Category: Nurse Skills
Articles involving nursing skills and techniques.
Articles involving nursing skills and techniques.

This article will delve into common infections in geriatric patients, encompassing early, middle, and late-stage symptoms, preventive measures, and prevalent treatment approaches, particularly for patients facing a terminal illness prognosis of six months or less.
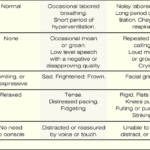
The PAINAD scale is a comprehensive tool that assesses and manages pain in older adults with dementia and delirium. It focuses on observable signs of pain rather than patient self-report, making it particularly useful for individuals who cannot communicate their discomfort
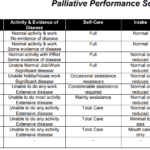
Explore the Palliative Performance Scale (PPS) and its crucial role in end-of-life care. Learn how this tool helps hospice professionals assess patient decline, predict life expectancy, and provide tailored care. Understand the significance of PPS changes in the final six months and how they guide compassionate care decisions.
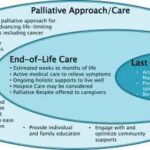
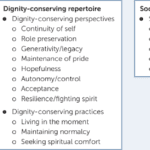
Explore the compassionate approach of hospice nursing assessments, emphasizing patient comfort and dignity over conventional hospital metrics. This article delves into the personalized care that defines hospice evaluations, ensuring a serene transition for patients and families.
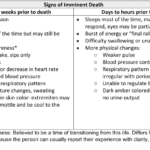
Recognizing end-of-life signs can be challenging. This guide outlines key symptoms indicating a terminally ill patient may have less than two weeks, offering crucial insights for caregivers and families.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.

As a caregiver or family member, it can be challenging to witness the changes that occur as a loved one approaches the end of their life. One such change that may occur is mottled skin, also known as livedo reticularis. Understanding what mottled skin is and its significance in the dying process can help you provide the best care and support to your loved one during this time.
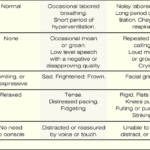
If you have a loved one with dementia, it can be difficult to know if they are in pain or discomfort. The Pain Assessment in Advanced Dementia Scale (PAINAD) is a tool that can help you determine if your loved one is uncomfortable. The Pain Assessment in Advanced Dementia Scale (PAINAD) is different from other pain assessment tools for people with dementia in several ways:

Heart failure is a complex medical condition that can impact the quality of life of patients, especially those in hospice care. As a hospice nurse, assessing the heart failure stage is crucial to providing appropriate care accurately. This article will explore the New York Heart Failure Classification System, its stages, and how to assess patients for their stages. Additionally, we will emphasize the importance of documentation in compliance with Medicare guidelines for terminally ill patients with heart failure.

Medication reconciliation plays a pivotal role in hospice care, ensuring terminally ill patients receive safe medication regimens. This process involves maintaining an accurate medication list to prevent adverse drug events. It's essential at various stages, including admission, recertification, and changes in condition. Healthcare professionals should be familiar with tools like the Beers Criteria and STOPP/START criteria to identify potentially inappropriate medications and prescribing omissions in older adults.

Serotonin syndrome is a potentially life-threatening condition caused by an excess of serotonin in the body. Detecting this condition early is crucial, but it can be particularly challenging when dealing with dementia patients due to communication barriers and the complexity of their symptoms. In this article, we will present three case studies that highlight the early detection and successful management of serotonin syndrome in patients with different types of dementia: Alzheimer's disease, vascular dementia, and Lewy Body Dementia.

Hospice nurses assess the status of the patient's journey towards the end of life every nursing visit. Situations where a reversible condition can drastically impact the patient and the hospice assessment can occur. If it is not caught, it is potentially mistreated, leading to increased discomfort and a faster death, often involving increased suffering. One of the common clues that someone is getting closer to dying is increased agitation and restlessness.
Are you aware of Serotonin Syndrome?
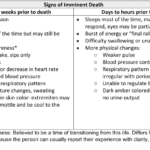
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.

