Category: Tips For Nurses
Articles for nurses caring for terminally ill patients including how to manage challenging situations.
Articles for nurses caring for terminally ill patients including how to manage challenging situations.

It is common for family members and caregivers who are not trained in end-of-life topics to be concerned about their loved one's oxygen concentration (SpO2 and sometimes also abbreviated SPaO2) reading from a pulse oximeter. Suppose their loved one refuses external oxygen or takes off the external oxygen. In that case, this often causes distress to the family and caregivers because they are focused on the numbers vs. the patients themselves. Hospice is about patient-centered care, and I would like to present four case studies to demonstrate how hospice manages this situation with compassion.

When a dementia patient inquiries about a family member who has passed away but still believes them to be alive, it's essential to respond with empathy and understanding. Here are some tips on how to handle such situations with compassion and sensitivity:
I know how important it is to provide comfort and support during this challenging journey. One aspect of hospice care that often raises concerns is deprescribing medications. In this article, we'll explore what deprescribing is and why it can benefit patients nearing the end of life.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.
As a hospice nurse, I understand the importance of documenting observational signs of discomfort in terminally ill patients. This guide covers recognizing physical and behavioral cues indicating discomfort, even if patients don't express it. It also highlights the benefits of journaling for families and nurses, with tips for effective documentation to enhance patient comfort and care.
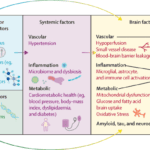
Dementia is a progressive disease that affects memory, thinking, and behavior. While there is no cure for dementia, there are ways to minimize its progression and improve the quality of life for those living with the disease. Here are some activities to do, activities to avoid, dietary changes to make, and activities to perform to minimize the progression of dementia.

Pharmaceutical advertisements often highlight the benefits of a particular drug, including its ability to reduce the risk of various health conditions. However, the actual risk reduction these drugs provide may differ from what is portrayed in the advertisements. It is the opinion of the author that if cardiologists and other providers told their patients the absolute risk reduction of statins is 0.8% for all-cause mortality, 1.3% for myocardial infarction and 0.4% for stroke and the side effects of going on a statin include dementia, worsening dementia, confusion, muscle problems, such as aches, pains, weakness, muscle breakdown, falls, nausea, constipation, diarrhea, and increase the risk of type 2 diabetes, would you or anyone else ever agree to take a statin?

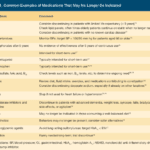
Proper documentation is crucial for hospice nurses to ensure Medicare compliance and maintain the patient's eligibility for services. Auditors, who may not have a healthcare background, review these documents to determine if the patient's condition is terminal. To avoid having the patient removed from service due to improper documentation, hospice nurses should be mindful of the words and phrases they use in their nursing narratives and progress notes. This article will guide what to avoid and why it is essential to paint a picture of a terminally ill patient.

Heart failure is a complex medical condition that can impact the quality of life of patients, especially those in hospice care. As a hospice nurse, assessing the heart failure stage is crucial to providing appropriate care accurately. This article will explore the New York Heart Failure Classification System, its stages, and how to assess patients for their stages. Additionally, we will emphasize the importance of documentation in compliance with Medicare guidelines for terminally ill patients with heart failure.
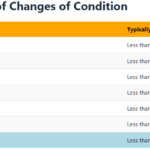
Explore the journey of functional decline in the natural dying process. This article provides insight for caregivers and families, emphasizing the importance of documenting changes to enhance care and decision-making in life’s final chapter.

Medication reconciliation plays a pivotal role in hospice care, ensuring terminally ill patients receive safe medication regimens. This process involves maintaining an accurate medication list to prevent adverse drug events. It's essential at various stages, including admission, recertification, and changes in condition. Healthcare professionals should be familiar with tools like the Beers Criteria and STOPP/START criteria to identify potentially inappropriate medications and prescribing omissions in older adults.

Hospice nurses assess the status of the patient's journey towards the end of life every nursing visit. Situations where a reversible condition can drastically impact the patient and the hospice assessment can occur. If it is not caught, it is potentially mistreated, leading to increased discomfort and a faster death, often involving increased suffering. One of the common clues that someone is getting closer to dying is increased agitation and restlessness.
Are you aware of Serotonin Syndrome?
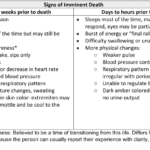
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.
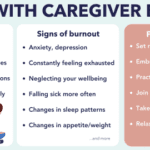
Caring for a loved one with dementia can be a rewarding experience, but it can also be physically, emotionally, and mentally exhausting. Family caregivers often neglect their own well-being while focusing on the needs of their loved ones, leading to burnout. Caregiver burnout is a state of physical, emotional, and mental exhaustion that can happen when caregivers don't get the help they need or try to do more than they are able to do. In this article, we will discuss how family caregivers of a loved one with dementia can avoid burnout and recover if they are already experiencing burnout.
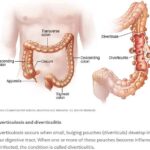
Caring for a loved one with a history of diverticulitis requires a combination of preventive measures, early detection of warning signs, and understanding the common signs and symptoms of this condition. Your role as a caregiver is crucial in providing support and assistance to ensure their well-being. In this comprehensive guide, we will explore essential aspects of caring for someone with diverticulitis, including prevention, early warning signs, and treatment options.

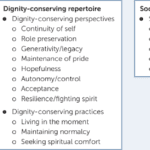
In the realm of hospice care, where empathy and compassion are paramount, a remarkable approach called Validation Therapy has emerged as a beacon of hope and comfort for individuals facing dementia and cognitive disorders in their final journey. As an experienced hospice registered nurse case manager, I've witnessed the transformative impact of Validation Therapy on patients, allowing them to find solace, regain their self-worth, and experience a sense of dignity during their end-of-life phase.

Caring for individuals with dementia can be both challenging and rewarding. One approach that has gained recognition for promoting meaningful relationships with dementia patients is Validation Therapy, developed by Naomi Feil. This article will explore how Validation Therapy works, why it does not involve telling a single lie, and why honesty is crucial when dealing with dementia patients.

Caring for a terminally ill loved one is a profound and challenging journey that requires compassion, understanding, and a willingness to alleviate any discomfort they may experience. In this guide, we will explore the concept of discomfort, its distinction from pain, and the importance of recognizing and addressing discomfort in addition to pain. You'll be better equipped to provide holistic care that enhances your loved one's quality of life during this sensitive time.
Throughout your loved one's illness, you might find yourself thinking that they don't require "pain medication" because they don't seem to be in pain. They might even respond with a direct "no" when asked about their pain. However, are you aware that most types of pain medication can alleviate discomfort? Did you also know that your loved one could be feeling uncomfortable without necessarily being in severe pain? Nonetheless, it's important to recognize that their discomfort requires the same treatment as if they were in pain.
This article provides valuable insights for hospice nurses on improving documentation to conquer Medicare audits and ensure claims are not denied due to insufficient evidence of terminal prognosis. The author shares real-life examples of visit narratives before and after implementing documentation best practices learned from an expert. The tips focus on capturing negative condition changes, disorientation levels, and functional decline to paint a clear picture of the patient's terminal state, ultimately leading to better patient care.
Educating nursing home staff on hospice care priorities like shifting focus from vital signs to comfort, managing symptoms like pain/breathlessness, providing psychosocial support, end-of-life planning, and bereavement care is crucial. Hospice emphasizes quality of life over curative treatments. Effective symptom management through medications and non-pharmacological approaches enhances patient comfort. Open communication, empathy, and respecting patient autonomy are essential. Hospice prepares families for the dying process and grief counseling.

The longer I work in hospice, the more I'm reminded about two critical pieces of wisdom: 1) Hospice is about living, and 2) we should all do our best to live a life of least regrets.
While this article is geared towards family members with a terminally ill loved one, as well as my fellow workers in the fields of palliative and hospice care, I believe the thoughts that I will share apply to everyone alive near and far.

Whether you are a new hospice nurse or an experienced one like me, I would hope that it is your desire to prove and support continued hospice eligibility for your patients and families. In my years as a hospice nurse, I've always felt the training on what words and phrases to use to support hospice eligibility was weak compared to the training received in other areas of nursing. Now, you have a means of getting the education you need in a very portable setup that you can take with you, use as you see fit, and bloom!

One of the hardest portions of the job of a hospice nurse is to identify when a patient has two weeks of life left to live; this can be especially difficult at facilities going through staffing shortages leading to inconsistent caregivers with little to verbally report on a patient’s change of condition. Since being aware of the velocity of declines is extremely important, let’s cover an area that we in hospice (nurses, families, and caregivers alike) can keep an eye on in terms of identifying terminal restlessness which is often a key indicator for one week or less of life.
I understand the challenges that patients and families face when receiving hospice services. One common issue that arises is the need for after-hour calls, which can add stress to an already demanding situation. However, with proactive care and effective communication, dayshift hospice RN case managers can play a crucial role in reducing after-hour calls and providing better support to patients and their families. Here’s how: