart function
- Range from temporary measures during surgery recovery to permanent implants
- Specify your preferences for artificial heart devices during different life stages
- Consider how these interventions align with your quality of life values
Breathing Assistance: Ventilators and Respiratory Support
Mechanical breathing support ranges from temporary assistance during surgery to permanent life support. Your preferences about respiratory interventions should address both short-term and long-term scenarios.
Mechanical Ventilation:
- Machines that breathe for you when you cannot breathe independently
- Can be temporary during illness recovery or permanent for chronic conditions
- Decide whether you want ventilator support initiated during emergencies
- Address preferences for time-limited trials vs. indefinite mechanical breathing
Non-Invasive Breathing Support:
- Includes oxygen therapy, CPAP machines, and BiPAP devices
- Less invasive than mechanical ventilation, but still provides life-sustaining support
- Consider your comfort level with various types of breathing assistance
- Address preferences for home-based vs. hospital-based respiratory care
Blood Products and Medications: Transfusions and Antibiotics
These common medical interventions can be life-saving but may conflict with personal, religious, or cultural beliefs. Your advance directive should clearly state your preferences about blood products and aggressive medical treatments.
Blood Transfusions:
- It can be essential during surgery, cancer treatment, or trauma care
- Some religious beliefs prohibit blood transfusions under any circumstances
- Consider preferences for blood alternatives and synthetic blood products
- Address emergency transfusion preferences when your life is immediately threatened
Antibiotics and Infection Treatment:
- Can cure serious infections, but may prolong the dying process during end-of-life care
- Decide whether you want aggressive infection treatment during terminal illness
- Consider comfort-focused antibiotic use vs. curative treatment goals
- Address preferences for treating infections that develop during palliative care
Specialized Advance Directives for Modern Challenges
Dementia Advance Directives: Planning for Cognitive Decline
Dementia affects millions of adults and creates unique challenges for medical decision-making. Traditional advance directives may not address the specific issues that arise during cognitive decline, making specialized dementia directives essential for comprehensive planning.
Early-Stage Dementia Preferences:
- Level of disclosure you want about your diagnosis and prognosis
- Preferences for maintaining independence vs. accepting help with daily activities
- Decision-making about driving, financial management, and living arrangements
- Treatment preferences for conditions that might accelerate cognitive decline
Advanced Dementia Considerations:
- Define what constitutes a meaningful quality of life during severe cognitive impairment
- Address preferences for artificial nutrition when you can no longer eat safely
- Specify comfort care preferences when you no longer recognize loved ones
- Consider VSED options during the early stages while you still have capacity
Mental Health Advance Directives: Psychiatric Crisis Planning
Mental health crises can temporarily impair your decision-making capacity just like physical medical emergencies. Psychiatric advance directives ensure your preferences guide treatment during mental health episodes across all adult age groups.
Crisis Intervention Preferences:
- Preferred hospitals and mental health professionals for emergency psychiatric care
- Medications you want to avoid due to previous adverse reactions
- Treatment approaches that have been effective or harmful in the past
- Contact persons who understand your mental health history and preferences
Treatment Philosophy:
- Preferences for inpatient vs. outpatient treatment during crisis
- Role of family members in mental health decision-making
- Religious or cultural considerations for psychiatric treatment
- Integration of mental health care with other medical treatments
VSED (Voluntarily Stopping Eating and Drinking) Directives: Comprehensive End-of-Life Choices
VSED represents a legal option for hastening death by refusing food and water. This approach requires careful planning and clear documentation to ensure your wishes are respected and your loved ones receive appropriate support.
VSED Considerations:
- Specific conditions that would prompt you to consider VSED
- Medical and emotional support you want during the VSED process
- Role of hospice care and palliative care professionals
- Family support and communication preferences
Legal and Practical Planning:
- Documentation required to ensure healthcare providers respect your VSED decision
- Advance planning for comfort care during the VSED process
- Address potential family conflicts about your VSED choice
- Integration with other advance directive preferences
Technology and Social Media: Digital Legacy Considerations
Modern medical crises extend into digital spaces in ways previous generations never considered. Your advance directive should address technology use, social media management, and digital communication during extended illness.