Dementia is a condition that affects millions of people worldwide, and it can cause a range of symptoms, including pain and discomfort. Unfortunately, pain is often under-detected and undertreated in people with dementia, leading to significant suffering and a reduced quality of life. In this article, we will explore the prevalence of pain among dementia patients, the impact of unmanaged pain on their quality of life, behavioral changes that may indicate pain, and the use of the PAINAD pain scale as a tool for assessing and managing pain in dementia patients.

In the realm of hospice care, where empathy and compassion are paramount, a remarkable approach called Validation Therapy has emerged as a beacon of hope and comfort for individuals facing dementia and cognitive disorders in their final journey. As an experienced hospice registered nurse case manager, I've witnessed the transformative impact of Validation Therapy on patients, allowing them to find solace, regain their self-worth, and experience a sense of dignity during their end-of-life phase.
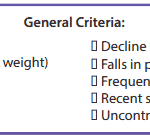
It’s essential to familiarize yourself with the key local coverage determination (LCD) facts for different terminal illnesses to avoid admitting patients who are not eligible for services only to be required to refund the money back to Medicare; otherwise, only have the patient on for one benefit period then discharged for failure to decline. These determinations provide guidelines on the coverage of hospice services for specific conditions. If you are the admitting nurse, please do not just admit because you were told to admit by someone, regardless of the position or standing of the person or party that told you to admit. Use your critical thinking and clinical judgment skills to evaluate the patient for admission. Most doctors will write "evaluate and treat" or something to that effect; never lose sight of the "evaluate" portion of the doctor's order.
Based on the provided PDF files, as noted in the resources section below, let’s explore some essential information for each terminal illness.

Caring for a terminally ill loved one is a profound and challenging journey that requires compassion, understanding, and a willingness to alleviate any discomfort they may experience. In this guide, we will explore the concept of discomfort, its distinction from pain, and the importance of recognizing and addressing discomfort in addition to pain. You'll be better equipped to provide holistic care that enhances your loved one's quality of life during this sensitive time.
Throughout your loved one's illness, you might find yourself thinking that they don't require "pain medication" because they don't seem to be in pain. They might even respond with a direct "no" when asked about their pain. However, are you aware that most types of pain medication can alleviate discomfort? Did you also know that your loved one could be feeling uncomfortable without necessarily being in severe pain? Nonetheless, it's important to recognize that their discomfort requires the same treatment as if they were in pain.
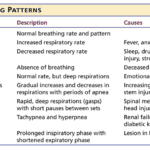
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.

It's common in nursing to be told by others that you shouldn't be a nurse, and some may even call you a "fake nurse" if you don't meet their standards of what they think is required to be a nurse. The first time I was told I could not be a nurse was by an elderly woman who believed only women could be nurses.
This article provides valuable insights for hospice nurses on improving documentation to conquer Medicare audits and ensure claims are not denied due to insufficient evidence of terminal prognosis. The author shares real-life examples of visit narratives before and after implementing documentation best practices learned from an expert. The tips focus on capturing negative condition changes, disorientation levels, and functional decline to paint a clear picture of the patient's terminal state, ultimately leading to better patient care.
Educating nursing home staff on hospice care priorities like shifting focus from vital signs to comfort, managing symptoms like pain/breathlessness, providing psychosocial support, end-of-life planning, and bereavement care is crucial. Hospice emphasizes quality of life over curative treatments. Effective symptom management through medications and non-pharmacological approaches enhances patient comfort. Open communication, empathy, and respecting patient autonomy are essential. Hospice prepares families for the dying process and grief counseling.

Whether you are a new hospice nurse or an experienced one like me, I would hope that it is your desire to prove and support continued hospice eligibility for your patients and families. In my years as a hospice nurse, I've always felt the training on what words and phrases to use to support hospice eligibility was weak compared to the training received in other areas of nursing. Now, you have a means of getting the education you need in a very portable setup that you can take with you, use as you see fit, and bloom!

What does a typical day, a typical week look like for a visiting hospice registered nurse case manager look like?

One crucial aspect for new hospice nurses to grasp is the Hospice Item Set (HIS) requirements. In this article, I’ll explain the HIS requirements for Medicare, providing you with a comprehensive understanding to ensure compliance and quality care delivery.