Tag: Hospice Care
Articles about hospice care including how to manage comfort at end of life.
Articles about hospice care including how to manage comfort at end of life.

As a caregiver or family member, witnessing the final hour of a loved one's life can be a challenging and emotional experience. It's essential to be prepared and understand what to expect. While each person's journey is unique, some common physical changes may occur in the last hour of life. Here's a guide to help you navigate this sensitive time:
Dealing with a loved one's heart failure can be overwhelming, but with the right knowledge and support, you can provide the best care possible. This guide aims to help families understand what heart failure is, what changes to expect in their loved one's condition, and how to provide compassionate care throughout the journey, from onset to end-of-life.

It is common for family members and caregivers who are not trained in end-of-life topics to be concerned about their loved one's oxygen concentration (SpO2 and sometimes also abbreviated SPaO2) reading from a pulse oximeter. Suppose their loved one refuses external oxygen or takes off the external oxygen. In that case, this often causes distress to the family and caregivers because they are focused on the numbers vs. the patients themselves. Hospice is about patient-centered care, and I would like to present four case studies to demonstrate how hospice manages this situation with compassion.

When a dementia patient inquiries about a family member who has passed away but still believes them to be alive, it's essential to respond with empathy and understanding. Here are some tips on how to handle such situations with compassion and sensitivity:
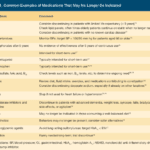
I know how important it is to provide comfort and support during this challenging journey. One aspect of hospice care that often raises concerns is deprescribing medications. In this article, we'll explore what deprescribing is and why it can benefit patients nearing the end of life.
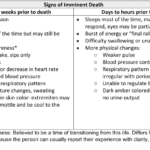
Recognizing end-of-life signs can be challenging. This guide outlines key symptoms indicating a terminally ill patient may have less than two weeks, offering crucial insights for caregivers and families.

As an experienced hospice nurse with years of experience, I understand that coping with a loved one's diagnosis of Chronic Obstructive Pulmonary Disease (COPD) can be overwhelming and challenging. In this article, we'll explore what to expect over the course of the disease, the changes you might notice in your loved one, and how to provide the best care and support from the onset until the end.
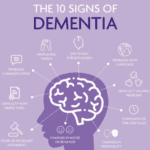
Caring for a loved one with dementia can be a challenging journey, filled with complex emotions and difficult decisions. As families and caregivers, it's crucial to understand the nature of dementia and the various tools available to help assess and manage the condition. This article aims to provide a comprehensive guide to the seven most common memory tests used to evaluate if a person has dementia. These include the Alzheimer's Disease Assessment Scale-Cognitive (ADAS-Cog), Mini-Mental State Examination (MMSE), General Practitioner Assessment of Cognition (GPCOG), Montreal Cognitive Assessment (MoCA), Self-Administered Gerocognitive Exam (SAGE), Neuropsychological evaluation, and Short Test of Mental Status. Each of these tests offers unique insights into the cognitive abilities of an individual and can be instrumental in the early detection and management of dementia. By understanding these tests, you can better navigate the path of dementia care and ensure your loved one receives the best possible support.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.
As a hospice nurse, I understand the importance of documenting observational signs of discomfort in terminally ill patients. This guide covers recognizing physical and behavioral cues indicating discomfort, even if patients don't express it. It also highlights the benefits of journaling for families and nurses, with tips for effective documentation to enhance patient comfort and care.
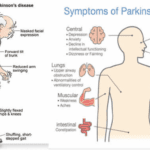
If you have a loved one diagnosed with Parkinson's disease, you may have many questions and concerns about what to expect and how to provide the best care possible. As an experienced hospice nurse with extensive experience in managing terminal illnesses, I am here to guide you through the journey of Parkinson's disease and offer compassionate support. In this article, we will explore Parkinson's disease, the changes your loved one may experience over time, and practical tips to care for them from the onset to the end-of-life phase.

Radiation therapy is a common treatment for head and neck cancers, but it can lead to the loss of taste, also known as dysgeusia, in some patients. This can be a distressing side effect, but there are steps that patients and caregivers can take to help restore the patient's sense of taste as quickly as possible, with minimal risk. While there is no guaranteed way to restore taste, these tips and strategies may help patients regain some of their enjoyment of food and drink.