Digital Communication:
- Who should manage your social media accounts during extended illness?
- Preferences for sharing health updates online
- Access to email, banking, and other password-protected accounts
- Management of professional online presence during medical leave
Technology in Healthcare:
- Preferences for telemedicine vs. in-person medical appointments
- Use of medical monitoring devices and health apps
- Privacy preferences for electronic medical records
- Integration of digital tools with traditional medical care
Expert Resource
For adults seeking comprehensive guidance on creating thorough advance directives, Beyond the Living Will: Creating Effective Advance Directives offers detailed information on all aspects of advance care planning. This resource addresses the complex scenarios and specialized directives discussed above, providing practical guidance for adults at every life stage who want to ensure their medical wishes are clearly documented and legally protected.
The key to complete advance directive coverage isn’t addressing every possible scenario—it’s clearly communicating your values and preferences so that medical professionals and loved ones can make decisions that honor your wishes, even in situations you never specifically anticipated.
Professional Support: How End-of-Life Doulas Can Help
When most people hear “end-of-life doula,” they picture someone who only works with dying patients. That common misconception prevents many healthy adults from accessing valuable support. End-of-life doulas are trained professionals who help people navigate medical decision-making throughout their adult lives—not just during their final days.
More Than End-of-Life Specialists
Training in Advance Directive Completion for All Adults
End-of-life doulas receive extensive training in advance care planning that goes far beyond basic living will forms. They understand the complex medical, legal, and emotional aspects of healthcare decision-making affecting adults at every stage.
Professional doula training includes:
- Understanding medical terminology and treatment options
- Knowledge of state-specific legal requirements for advance directives
- Techniques for facilitating difficult conversations about medical preferences
- Cultural competency for diverse family structures and belief systems
- Crisis intervention skills for family conflicts over medical decisions
Whether you’re a 25-year-old starting your first job or a 65-year-old planning retirement, doulas can help you create comprehensive advance directives that reflect your current life situation and values. They work with healthy adults who want to plan ahead, not just people facing terminal diagnoses.
Unbiased Guidance Through Complex Medical Decisions
One of the most valuable aspects of working with an end-of-life doula is their neutrality. Unlike family members who may have emotional investments in your medical decisions, doulas provide objective guidance based on your expressed values and preferences.
Consider these common family dynamics that doulas help navigate:
Young Adults (20s-30s):
- Parents who struggle to accept their adult child’s medical independence
- Romantic partners versus family conflicts over decision-making authority
- Religious differences between generations about medical interventions
- Financial considerations when parents are still providing health insurance
Mid-Life Adults (40s-50s):
- Spouses who disagree about aggressive treatment preferences
- Adult children who have different opinions about their parents’ care wishes
- Blended family complications with multiple sets of children and ex-spouses
- Career considerations that family members may not fully understand
Older Adults (60s+):
- Adult children who can’t agree among themselves about their parents’ wishes
- Second marriages create conflicts between the current spouse and the biological children
- Long-term friendships that feel like family but lack legal standing
- Religious community involvement that may influence family dynamics
Emotional Support During Difficult Conversations
Creating an advance directive forces you to confront your own mortality—a challenging process at any age. Doulas provide emotional support and practical guidance for these difficult conversations, helping you work through complex feelings about medical treatments, death, and dying.
Doulas help you process:
- Fear and anxiety about losing control over medical decisions
- Guilt about potential burdens on family members
- Uncertainty about medical treatments you’ve never experienced
- Grief about acknowledging your own mortality and vulnerability
The Value of Expert Assistance
Understanding Medical Terminology and Implications
Medical decisions involve complex terminology and treatment implications that can be overwhelming for people without healthcare backgrounds. End-of-life doulas translate medical jargon into understandable language and help you understand the real-world consequences of different treatment choices.
