Understanding and Addressing Delirium in Terminal Care
Published on January 29, 2025
Updated on January 28, 2025
Published on January 29, 2025
Updated on January 28, 2025
Table of Contents
Caring for a loved one who is terminally ill is a journey filled with love, challenges, and sometimes, confusion. One aspect that can be notably perplexing is when a loved one experiences delirium. This sudden change in their mental state can cause them to be confused, restless, or have trouble paying attention.
Delirium can be a scary experience, both for the person experiencing it and for you, the caregiver. It’s like a thick fog that suddenly rolls in, making everything less clear for your loved one. They might see or hear things that aren’t there or believe things that don’t make sense. It’s important to remember that this isn’t their fault, and it’s not yours either. It’s just a symptom that can happen when someone is very sick.
Delirium can come and go, and sometimes, it can be reversed. This is often called ‘reversible delirium.’ Medications, dehydration, or infections might cause it; treating these can help clear the fog. However, terminal restlessness is a type of irreversible delirium. It can happen in the final stages of life and is a sign that the body is starting to shut down.
As a caregiver, you play a crucial role in helping manage delirium. Your support and understanding can be a light in the fog of confusion. You can help by creating a calm environment, speaking in a soothing voice, and gently reminding your loved one of the time, place, and people around them. It’s also important to talk to their healthcare team about what you’re observing, as they can provide treatments that may help.
Remember, you’re not alone in this. Some resources and people can help guide you through these challenging times. Your love and care make a world of difference to your loved one, even when things seem cloudy.
When someone you love is facing a severe illness, changes in their thinking or behavior can be one of the first signs that something’s not right. This is often delirium. It can start suddenly, and you might notice they’re having trouble focusing, are easily startled, or are not making much sense when they talk. They might see things that aren’t there or get confused about the time or where they are. These early signs are your cue to get help and support.
It’s easy to get mixed up between delirium and dementia because they can look a lot alike. But there’s a big difference: delirium starts quickly and can come and go, while dementia comes on slowly and doesn’t change much from day to day. Consider delirium as a sudden storm and dementia as a slow change of seasons.
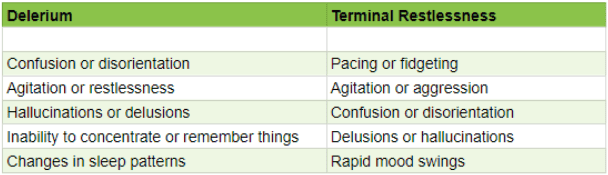
Delirium can be a part of the journey at the end of life, but sometimes it’s different—terminal restlessness. This is when your loved one might seem agitated, restless, or even trying to get out of bed when they’re too weak. It’s tough to see, but knowing it’s a standard part of the process can help you to cope and provide comfort.
To figure out what’s going on, healthcare providers use special tools and techniques. They might ask questions, do tests, or use checklists to see how your loved one’s brain is working. You can help by sharing what you’ve noticed—like changes in sleep, mood, or behavior. Your observations are super valuable in piecing together the puzzle of delirium.
Remember, you’re not alone in this. Nurses, doctors, and other caregivers help guide you and your loved one through this challenging time. Your care and attention can make a big difference in their comfort and well-being.
When a loved one starts showing signs of delirium, it’s like a puzzle. Some pieces of this puzzle are medical things, like infections, insufficient water (dehydration), or side effects from medicines. Other pieces can be about where they are, like if it’s too noisy, too bright, or if they’re in a place they don’t know. All these things can make the brain work differently and cause delirium. It’s important to spot these triggers because, sometimes, fixing them can help clear up the confusion.
Delirium isn’t just about physical stuff. Feelings and thoughts play a big part, too. It can worsen delirium if your loved one is scared, sad, or stressed. It’s like when you’re so worried about something that you can’t think straight. For someone who’s very sick, these feelings can be even more potent and mix up their thoughts more. That’s why being there for them, holding their hand, and listening can be powerful. It helps calm the storm inside and can make a real difference in their well-being.
Remember, you’re doing a fantastic job caring for your loved one. It’s okay to ask for help from doctors or nurses when things get tough. They can work with you to determine the causes of delirium and how to improve things. Your love and care are the most essential medicine.
When delirium appears, it’s like a red flag waving, telling us something’s wrong. It’s essential to play detective and figure out the cause because sometimes, you can fix it. This is what we call ‘reversible delirium.’ It could be an infection, insufficient fluids, or a reaction to a new medicine. By finding the cause, doctors can treat it, and you might see the fog of confusion lift from your loved one.
Consider the following reversible causes and evaluate if the patient is having any of these issues and then address them appropriately:
Pain: Does the patient have unmanaged pain? How is the patient’s pain currently being managed? What changes can take place to manage the patient’s pain better?
Constipation: When was the patient’s last bowel movement? If it has been more than three days or is unknown, treat for constipation unless contraindicated.