Witnessing a loved one nearing the end of life can be challenging and emotional for a caregiver. One symptom you may encounter during this time is the death rattle. Understanding what the death rattle is, how to recognize it, and how to manage its symptoms can help you provide comfort and support to your loved one in their final days. This guide will explore the death rattle, its significance, and practical tips for managing it.
Hospice volunteer coordinators ensure hospice patients receive the compassionate care and support they need during their end-of-life journey. In this article, we will explore the responsibilities of a hospice volunteer coordinator, address common misconceptions about hospice volunteers, and share insights from Hope Eberly, Volunteer Coordinator for Grane Hospice.

As a caregiver or family member, it can be challenging to witness the changes that occur as a loved one approaches the end of their life. One such change that may occur is mottled skin, also known as livedo reticularis. Understanding what mottled skin is and its significance in the dying process can help you provide the best care and support to your loved one during this time.
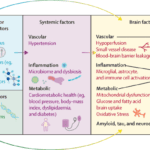
Dementia is a progressive disease that affects memory, thinking, and behavior. While there is no cure for dementia, there are ways to minimize its progression and improve the quality of life for those living with the disease. Here are some activities to do, activities to avoid, dietary changes to make, and activities to perform to minimize the progression of dementia.

Pharmaceutical advertisements often highlight the benefits of a particular drug, including its ability to reduce the risk of various health conditions. However, the actual risk reduction these drugs provide may differ from what is portrayed in the advertisements. It is the opinion of the author that if cardiologists and other providers told their patients the absolute risk reduction of statins is 0.8% for all-cause mortality, 1.3% for myocardial infarction and 0.4% for stroke and the side effects of going on a statin include dementia, worsening dementia, confusion, muscle problems, such as aches, pains, weakness, muscle breakdown, falls, nausea, constipation, diarrhea, and increase the risk of type 2 diabetes, would you or anyone else ever agree to take a statin?
Laryngeal cancer is a complex diagnosis for both patients and families. This article aims to provide guidance and support for families new to caring for a loved one with laryngeal cancer. We will discuss what to expect throughout the disease, the changes you may notice in your loved one, and how to provide optimal care from the initial diagnosis to the end.
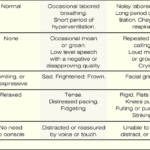
If you have a loved one with dementia, it can be difficult to know if they are in pain or discomfort. The Pain Assessment in Advanced Dementia Scale (PAINAD) is a tool that can help you determine if your loved one is uncomfortable. The Pain Assessment in Advanced Dementia Scale (PAINAD) is different from other pain assessment tools for people with dementia in several ways:
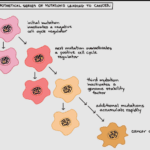
When cancer spreads from its original site to other parts of the body, it's known as metastatic cancer. This article aims to provide information about cancer metastasis, the common areas of metastasis based on the origin of the cancer, observable signs and symptoms, and how families can support their loved ones as the cancer progresses.

Receiving a terminal cancer diagnosis for a loved one can be overwhelming and emotional. I understand your challenges in providing care and support during this difficult journey. This educational article aims to guide families on what to expect throughout the disease, what changes they might see in their loved one, and how to best care for them from onset until the end.

Proper documentation is crucial for hospice nurses to ensure Medicare compliance and maintain the patient's eligibility for services. Auditors, who may not have a healthcare background, review these documents to determine if the patient's condition is terminal. To avoid having the patient removed from service due to improper documentation, hospice nurses should be mindful of the words and phrases they use in their nursing narratives and progress notes. This article will guide what to avoid and why it is essential to paint a picture of a terminally ill patient.

Heart failure is a complex medical condition that can impact the quality of life of patients, especially those in hospice care. As a hospice nurse, assessing the heart failure stage is crucial to providing appropriate care accurately. This article will explore the New York Heart Failure Classification System, its stages, and how to assess patients for their stages. Additionally, we will emphasize the importance of documentation in compliance with Medicare guidelines for terminally ill patients with heart failure.

Deciding on end-of-life care for a loved one is challenging and emotional. One major decision to make is whether to opt for home hospice or hospice care at a facility. Both options have advantages and drawbacks, and understanding the pros and cons can help families make an informed choice. Here, we'll explore the pros and cons of each option and provide key questions that families should ask themselves to aid in their decision-making process.