Examples of complex medical concepts doulas explain:
Artificial nutrition and hydration:
- What PEG tubes actually involve and how they affect daily life
- Differences between temporary and permanent feeding interventions
- Comfort care alternatives that focus on quality rather than prolonging life
- Legal and ethical implications of refusing artificial nutrition
Mechanical ventilation:
- Various types of breathing support, from CPAP machines to full life support
- What “being on a ventilator” actually means for consciousness and communication
- Time-limited trials versus indefinite mechanical breathing support
- Weaning processes and realistic expectations for recovery
Palliative care versus hospice care:
- When palliative care is appropriate for people who aren’t dying
- Insurance coverage differences between curative and comfort-focused care
- Integration of palliative approaches with ongoing medical treatments
- Family education about comfort care that doesn’t mean “giving up”
Navigating Family Dynamics and Disagreements
Family conflicts over medical preferences can tear relationships apart during already stressful times. Doulas are skilled in family mediation and communication techniques that help families work through disagreements before medical crises occur.
Common family conflicts doulas help resolve:
Decision-Making Authority:
- Who should be designated as a healthcare proxy when multiple family members want the role
- How to handle situations where legal next-of-kin isn’t the person you trust most
- Balancing family input with personal autonomy over medical decisions
- Managing expectations when family members disagree with your choices
Religious and Cultural Differences:
- Navigating conflicts between traditional family beliefs and personal medical preferences
- Respecting cultural values while asserting individual choice
- Addressing religious concerns about specific medical interventions
- Finding compromise when family members hold different spiritual beliefs
Geographic and Logistical Challenges:
- Coordinating medical decision-making when family members live far apart
- Managing communication during medical crises across time zones
- Addressing practical concerns about who can physically be present for medical decisions
- Planning for scenarios where primary decision-makers are unavailable
Ensuring Comprehensive Coverage of All Scenarios
Most people create basic advance directives that only address obvious scenarios like terminal illness or vegetative states. Doulas help you think through less obvious but equally critical medical situations that could affect your care.
Comprehensive scenarios doulas help you address:
Mental Health Crises:
- Psychiatric advance directives for depression, anxiety, or bipolar episodes
- Preferences for involuntary hospitalization during mental health emergencies
- Medication preferences based on previous experiences with psychiatric treatments
- Integration of mental health care with other medical decision-making
Dementia and Cognitive Decline:
- Early-stage dementia decision-making while you still have mental capacity
- Preferences for disclosure about cognitive decline diagnoses
- Advanced dementia care preferences when you no longer recognize loved ones
- VSED considerations during the early stages of cognitive impairment
Pregnancy and Reproductive Health:
- Medical decision-making during pregnancy complications
- Preferences for maternal versus fetal health in emergency situations
- Contraception and fertility treatment preferences during incapacity
- Postpartum medical decisions if complications arise after childbirth
When to Seek Doula Support
Creating Your First Advance Directive
If you’ve never created an advance directive, working with a doula provides structure and guidance for what can feel like an overwhelming process. Doulas help break down advance care planning into manageable steps and ensure you don’t overlook essential considerations.
First-time advance directive benefits:
- Education about your options without pressure to make immediate decisions
- Help understanding your state’s specific legal requirements
- Guidance on choosing appropriate witnesses and notarization
- Support for difficult conversations with family members about your choices
Major Life Changes Requiring Updates
Significant life transitions often require substantial updates to advance directives. Doulas can help you navigate these changes and ensure your updated directive reflects your new circumstances and evolved preferences.
Life changes that benefit from doula support:
Relationship Transitions:
- Marriage or divorce requires changes to healthcare proxy designations
- New serious relationships where you’re considering including your partner in medical decisions
- The death of a spouse or life partner requires a complete revision of the decision-making structure
- Blended family formation with complex step-relationships affecting medical choices
Health Status Changes:
- New chronic illness diagnoses that change your treatment preferences
- Recovery from a serious illness gives you a new perspective on medical interventions
- Mental health diagnoses requiring psychiatric advance directive additions
- Family medical history discoveries that affect your risk factors and preferences
Family Conflicts Over Medical Preferences
When family members strongly disagree with your medical preferences, doulas can facilitate conversations and help find solutions that respect your autonomy while maintaining meaningful relationships.
Conflict resolution scenarios:
- Parents who disagree with their adult child’s medical choices
- Spouses with different religious or cultural beliefs about medical interventions
- Adult children who can’t agree among themselves about their parents’ care
- Extended family members who feel their opinions should influence your medical decisions
Complex Medical Histories
Adults with complicated medical backgrounds benefit from doula expertise in creating advance directives that address their specific health challenges and treatment experiences.
Complex medical situations:
- Multiple chronic conditions require coordination between different specialists
- Previous negative experiences with specific treatments or healthcare providers
- Rare medical conditions that most people don’t understand
- Mental health and physical health conditions that interact in complicated ways
Working with an end-of-life doula isn’t about preparing for death—it’s about taking control of your medical future while you’re healthy and able to make thoughtful decisions. Whether you’re 22 or 82, single or married, healthy or managing chronic conditions, professional support can help you create an advance directive that genuinely reflects your values and protects both you and your loved ones from unnecessary confusion and conflict during medical emergencies.
Professional Guidance: End-of-Life Doulas vs. Attorneys
CRITICAL Disclaimer – Nothing in this article constitutes legal or medical advice, but is provided for educational purposes only. Always consult with qualified professionals for your specific situation.
Creating a legally sound advance directive isn’t a do-it-yourself project. The complexity of medical decisions, legal requirements, and emotional implications makes professional guidance essential for every adult. Whether you’re 22 or 82, the stakes are too high to risk getting it wrong. The question isn’t whether you need professional help—it’s choosing the right type of professional support for your situation.
Why Professional Help is Essential
Legal Requirements Are Complex and Vary Significantly by State
Each state has its own intricate web of legal requirements that can make or break the validity of your advance directive. What works perfectly in Florida might be completely invalid in Oregon. These aren’t minor technical differences—they’re fundamental legal requirements determining whether your wishes will be honored during a medical emergency.
Consider Sarah, a 34-year-old marketing manager who moved from Texas to Colorado for a new job. Her Texas advance directive didn’t meet Colorado’s witness requirements, leaving her legally unprotected when she suffered complications during routine surgery. Without professional guidance, she had no idea her directive was invalid in her new state.
State-specific complications include:
- Witness requirements vary from one to three unrelated adults
- Notarization standards that differ significantly between jurisdictions
- Specific language requirements for certain medical decisions
- Recognition policies for directives created in other states
Medical Terminology and Treatment Implications Require Expert Understanding
Medical decisions involve complex terminology and treatment implications that most adults don’t encounter until they’re facing a health crisis. Understanding the difference between palliative care and hospice care, or what artificial nutrition actually involves, requires specialized knowledge that professionals bring to the conversation.
Examples of complex medical concepts that require professional explanation:
Young Adults (20s-30s) often don’t understand:
- What “life support” actually means in terms of daily experience and long-term implications
- The difference between temporary and permanent medical interventions
- How mental health crises might affect medical decision-making capacity
- Insurance implications of different treatment choices
Mid-Life Adults (40s-50s) typically need guidance on:
- Coordination between multiple chronic conditions and treatment preferences
- How medical decisions affect dependent children and family financial security
- Integration of advance directives with disability insurance and estate planning
- Cancer treatment options and quality-of-life considerations
Older Adults (60s+) require understanding of:
- Medicare coverage implications for different types of care
- The progression of dementia and cognitive decline planning
- Realistic expectations for recovery from common age-related medical events
- Coordination with existing medical conditions and medication interactions
Professional Guidance Prevents Costly Legal Mistakes That Can Invalidate Your Directive
A single technical error can make your entire advance directive legally worthless. Improper witness selection, incorrect notarization, or missing required language can leave your family without legal guidance during the worst possible time. Professional guidance ensures every legal requirement is met correctly the first time.
Common costly mistakes professionals prevent:
- Choosing inappropriate witnesses who have conflicts of interest
- Using outdated forms that no longer meet current state requirements
- Missing required signatures, initials, or dating
- Failing to coordinate advance directives with other legal documents properly
Emotional Support During Difficult Conversations About Mortality and Medical Preferences
Creating an advance directive forces you to confront your own mortality—a process that can be emotionally overwhelming at any age. Professionals provide emotional support and facilitate difficult family conversations that many adults avoid indefinitely.
Marcus, a 28-year-old teacher, kept postponing his advance directive because thinking about death felt too scary. Working with an end-of-life doula helped him process his fears while creating a comprehensive directive that gave him peace of mind rather than anxiety.
End-of-Life Doulas: Your First Choice for Most Adults
Comprehensive Training Specifically in Advance Directive Completion and Healthcare Decision-Making
End-of-life doulas receive extensive specialized training that focuses specifically on advance care planning, medical decision-making, and family communication. Unlike attorneys who may handle advance directives as one small part of estate planning, doulas specialize in this exact type of healthcare planning.
Doula training includes:
- Medical terminology and treatment option education for non-healthcare professionals
- State-specific legal requirements for advance directives
- Family communication and conflict resolution techniques
- Cultural competency for diverse religious and ethnic backgrounds
- Crisis support for families facing difficult medical decisions
Deep Understanding of Both Medical Terminology and Legal Requirements
Doulas bridge the gap between medical complexity and legal requirements in ways that most other professionals cannot. They understand what medical treatments actually involve from a patient experience perspective while ensuring all legal requirements are properly met.
Examples of doula expertise in action:
For Young Professionals:
- Explaining how psychiatric advance directives work for mental health crises
- Helping navigate family dynamics when parents disagree with their adult child’s medical preferences
- Understanding the insurance implications of different treatment choices
- Addressing concerns about career impact from medical decisions
For Growing Families:
- Coordinating advance directives between spouses with different medical preferences
- Addressing how medical decisions affect dependent children and family security
- Understanding pediatric considerations when parents have medical emergencies
- Balancing individual medical wishes with family responsibilities
For Older Adults:
- Explaining Medicare coverage for different types of medical care
- Understanding dementia progression and cognitive decline planning
- Coordinating advance directives with existing chronic condition management
- Addressing end-of-life care preferences with adult children
Cost-Effective Professional Guidance
Professional doula services typically cost $150-400 for complete advance directive assistance, compared to $500-2000+ for attorney consultations. This makes professional guidance accessible for adults at all income levels and life stages.
What doula fees typically include:
- Initial consultation and values clarification discussions
- Complete document preparation and legal requirement compliance
- Witness coordination and notarization arrangement
- Family communication support and education
- Follow-up support for questions and minor updates
Ongoing Relationship for Updates, Maintenance, and Family Support Throughout Your Adult Life
Unlike one-time attorney consultations, doulas provide ongoing professional relationships that evolve with your changing adult life circumstances. This continuity ensures your advance directive stays current and your family remains informed about your preferences.
Ongoing doula support includes:
- Regular review appointments every 3-6 months to assess needed updates
- Life transition support when major changes require directive updates
- Family education and communication support as your preferences evolve
- Crisis support if medical emergencies arise before you can update your directive
When Attorneys Become Necessary
Complex Blended Family Situations With Potential Legal Conflicts Over Medical Decisions
Some family situations involve legal complexities that require an attorney’s expertise rather than a doula’s support. When family members might legally challenge your medical decisions, attorney-prepared documents provide stronger legal protection.
Attorney consultation becomes necessary for:
- Estranged family members who might contest your healthcare proxy designations
- Blended families where the current spouse and adult children from previous marriages disagree
- Same-sex couples in states with unclear legal recognition of relationships
- Adults who want to exclude certain family members from medical decision-making
Significant Assets Requiring Coordination Between Advance Directives and Estate Planning
High-net-worth adults often need coordination between advance directives, estate planning, business succession, and trust management, which requires specialized attorney expertise.
Complex financial situations requiring attorney involvement:
- Business ownership that needs management during extended medical incapacity
- Trust funds or estate planning that intersects with healthcare decision-making authority
- Significant assets that could be depleted by prolonged medical care
- International assets or residences that complicate legal jurisdiction issues
Previous Family Legal Disputes Over Medical or Financial Decisions
Adults with histories of family legal conflicts need attorney-prepared advance directives that can withstand potential court challenges from disagreeing family members.
What Your Professional Will Handle For You
Gathering All Required State-Specific Forms and Documents
Your professional handles all the paperwork, research, and document gathering. You never need to worry about finding the right forms, understanding legal requirements, or ensuring you have the most current versions. This eliminates the risk of using outdated or incorrect forms that could invalidate your directive.
Please note that most attorneys are not up-to-date on advance directives for dementia, mental illness, VSED, et, and this is where end-of-life doulas who are appropriately trained shine!
Explaining Complex Legal and Medical Implications in Understandable Language Throughout the Process
Professional guidance translates complex medical and legal concepts into understandable language, helping you make informed decisions about your preferences without requiring medical or legal training.
The choice between professional support and attempting to create an advance directive alone isn’t really a choice at all—it’s an investment in your future security and your family’s peace of mind. Whether you choose an end-of-life doula for standard situations or an attorney for complex legal circumstances, professional guidance ensures your advance directive truly protects your wishes when you need them most.
Taking Action: Working with Professionals
The time for procrastination is over. Every day you wait to create or update your advance directive is another day you’re leaving your medical future—and your family’s peace of mind—to chance. Taking action means partnering with the right professional who can guide you through this essential adult responsibility with expertise, compassion, and attention to legal detail.
Choosing the Right Professional Support
Honestly Assessing Your Family and Financial Situation’s Complexity
Before you can choose the right professional, you need to take an honest look at your life circumstances. This isn’t about judgment—it’s about matching the right level of professional expertise to your specific situation and needs.
Most adults benefit from end-of-life doula support if they have:
Straightforward Young Adult Situations (20s-30s):
- Clear family relationships without major ongoing conflicts or estrangements
- Standard employment with typical health insurance coverage
- Single or married status without complex previous relationships
- Basic financial situations without significant business ownership or complex assets
Typical Mid-Life Adult Circumstances (40s-50s):
- Stable marriages or partnerships with good communication about medical preferences
- Standard parent-child relationships where adult children generally agree with each other
- Moderate income levels without complex investment portfolios or business interests
- Health situations involving common conditions that don’t require specialized legal planning
Standard Older Adult Scenarios (60s+):
- Retirement planning that includes Medicare and standard Social Security benefits
- Adult children who communicate well and respect their parents’ autonomy
- Straightforward estate planning without complex trusts or business succession issues
- Health conditions that are well-understood and don’t involve rare or experimental treatments
You likely need an attorney consultation instead if your situation involves:
- Blended family conflicts where the current spouse and adult children from previous marriages disagree about medical decisions
- Significant business ownership requiring management during potential medical incapacity
- Previous legal disputes within your family over financial or medical matters
- Multiple state residences with conflicting advance directive laws
Finding Qualified End-of-Life Doulas in Your Geographic Area
Professional certification ensures your doula has proper training in advance care planning, medical terminology, and family communication support. Don’t settle for well-meaning volunteers or uncertified individuals who lack specialized expertise.
Reliable sources for finding certified professionals:
National Certification Organizations:
- The National End-of-Life Doula Alliance (NEDA) provides geographic search capabilities
- International End-of-Life Doula Association (INELDA) maintains directories of certified professionals
- Hospice organizations often maintain referral lists of qualified end-of-life doulas
- Hospital social work departments frequently know certified professionals in your area
Local Professional Networks:
- Senior centers often host advance directive workshops with certified doula support
- Religious organizations may have partnerships with certified end-of-life doulas
- Healthcare providers sometimes maintain referral lists of qualified professionals
- Legal aid organizations occasionally partner with certified doulas for community education
Questions to Verify Professional Qualifications:
- What specific training and certification do you have for advance directive completion?
- How many advance directives have you helped adults complete in the past year?
- Are you familiar with our state’s specific legal requirements and recent changes?
- Do you provide ongoing support for updates and family communication?
Recognizing Situations That Require Attorney Consultation Instead of Doula Support
Honest self-assessment helps you choose appropriate professional support before investing time and money in the wrong type of guidance. Some situations genuinely require legal expertise rather than doula support.
Clear indicators you need an attorney consultation:
Legal Complexity Markers:
- Previous family lawsuits over medical or financial decisions
- Concerns that family members might legally challenge your healthcare proxy designations
- Complex business partnerships that could be affected by extended medical incapacity
- Significant assets requiring coordination between advance directives and estate planning
Family Relationship Complications:
- Estranged family members who might interfere with your medical decision-making
- Same-sex relationships in states with unclear legal recognition
- International family members or assets complicating legal jurisdiction
- Previous domestic violence or restraining orders affecting family access to medical decisions
Essential Questions to Ask Potential Professionals About Their Training, Experience, and Approach
Professional competence varies significantly, even among certified practitioners. Asking specific questions can help you find someone with the technical expertise and communication style that works for your situation.
Critical Questions About Training and Experience:
- What specific certification do you hold in end-of-life doula work or advance care planning?
- How many years have you been helping adults complete advance directives?
- Are you familiar with our state’s witness and notarization requirements?
- Do you stay current with changes in healthcare law and medical treatment options?
Questions About Approach and Communication Style:
- How do you help people work through difficult emotions about mortality and medical decisions?
- What’s your experience with family conflicts over medical preferences?
- How do you handle situations where family members disagree with someone’s choices?
- What ongoing support do you provide after advance directives are completed?
Practical Questions About Process and Costs:
- What exactly is included in your advance directive completion services?
- How long does the typical process take from start to finish?
- What are your fees, and what payment options do you accept?
- Do you provide support for regular updates and reviews?
The Professional Process: What to Expect
Initial Consultation to Assess Your Needs and Determine Appropriate Level of Professional Support
Your first meeting establishes whether you’ve chosen the right type of professional and creates a foundation for the advance directive completion process. Quality professionals spend significant time understanding your unique situation before jumping into document preparation.
What happens during initial consultations:
Comprehensive Situation Assessment:
- Discussion of your family relationships and potential sources of conflict over medical decisions
- Review of your current health status and any existing medical conditions
- Evaluation of your financial situation and insurance coverage
- Assessment of any previous experiences with serious illness or medical decision-making
Values and Preferences Exploration:
- What does quality of life mean to you personally at your current life stage?
- How do your religious, cultural, or philosophical beliefs influence your medical preferences?
- What are your biggest fears or concerns about potential medical incapacity?
- How do you want your family involved in medical decision-making processes?
Legal and Logistical Planning:
- Review of your state’s specific requirements for advance directive validity
- Discussion of witness and notarization requirements you’ll need to arrange independently
- Timeline establishment for completing your comprehensive advance directive
- Coordination with any existing legal documents, like wills or a power of attorney
Guided Values Clarification Discussions to Identify Your Medical and End-of-Life Preferences
This is where professional expertise becomes invaluable. Doulas help you think through complex medical scenarios you might never have considered, ensuring your advance directive addresses real-world situations rather than just obvious end-of-life decisions.
Typical values clarification topics:
Quality vs. Quantity of Life Decisions:
- What level of cognitive function would you require to consider life meaningful?
- How important is physical independence versus emotional connection with loved ones?
- What role does pain management play in your definition of acceptable quality of life?
- How do your responsibilities to family members influence your treatment preferences?
Specific Medical Intervention Preferences:
- Artificial nutrition and hydration during various stages of illness or injury
- Mechanical ventilation for both temporary and potentially permanent situations
- Dialysis and other organ support systems for chronic versus acute conditions
- Blood transfusions and aggressive infection treatments during end-of-life care
Communication and Family Involvement Preferences:
- How much medical information do you want shared with different family members?
- What role should religious or spiritual advisors play in your medical care?
- How do you want disagreements between family members handled?
- What level of privacy do you want regarding your medical condition and treatments?
Professional Document Preparation Ensuring Full Legal Compliance With Your State’s Requirements
Your professional handles all the technical aspects of document preparation while you focus on clarifying your medical preferences and values.
What professionals handle for you:
- Gathering current state-specific forms and ensuring you have the most recent legal versions
- Translating your preferences into a legally appropriate language that meets state requirements
- Ensuring all required sections are completed properly and all signatures are obtained
- Explaining witness and notarization requirements
Your responsibilities during document preparation:
- Thoughtful completion of all personal information and medical preference sections
- Arranging for appropriate witnesses who meet your state’s legal requirements
- Scheduling notarization appointments with qualified notaries who are not related to you
- Reviewing completed documents carefully to ensure they accurately reflect your wishes
Family Communication Support and Education About Your Completed Advance Directive
Creating your advance directive is only the beginning. Professional support includes helping you communicate your decisions to family members and ensuring everyone understands their roles during potential medical emergencies.
Family education and communication support:
- Facilitating family meetings to discuss your completed advance directive and medical preferences
- Providing educational materials to help family members understand medical terminology and treatment options
- Addressing family concerns or disagreements about your documented preferences
- Ensuring your designated healthcare proxy understands their responsibilities and feels prepared
Ongoing Professional Maintenance and Updates
Establishing Regular Review Schedules (Every 3-6 months) With Your Chosen Professional
Your advance directive should evolve as your life changes. Professional support includes ongoing maintenance to ensure your documented preferences stay current with your actual values and circumstances.
Regular review appointments typically address:
- Significant life changes since your last review that might affect your medical preferences
- Updates to your health status or new medical diagnoses
- Changes in family relationships or healthcare proxy availability
- Moves to different states or changes in insurance coverage
Identifying Life Change Triggers That Require Immediate Directive Updates
Certain life events require immediate professional attention rather than waiting for your next scheduled review. Understanding these triggers helps you maintain current, legally valid documentation.
Major life changes requiring immediate updates:
- Marriage, divorce, or the death of a spouse affects healthcare proxy designations
- The birth or adoption of children changes your medical decision-making priorities
- Diagnosis of serious or chronic medical conditions affects treatment preferences
- Geographic relocation to states with different advance directive legal requirements
Ongoing Professional Support for Family Communication About Medical Preference Changes
Family relationships and communication needs evolve over time. Ongoing professional support helps maintain healthy family communication about your medical preferences as circumstances change.
Building a Long-Term Professional Relationship That Evolves With Your Changing Adult Life Circumstances
Quality end-of-life doula relationships span decades rather than single transactions. This continuity ensures someone familiar with your values and family dynamics provides consistent support throughout your adult life.
Call to Action: Find Your Professional Today
The peace of mind that comes from knowing your advance directive was created with proper professional guidance cannot be overstated. Every adult deserves expert support in making these crucial decisions—whether you’re 18 or 80, healthy or managing chronic conditions.
Your Immediate Next Steps:
- Locate qualified end-of-life doulas in your area through professional certification organizations like INELDA or NEDA
- Schedule initial consultations to find the right professional fit for your situation and communication style
- Don’t wait for a health crisis—professional guidance is most effective when you’re healthy and able to think clearly about your preferences
- Remember that professional support is an investment in your future peace of mind and your family’s emotional well-being during difficult times
The most important decision isn’t whether you can afford professional help—it’s whether you can afford to leave your medical future to chance. Find an end-of-life doula today to review any existing directives or create comprehensive new ones that truly protect your wishes and your loved ones.
Your future self will thank you for taking control today. Every adult conversation you avoid, every month you postpone this essential planning, is another opportunity lost to ensure your medical care reflects your values when you can’t speak for yourself. The time for action is now—find your professional support and take control of your medical future while you still can.
Resources
Approximately One In Three US Adults Completes Any Type Of Advance Directive For End-Of-Life Care
Most Americans lack advance directives — but they also report concerns about end-of-life care
Many Avoid End-Of-Life Care Planning, Study Finds
Less Than Half of U.S. Adults Have Wills or Advance Healthcare Directives
The National Academy of Elder Law Attorneys (NAELA) is dedicated to improving the quality of legal services provided to older adults and people with disabilities
Articles on Advance Directives
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
Caregiver Support Book Series
VSED Support: What Friends and Family Need to Know
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.
End-of-Life-Doula Articles