Category: Tips For Nurses
Articles for nurses caring for terminally ill patients including how to manage challenging situations.
Articles for nurses caring for terminally ill patients including how to manage challenging situations.

Explore the essential regulatory timeline requirements for hospice providers, covering everything from initial certifications to recertifications, nurse visits, and face-to-face encounters. This comprehensive guide helps ensure compliance and proper billing practices for hospice services.
Dementia is a challenging journey for both patients and caregivers. This comprehensive guide explores the stages of dementia progression and offers practical advice on care strategies, treatment options, and support resources. Learn how to navigate the changes and provide compassionate care throughout the journey.

This article delves into Utilization Behavior in dementia, offering practical advice for families and caregivers to create a safe environment and mitigate the challenges associated with this condition.
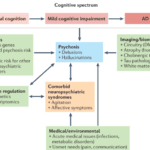
This guide provides hospice nurses, caregivers, and family members with essential information on dementia-induced psychosis, including its signs, symptoms, differentiation from other conditions, and effective management strategies.

This article provides practical tips and strategies for caregivers and family members to prevent dementia patients from removing their oxygen nasal cannula. Ensuring continuous oxygen use is essential for their health and well-being.

Learn about the diagnosis codes not allowed as primary diagnoses on hospice claims. This guide helps hospice agencies ensure accurate billing and optimal patient care.
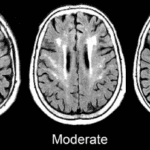
Caring for someone with Chronic Small Vessel Disease (CSVD) can be challenging, but with the proper knowledge and strategies, you can make a significant difference. This guide offers practical advice on creating a supportive environment, managing symptoms, and improving the quality of life for your loved one with CSVD.

This comprehensive guide explores blood work for common terminal diseases. Learn which lab tests are necessary for different conditions and how they assist in managing disease progression and treatment. Ideal for caregivers, nurses, and family members.

This guide helps hospice teams, caregivers, and families support loved ones with immunotherapy-induced tremors. Explore adaptive tools, tremor-reducing therapies, medication options, and practical care strategies to improve quality of life during hospice transitions.
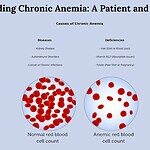
This guide explains chronic anemia in simple terms, covering symptoms, diagnosis, and treatments. Helps patients and families recognize signs and work with healthcare providers.
This article delves into the relationship between vertigo and dementia, offering insights for nurses, caregivers, and families to manage dizzy spells and provide compassionate care for those with cognitive challenges.

This article delves into the common medications that can lead to swelling in geriatric patients, with a focus on those receiving end-of-life care. It provides insights into prevention, management, and the importance of informed healthcare decisions.
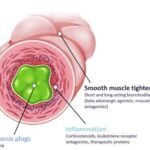
Understanding respiratory mucus plugs is crucial, especially for those navigating the challenges of caring for terminally ill patients. As an experienced hospice nurse, I recognize the significance of addressing respiratory issues with empathy and clarity. This article aims to provide valuable insights into respiratory mucus plugs, their causes, diagnosis, treatment, prevention, and practical techniques to enhance lung function.

Caring for a loved one with dementia can be challenging, especially when it comes to preventing falls. One innovative and inexpensive solution is using pool noodles as bed bumpers. This article provides a comprehensive guide on effectively utilizing pool noodles to create a safe and secure sleeping environment, reducing the risk of falls and injuries. From selecting the right noodles to proper installation techniques, we cover everything you need to know to ensure your loved one's safety and peace of mind.

Discover the art of crafting hospice prayers that resonate with patients’ beliefs, providing comfort and solace in their final journey. Learn from hospice professionals about personalizing this sacred support.

Understanding the nuances between a Cerebrovascular Accident (CVA) and a Transient Ischemic Attack (TIA) can be life-saving. This guide helps family members recognize signs, differentiate between CVA and TIA, and respond swiftly to ensure the best possible care.
We understand that caring for a loved one in hospice can be a journey filled with compassion, love, and sometimes, uncertainty. When seizures are part of this journey, it’s natural to have concerns and questions. This guide is here to walk alongside you, offering knowledge and support as you navigate the complexities of seizure management in hospice settings.

Caring for terminally ill patients in denial can be challenging. This article explores why understanding denial is crucial and offers strategies for compassionate care. Techniques like Naomi Feil's validation therapy and motivational interviewing are highlighted to support patients respectfully, maintaining their dignity and emotional well-being.
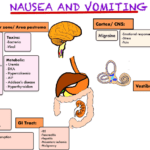
Nausea and vomiting are common and distressing symptoms in terminally ill patients. This comprehensive guide offers practical advice for caregivers and healthcare professionals on managing these symptoms, including pharmacological and non-pharmacological approaches, diet and lifestyle changes, and when to seek additional help.
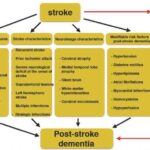
Stroke-induced dementia is a complex condition that affects both patients and their caregivers. In this guide, we’ll explore the impact of strokes on cognitive function, practical caregiving strategies, and considerations for maintaining quality of life.

Unveiling the pivotal events that may fast-track dementia progression. This article delves into how fractures, ulcers, infections, dietary habits, and certain medications like statins play a role in accelerating the onset and severity of dementia symptoms.

Discover critical approaches for hospice nurses and staff to identify and address factors leading to unnecessary discharges. This guide offers practical steps to maintain quality end-of-life care for terminal patients, fostering a stable care environment.

Discover the critical role of trauma-informed care in hospice. This guide provides nurses and staff with the knowledge to support traumatized patients while educating caregivers and family members on providing empathetic end-of-life care.

Discover the top twenty dermatologic conditions prevalent among the elderly. This guide covers symptoms, treatments, and tips for maintaining healthy skin in the golden years. It is perfect for caregivers and healthcare professionals.