Balancing Patient Care and Compliance: The Impact of Extended Hospice Care for Dementia Patients
Published on January 27, 2025
Updated on January 26, 2025
Published on January 27, 2025
Updated on January 26, 2025
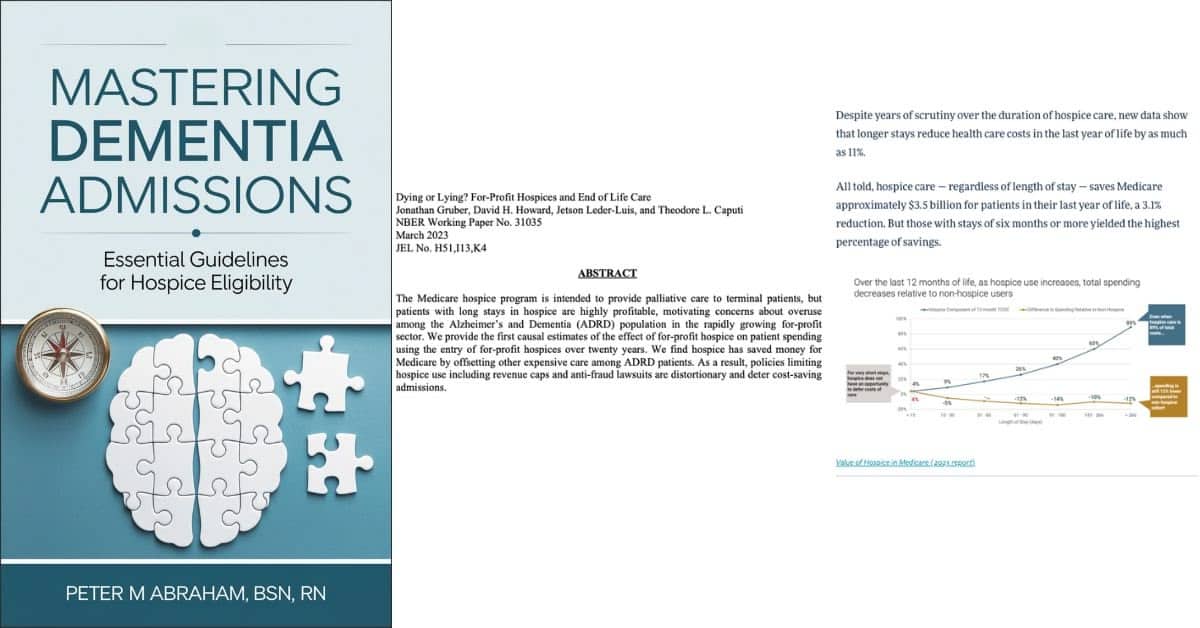
Table of Contents
Extended hospice care creates significant value for everyone involved – from patients and families to healthcare systems and society. Let’s explore these benefits in detail:
The financial benefits of more extended hospice stays are substantial and well-documented:
Medicare Cost Savings
Where the Savings Come From:
| Type of Care | How Hospice Reduces Costs |
|---|---|
| Skilled Nursing | Decreased facility admissions |
| Home Health | Lower utilization of services |
| Hospital Care | Fewer emergency visits and admissions |
| Medications | Reduced pharmaceutical spending |
Enhanced Quality of Life
Family Support Services
Medical Benefits
The benefits of hospice care increase significantly when patients are admitted earlier in their disease progression:
For Patients:
For Families:
For Healthcare Systems:
This comprehensive approach to end-of-life care demonstrates why longer hospice stays benefit everyone involved, creating financial savings and improved care experiences.
The regulatory landscape for hospice providers caring for dementia patients presents unique challenges that require careful navigation and thorough documentation. Let’s explore these challenges and their practical implications:
The Six-Month Rule Challenge
The fundamental requirement that patients have a prognosis of six months or less creates particular difficulties with dementia patients because:
Key Areas of Regulatory Focus
| Area of Scrutiny | What CMS Looks For | Best Practice Response |
|---|---|---|
| Length of Stay | Evidence supporting terminal prognosis | Document all decline indicators, even subtle ones |
| Disease Progression | Ongoing decline documentation | Regular functional assessments with specific examples |
| Recertification | Justification for continued care | Build a comprehensive narrative showing a pattern of decline |
Proving Ongoing Eligibility
To maintain compliance while providing necessary care, focus documentation on the following:
During periods of relative stability, document:
Building Strong Recertification Documentation:
This comprehensive approach to regulatory compliance helps ensure patients receive needed care while meeting CMS requirements. Remember, the goal is to tell the patient’s story clearly and accurately, supporting both quality care and regulatory compliance.
Healthcare providers face significant challenges in delivering hospice care for dementia patients while maintaining regulatory compliance. Let’s explore these challenges and their practical implications:
Operational Differences Between For-Profit and Non-Profit Hospices
| Aspect | For-Profit Agencies | Non-Profit Agencies |
|---|---|---|
| Length of Stay | Typically longer (average 84 days) | Generally shorter (average 65 days) |
| Patient Mix | Higher ADRD population | More cancer diagnoses |
| Financial Pressure | Greater scrutiny on long stays | Less cap pressure |
Managing Length of Stay Effectively
The key challenges in the length of stay management include:
Quality and Outcomes Focus
Hospices must track and improve:
Assessment Challenges
Clinical teams face several key difficulties when assessing dementia patients:
Documentation Requirements
The documentation burden includes:
Care Plan Management Complexities
Teams must address:
To meet these challenges effectively:
This comprehensive approach helps ensure quality care delivery and regulatory compliance while managing the unique challenges of dementia care in hospice.
Navigating dementia care in hospice requires a balanced approach between providing quality patient care and maintaining regulatory compliance. Let’s explore practical solutions that help achieve both goals:
Key Assessment Components
Best Practices for Documentation
| Area to Monitor | What to Document | Frequency |
|---|---|---|
| Functional Status | FAST score changes | Monthly |
| Weight/Nutrition | Weight, intake patterns | Weekly |
| Complications | Infections, falls, wounds | Each occurrence |
| Cognitive Changes | Communication ability, awareness | Each visit |
Physical Decline Indicators
Cognitive Assessment Tools
This comprehensive resource provides practical guidance for:
Documentation Excellence
Clinical Decision Support
Key Documentation Strategies
Team Approach
This structured approach helps ensure quality care delivery and regulatory compliance while supporting appropriate lengths of stay for dementia patients in hospice care.
Improving dementia care in hospice requires a multi-faceted approach that benefits patients, families, and providers while maintaining regulatory compliance. Here’s a comprehensive roadmap for hospice organizations:
Education Priorities
Key Training Areas
| Focus Area | Benefits | Implementation |
|---|---|---|
| Assessment Skills | More accurate eligibility decisions | Monthly case reviews |
| Documentation | Better compliance outcomes | Template training |
| Family Communication | Improved satisfaction scores | Role-play scenarios |
| Care Planning | Enhanced patient outcomes | Mentorship programs |
Essential Components
Implementation Steps
The book Mastering Dementia Admissions: Essential Guidelines for Hospice Eligibility provides:
Clinical Tools
Practical Benefits
This comprehensive approach helps ensure quality care delivery and regulatory compliance while managing appropriate lengths of stay for dementia patients in hospice care.
Dying or Lying: For-Profit Hospices and End-of-Life Care at https://www.nber.org/system/files/working_papers/w31035/w31035.pdf
Hospice Saves Medicare Upwards of $3.5B Annually, with Longer Stays Especially Valuable at https://hospicenews.com/2023/03/22/longer-hospice-stays-lead-to-larger-medicare-cost-savings/
Longer Hospice Stays Among Dementia Patients Save Medicare Dollars at https://hospicenews.com/2024/11/04/longer-hospice-stays-among-dementia-patients-save-medicare-dollars/
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Mastering Dementia Admissions: Essential Guidelines for Hospice Eligibility at https://amzn.to/4j9rLmC
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Holistic Nurse: Skills for Excellence book series
Trivia Games – Caregiver Activities for Alzheimer’s and Dementia
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Holistic Nurse: Skills for Excellence book series
Dementia Home Care: How to Prepare Before, During, and After
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
Fading Reflection: Understanding the complexities of Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)