Category: Palliative Care
Articles about palliative care including the differences between palliative care and hospice care which is palliative care at end-of-life.
Articles about palliative care including the differences between palliative care and hospice care which is palliative care at end-of-life.

Hospice care is often seen as the final chapter, but sometimes, it leads to unexpected recoveries. This article explores stories of resilience and healing in hospice care, reminding us that hope and recovery can still be part of the journey.

Learn about cortical dementia: its symptoms, treatments, and impact on daily life. Get empowered with essential knowledge to navigate this condition.
Discover essential insights into Adult Failure to Thrive—a condition affecting older adults. Learn why early recognition and compassionate care are crucial for improving quality of life.
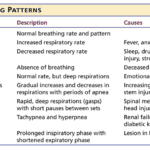
Understanding breathing patterns in end-of-life care is crucial for providing comfort to your loved one. Learn about regular vs. irregular breathing rhythms and when to contact hospice for additional support.
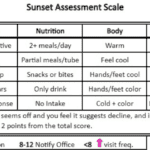
Discover how the Sunset Assessment Scale guides hospice nurses in determining visit frequencies, ensuring compassionate, patient-centered care during the final journey.

Adult daycare can be a great way to support your loved one with dementia. It offers engaging activities and social interaction, while giving caregivers some much-needed respite. Learn how to choose the right center and prepare for the transition.

Discover practical strategies for supporting a loved one with cognitive decline during doctor visits. From preparation to follow-up, learn how to communicate effectively, respect autonomy, and handle sensitive topics. This guide offers valuable tips for caregivers to ensure productive appointments and quality care for their loved ones.

In-home hospice care offers a sanctuary of comfort and support for terminally ill loved ones and their families. It brings medical care, emotional solace, and practical help to your doorstep, allowing patients to spend their final days in the warmth of home. Learn how hospice care can provide personalized support, ensuring dignity and quality of life.

Explore the role of oxygen saturation in hospice care, where comfort takes precedence over numbers. Learn how hospice teams prioritize quality of life, interpret vital signs differently, and make ethical decisions about oxygen use. Discover a compassionate approach focused on dignity and peace.
Dementia can lead to aggressive behavior in elderly patients, causing distress for both them and their caregivers. This comprehensive guide explores the underlying causes of aggression, from sleep disturbances to medication side effects, and offers practical, empathetic strategies for managing these challenging situations and improving the quality of life for all involved.

This comprehensive guide empowers families to navigate care plan meetings for terminally ill loved ones. Learn the significance of these meetings, how to prepare, communicate your loved one's needs, and advocate for their best interests. Gain insights into recognizing when meetings are necessary and the benefits of regular care planning. Equip yourself with the knowledge to ensure your loved one receives personalized, dignified care aligned with their wishes.

When a loved one is facing a serious illness, it can feel like standing at a crossroads. Each path represents a different way to care for them in their time of need. It’s a moment filled with tough choices and deep emotions. This article thoroughly explains hospice care, its philosophy, and the benefits it provides to patients and families facing terminal illness. Learn about the decision-making process, the hospice experience, and how to navigate this difficult choice with dignity and love.

Dementia is a word we use to describe a significant change in the brain that makes it hard for people to remember things, think clearly, make decisions, or even control their emotions. It’s like a fog that slowly creeps in, affecting how a person thinks, feels, and lives daily. It’s not just one disease but a group of symptoms that can be caused by different diseases, including Parkinson’s and Alzheimer’s.

Vitamin B deficiencies can lead to severe health issues mimicking terminal diseases like nerve damage, anemia, and increased cancer risk. This comprehensive guide explores the symptoms, causes, diagnosis, and treatment options for vitamin deficiencies B1, B2, B3, B5, B6, B7, B9, and B12. Understand the importance of adequate vitamin B intake for energy production, metabolism, cell growth, and overall well-being.
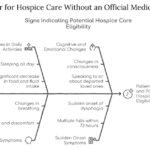
This article aims to provide information and guidance on qualifying for hospice care without an official medical diagnosis. We will explain hospice care, how to access it without a physician’s consent, what to expect, and how to make the most of it.

Hospice care focuses on comfort rather than curative treatments. In emergencies, calling 911 can lead to invasive procedures and disrupt hospice care. This article explores why contacting your hospice provider first is crucial and offers guidance on alternatives to calling 911.

If you are caring for a loved one with pulmonary fibrosis, you may have many questions and concerns about their condition and how to support them best. You may also feel overwhelmed, stressed, or isolated by the challenges and responsibilities of caregiving. You are not alone. Many people face similar situations and emotions when caring for someone with chronic and progressive lung disease.
This article will help you understand pulmonary fibrosis and how it affects your loved one and yourself. It will also provide practical and helpful information on providing the best care for your loved one and yourself.
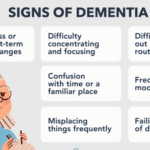
Learn to recognize early dementia signs and explore care options, including hospice. This guide offers insights into dementia, practical care tips, and when to seek professional help.

Caring for a loved one with dementia in rural areas can be challenging when local care facility options are limited. This guide explores alternatives, such as contacting organizations like the Alzheimer's Association, considering different facility types (adult day care, long-term care, respite care, memory care), seeking financial assistance, evaluating hospice eligibility, and assessing life plan/continuing care communities. It also addresses the legal and ethical implications of using hospitals as a last resort.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.
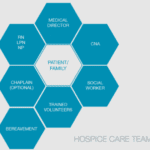
Hospice care is about providing compassionate support and comfort to patients during their end-of-life journey. Interdisciplinary Group (IDG) meetings ensure the highest quality care for hospice patients and their families. These meetings bring together a diverse team of professionals to discuss patient care plans, address concerns, and collaborate on providing holistic support. However, these meetings can sometimes become overwhelming and time-consuming. Let's explore some best practices to make the most of IDG meetings while keeping patient-centered care at the forefront.
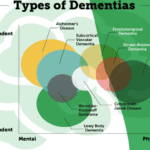
This article summarizes the twelve known types of dementia, which are the most common and well-studied forms of this condition. You will learn about the signs and symptoms of each type, how they are diagnosed, what causes them, and how they are treated. This article is intended for family members and caregivers of people with dementia who may want to understand more about the condition and how to support their loved ones.
Explore the complex world of dementia-related aggression and learn how to identify its underlying causes. This comprehensive guide offers insights into medication-related issues, pain management, and non-pharmacological interventions. Discover compassionate care strategies to support patients and caregivers on this challenging journey.
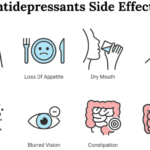
Dive into the world of Selective Serotonin Reuptake Inhibitors (SSRIs) and their role in treating depression. Discover the importance of medication half-life, the risks of serotonin syndrome, and why the chemical imbalance theory of depression is being challenged. Learn about the concerns of overprescription in older adults.