Urine retention: If the patient does not have end-stage renal disease and is anuric, are they urinating? Palpate the patient’s bladder and obtain an order for a bladder scan or straight CATH with education that a chronic Foley may need to be placed.
Infection: Assess for UTI, respiratory infection, GI infection, and sepsis. If the infection is found, work with the provider to be clear on communicating known allergies and following any pre-existing orders to treat or not treat infection (some states, like Pennsylvania, allow the POA/family to make that determination). Keep in mind sepsis may not be reversible if caught late.
Recently broken bones or fractures: assess for internal bleeding, remembering blood is a powerful laxative; assess for blood in the stool and any coffee ground emesis. Please keep in mind that if there is internal bleeding, like sepsis, which is caught too late, typical delirium may turn into terminal restlessness that leads to death.
Dehydration: If the patient is awake and alert with an intact gag reflex, are they hydrated enough? If not, encourage fluids.
Medications: Were there recent medication changes—new medications, changing doses, or discontinuing drugs? It may be possible that the medicines were stopped without proper titration. Consider reviewing all the medications the patient is taking with a hospice pharmacist to rule out medication-induced delirium.
Metabolic imbalances: Electrolyte imbalances and metabolic disorders, such as liver or kidney failure, can cause delirium. Treating the underlying condition can help alleviate symptoms. Remember that if the patient has had frequent loose stools or vomiting with emesis, they will have an electrolyte imbalance and dehydration.
There are ways to help ease delirium without using medicines. These are called ‘non-pharmacological interventions,’ they’re all about making your loved one feel safe and comfortable. Simple things like keeping a night light on, having a familiar clock or calendar nearby, and sticking to a routine can make a big difference. Playing their favorite music or bringing in a cherished photo album can also help bring moments of calm and joy.
Sometimes, medications are needed to help manage delirium. These treatments are tools in a toolbox—each has a specific job. Some medicines can help with anxiety or help your loved one sleep better. Others might be used to treat the underlying causes of delirium, like an infection. Working closely with healthcare providers to find the right balance is essential, as these medicines must be used carefully.
Imagine creating a bubble of peace around your loved one. This is what a supportive environment feels like. It’s about making the space around them as calming as possible. Soft lighting, quiet voices, and a tidy room can help reduce stress and confusion. Being there for them, holding their hand, and speaking gently and reassuringly can create a sense of security and love. Your presence is a powerful part of their care.
Caring for someone with delirium can be challenging, but remember, you’re not alone. A whole team of people is ready to help and support you. Your dedication and love are the most important gifts you can give your loved one during this time.
When your loved one is going through delirium, talking to them might feel like trying to send a message through a storm. The key is to be calm and clear. Use simple words and short sentences. It’s okay to repeat yourself if needed. Hearing your voice can sometimes be comforting, even if they seem confused. Remember, it’s not about the conversation making sense; it’s about making them feel safe and loved.
Taking care of someone can be harsh on your heart and mind. It’s like carrying a heavy backpack that gets more packed every day. That’s why taking breaks and talking about your feelings is super important. Joining a support group or chatting with friends can help lighten the load. And don’t forget to take care of your health too. You need to be strong to be there for your loved one.
Sometimes, the delirium can get too hard to handle on your own. If your loved one is in pain, very upset, or if you’re feeling overwhelmed, it’s time to call in the pros. Nurses, doctors, and counselors have special training to help out. They can give you advice, offer treatments, and sometimes, talking to someone who understands can make a big difference.
Hospice care is like a guardian angel, always there, even in the middle of the night. If you’re ever in doubt or need someone to talk to, pick up the phone and call their support number. They help 24 hours a day, seven days a week. You’re not alone in this, and the hospice team is ready to stand with you every step of the way.
Caring for a loved one with delirium can be challenging, but it can also offer moments of deep connection and love. Remember to seek help when needed and take care of yourself. Your strength and compassion are incredible gifts to those you care for.
Caring for a loved one facing the end of their journey is a profound act of love. It’s about more than just medical treatments; it’s about caring for the whole person. This means looking after their body, mind, and spirit. Comprehensive care is like a big, warm blanket that wraps around your loved one, offering comfort from all sides. It’s about managing pain, easing confusion, and filling their days with as much peace as possible. It’s also about supporting you, the caregiver because your well-being is just as important.
Remember, caring for someone at the end of life is one of the most challenging and meaningful things you can do. It’s okay to feel overwhelmed sometimes. Reach out for help, take breaks when needed, and take pride in the love and care you provide. Your role is invaluable, and resources are available to support you every step of the way.
Reversible delirium in terminally ill patients
A Change in Behavior: Delirium, Terminal Restlessness, or Dementia, A Pragmatic Clinical Guide
Delirium in Older Persons: Evaluation and Management
Delirium (booklet / PDF)
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying