Empowering Caregivers: Effective Communication with Healthcare Providers
Published on June 23, 2024
Updated on July 12, 2024
Published on June 23, 2024
Updated on July 12, 2024

Table of Contents
Being a family caregiver is a significant responsibility. You’re not just there to provide comfort and companionship; you’re also an advocate for your loved one’s well-being. It’s natural to feel concerned about their care, especially when you notice something amiss. But remember, your voice matters, and expressing your worries is essential. Let’s explore two practical communication tools—the CUS Tool and the Caring Feedback Model—that can empower you to speak up confidently.
As a family caregiver, you’re deeply invested in your loved one’s well-being. Sometimes, you might notice things that worry you about their care. Speaking up can feel intimidating, especially when communicating with doctors or nurses. But your voice matters, and there are effective ways to express your concerns. Let’s explore the CUS Tool—a powerful communication method to help you advocate for your loved one.
The CUS Tool is a straightforward approach that empowers you to escalate your concerns respectfully and clearly. The acronym stands for:
The CUS Tool is effective because it allows you to be clear and direct without being confrontational. Following this structured approach, you advocate for your loved one while maintaining a respectful relationship with the care team. Remember, healthcare professionals value your insights, and your voice matters. Use the CUS Tool confidently—it’s powerful in your caregiving toolkit.
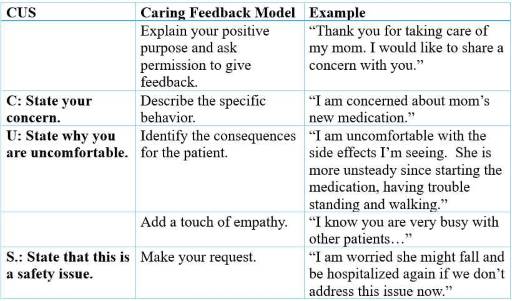
As a family caregiver, your role extends beyond providing physical care. You’re also an advocate for your loved one’s well-being. When communicating with healthcare professionals, you must balance your concerns with empathy and respect. The Caring Feedback Model offers a structured way to express your worries while maintaining a positive relationship with the care team.
The Caring Feedback Model emphasizes compassion and collaboration. Let’s break it down:
This approach balances your concerns with appreciation and empathy. It fosters open communication and encourages collaboration. Remember, healthcare professionals value your insights. Using the Caring Feedback Model, you advocate effectively for your loved one while maintaining a respectful relationship with the care team.
As a family caregiver, you’re navigating a complex landscape of healthcare decisions for your loved one. Combining the CUS Tool and the Caring Feedback Model can empower you to advocate effectively while maintaining a respectful relationship with the care team. Let’s dive into how these two approaches work together:
Appreciate: Start any conversation with gratitude. Acknowledge the hard work of the healthcare providers. For instance:
Concern: State your worry clearly. Be specific about what you’ve observed. For example:
Uncomfortable: Express any discomfort you feel. Describe the side effects or issues you’ve noticed:
Safety: If the concern persists, emphasize safety. Highlight potential risks:
Suggest: Offer constructive solutions. Collaborate with the care team:
Consequences: Help the care team understand the potential outcomes. Explain the impact of unaddressed issues:
Empathize: Show understanding. Recognize that healthcare providers have many patients:
Remember, your goal is to work collaboratively with healthcare professionals to ensure the best care possible for your loved one. Your voice matters; combining these communication tools allows you to advocate effectively while maintaining empathy and respect.
As a family caregiver, your role is multifaceted—you provide comfort, companionship, and crucial advocacy for your loved one’s well-being. The CUS Tool (Concern, Uncomfortable, Safety) is a powerful way to express your concerns effectively. Let’s explore how you can prepare to use the CUS Tool confidently:
Your instincts matter. Here are situations where using the CUS Tool is essential:
Remember, your voice matters. Trust your instincts—it’s worth speaking up when something feels wrong.
Before using the CUS Tool, gather the essential details:
Use this sample table to organize your observations:
| Date | Time | Observation | Questions/Concerns |
|---|---|---|---|
Advocacy can be nerve-wracking, but you’re an essential part of the care team. Boost your confidence:
By preparing thoroughly, you’ll confidently use the CUS Tool. Healthcare providers value your insights, and your advocacy ensures the best care for your loved one.
As a family caregiver, your role is vital in ensuring your loved one receives the best care possible. The CUS Tool (Concern, Uncomfortable, Safety) is a valuable communication method that allows you to express your concerns effectively. Let’s dive into how you can implement the CUS Tool in healthcare conversations:
When discussing your concerns with healthcare providers, follow these guidelines:
If your initial concern isn’t adequately addressed, express your discomfort:
When steps 1 and 2 don’t lead to action, stress the safety aspect:
Always follow up with a proposed course of action:
Here’s a table to help you remember the CUS steps:
| Step | Key Word | Purpose | Example Phrase |
|---|---|---|---|
| 1 | Concern | Express worry | “I’m concerned about…” |
| 2 | Uncomfortable | Escalate the issue | “I’m uncomfortable with…” |
| 3 | Safety | Emphasize potential harm | “This is a safety issue because…” |
| 4 | Suggest | Propose a solution | “Could we please…” |
Remember, your goal is collaborative communication with healthcare providers. Stay respectful, stay focused on your loved one’s well-being, and don’t hesitate to use the CUS Tool. You’re not being difficult—you’re an essential advocate for your loved one’s health and safety. Healthcare professionals are trained to respond to these keywords, so use them confidently when necessary.
Pro Tip: To build confidence, practice using the CUS Tool with a friend or family beforehand. Your advocacy matters!
As a family caregiver, you’re navigating a complex healthcare landscape, and advocating for your loved one can be rewarding and challenging. Let’s explore some common challenges and practical strategies to overcome them:
Healthcare providers may sometimes appear dismissive of your concerns. Here’s how to handle such situations:
Medical terminology can be confusing. Here’s how to handle it:
If your concerns aren’t being addressed, persistence is crucial:
Here’s a table summarizing these strategies:
| Challenge | Strategy | Example Phrase |
|---|---|---|
| Dismissive Responses | Stay calm, reiterate concern, seek support | “I understand you’re busy, but I’m concerned about…” |
| Medical Jargon | Ask for clarification, take notes, use resources | “Can you explain that in a way I can understand?” |
| Unaddressed Concerns | Document everything, follow up, escalate if needed | “I mentioned my concern last week. Can we please review it again?” |
Pro Tip: Practice these strategies with a friend or family member to build confidence. Remember, your persistence and advocacy significantly impact your loved one’s care. Healthcare providers value your input; you’re essential to the care team!
As a caregiver, you play a vital role in advocating for your loved one’s well-being. The CUS Tool (Concern, Uncomfortable, Safety) empowers you to express your worries effectively. Let’s explore real-life scenarios where CUS can make a difference:
Scenario: Your mother has been prescribed a new medication, but you notice she’s experiencing unusual side effects.
Using CUS:
Remember: Your observations are valuable. Don’t hesitate to speak up about medication concerns.
Scenario: Your spouse is recovering from surgery and appears to be in significant pain despite the current pain management plan.
Using CUS:
Pro Tip: Use a pain scale (0-10) to objectively describe your loved one’s pain level to healthcare providers. If you or your loved one are uncomfortable using the zero to ten scale, use “none, mild, moderate, and severe.”
Scenario: The hospital is preparing to discharge your father, but you feel he’s not ready to manage at home yet.
Using CUS:
Important: Don’t be afraid to ask for a detailed discharge plan and instructions.
Here’s a table summarizing these scenarios:
| Scenario | Concern | Uncomfortable | Safety | Suggestion |
|---|---|---|---|---|
| Medication | New side effects | Continuing without discussion | Risk of falls or errors | Review medication |
| Pain Management | Increased pain | Ineffective management | Slow recovery, complications | Reassess pain plan |
| Discharge Readiness | Weakness, unsteadiness | Going home too soon | Fall risk, inability to self-care | Review discharge plan |
Remember: These scenarios are just examples. Every situation is unique, and you should trust your instincts regarding your loved one’s care. The healthcare team wants to provide the best care possible, and your input is crucial in achieving that goal. By using the CUS tool in these situations, you’re not being difficult – you’re an essential advocate for your loved one’s health and safety. Practice these scenarios with a friend or family member to build your confidence in using CUS when it matters.
As a caregiver, your role is critical in ensuring the well-being of your loved one. Effective communication with healthcare providers can significantly impact the quality of care your loved one receives. Let’s explore practical tips for building rapport, documenting observations, preparing for appointments, and using clear communication techniques:
Building a good relationship with your loved one’s medical team can make a big difference in their care. Here are some ways to do this:
Pro Tip: Start conversations with a positive comment or thank you. For example, “Thank you for speaking with me about my mother’s care.”
Keeping accurate records can help you communicate more effectively with healthcare providers. Here’s how to do it:
Here’s a simple table you can use to organize your observations:
| Date | Time | Observation | Questions/Concerns |
|---|---|---|---|
Remember: Your observations are valuable. Don’t hesitate to share them with the healthcare team.
Being prepared can help you make the most of your time with healthcare providers:
Tip: Ask the most important questions first in case time runs short.
When speaking with healthcare providers:
Example: “I’m concerned about the new medication because I’ve noticed my father seems more confused since starting it.”
Remember: You are essential to your loved one’s care team. Your input and observations are valuable; you can ask questions and express concerns. You can build a strong partnership with your loved one’s healthcare providers using these communication strategies. This collaboration can lead to better care and outcomes for your loved one. Don’t be afraid to speak up—your role as an advocate is crucial in ensuring the best possible care.
Patient advocates are professionals who work to protect patients’ rights and help them navigate the complex healthcare system. They can be a powerful ally when facing challenges in your loved one’s care.
You might want to involve a patient advocate when:
Remember: Seeking help from a patient advocate doesn’t mean you’ve failed. It means you’re doing everything you can to ensure the best care for your loved one.
There are different types of patient advocates available:
Here are some steps to find a patient advocate:
Once you’ve found an advocate, here’s how to work effectively with them:
Here’s a table to help you prepare for working with a patient advocate:
| Information to Prepare | Details to Include |
|---|---|
| Medical History | Diagnoses, treatments, medications |
| Current Concerns | Specific issues you’re facing |
| Previous Actions Taken | Use of CUS tool, conversations with providers |
| Goals | What do you hope to achieve with advocacy |
| Questions | List any questions you have for the advocate |
Pro Tip: Keep a folder with all this information organized and ready to share with your advocate.
Involving a patient advocate can:
Remember: You’re not alone in this journey. Patient advocates support you and your loved one, ensuring the best care and outcomes. By involving a patient advocate when necessary, you’re taking an essential step in being the best possible caregiver for your loved one. It’s a sign of strength, not weakness, to seek help when needed. Your loved one’s health and well-being matter most, and a patient advocate can be a valuable ally in achieving the best possible care.
When all family members are on the same page and know how to use the CUS tool, their collective voice strengthens. This can lead to better communication with healthcare providers and improved care for your loved one.
Here’s how you can teach the CUS tool to other family members:
Example Handout:
| Step | What to Say | Example |
|---|---|---|
| Concern | “I’m concerned about…” | “I’m concerned about Dad’s new medication.” |
| Uncomfortable | “I’m uncomfortable with…” | “I’m uncomfortable with the side effects he’s experiencing.” |
| Safety | “This is a safety issue because…” | “This is a safety issue because he might fall.” |
When all family members are empowered to use CUS, it creates a more vital, unified approach to advocating for your loved one. Here’s how to ensure everyone is on the same page:
Scenario: Your family is concerned about your grandmother’s pain management.Family Meeting Discussion:
To ensure that all family members consistently use the CUS tool:
Pro Tip: Create a family group chat or email thread to share updates and support each other using the CUS tool. Empowering other family members to use the CUS tool creates a robust and united front that can effectively advocate for your loved one’s care. Remember, your collective voice is powerful, and using CUS can help ensure that healthcare providers hear and address your concerns.
When all family members and caregivers know how to use the CUS tool, they strengthen their collective ability to communicate concerns effectively, leading to better care and safety for their loved ones.
Example Handout:
| Step | What to Say | Example |
|---|---|---|
| Concern | “I’m concerned about…” | “I’m concerned about Dad’s new medication.” |
| Uncomfortable | “I’m uncomfortable with…” | “I’m uncomfortable with the side effects he’s experiencing.” |
| Safety | “This is a safety issue because…” | “This is a safety issue because he might fall.” |
Role-playing can help family members feel more comfortable using the CUS tool. Here are some scenarios to practice:
Scenario 1: Medication Concerns
Scenario 2: Addressing Pain Management
Scenario 3: Questioning Discharge Readiness
When all family members are empowered to use CUS, it creates a more vital, unified approach to advocating for your loved one. Here’s how to ensure everyone is on the same page:
To ensure that all family members consistently use the CUS tool:
Pro Tip: Create a family group chat or email thread to share updates and support each other using the CUS tool. By teaching the CUS tool to your support network, you create a robust and united front that can effectively advocate for your loved one’s care. Remember, your collective voice is powerful, and using CUS can help ensure that healthcare providers hear and address your concerns.
Effective communication is crucial in healthcare settings. As a caregiver, your observations and concerns are vital to ensuring your loved one receives the best care. Throughout this guide, we’ve discussed several tools and strategies to help you communicate effectively with healthcare providers:
You are essential to your loved one’s healthcare team as a caregiver. Your voice matters, and you have the power to make a significant difference. Here are some empowering words to keep in mind:
Remember: Your role as a caregiver is invaluable. By using effective communication tools and strategies, you can help ensure your loved one receives the best possible care. Your advocacy can prevent errors, improve outcomes, and provide comfort and safety for your loved one.
Advocating for your loved one in healthcare settings can be challenging, but it is also gratifying. By using the CUS tool, building rapport with the medical team, documenting concerns, involving patient advocates, and empowering other family members, you can create a strong support system for your loved one. Your dedication and persistence are crucial to ensuring their safety and well-being.
Pro Tip: Keep a positive mindset and remind yourself of your impact. Your efforts are helping your loved one and contributing to a culture of safety and effective communication in healthcare.
Empowering Affirmation: “I am my loved one’s voice. My concerns are valid, and I have the power to make a difference in their care.”By embracing these tools and strategies, you are taking an active role in your loved one’s healthcare journey. Your advocacy is powerful for ensuring they receive the best possible care.
Use the CUS tool to speak up with confidence.
Safeguarding patients: The courageous communication solution
DESC Tool for de-escalation focused on patient safety and positive outcomes
Empowering Your Caregiving: Learning to Advocate for Your Loved One (PDF)
Pathways to Effective Communication for Health Care Providers and Caregivers
Communication Tips for Caregivers
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?