Hospice General Inpatient Care: a Guide for Families and Nurses
Published on July 22, 2024
Updated on July 4, 2025
Published on July 22, 2024
Updated on July 4, 2025
Table of Contents
Hospice care focuses on improving the quality of life for patients with life-limiting illnesses and their families. It provides physical, emotional, and spiritual support to help patients cope with their condition and prepare for the end of life. Hospice care can be provided in various settings, such as the patient’s home, a hospice facility, a nursing home, or a hospital.
However, sometimes hospice patients may experience severe pain or other symptoms that cannot be adequately controlled in their current setting. In such cases, they may need a higher level of care that can only be provided in an inpatient setting. This is called hospice general inpatient care, or GIP for short. GIP is a short-term level of care that aims to stabilize the patient’s condition and relieve their suffering. GIP is not a permanent placement but a temporary intervention that can be discontinued when the patient’s symptoms improve or they return to their previous setting.
GIP can offer many benefits for hospice patients and their families. It can help patients better manage pain and symptoms, enhancing their comfort and dignity. GIP can also help families reduce their stress and burden, as they can rely on the professional care and guidance of the hospice team. GIP can also allow families to spend quality time with their loved ones without worrying about their medical needs.
In this article, we will explain everything you need to know about GIP, including:
We hope this article will help you understand GIP better and make informed decisions for yourself or your loved one. If you have any questions or concerns about GIP, don’t hesitate to contact your hospice provider or refer to your hospice handbook for more information and support.
Not every hospice patient is eligible for GIP. GIP is only appropriate for patients who have severe pain or other symptoms that cannot be managed in different settings, such as their home, a nursing home, or an assisted living facility. GIP is not a substitute for long-term care or custodial care. GIP is also not a choice that patients or families can make alone. GIP requires a medical justification and a written order from the hospice medical director or the patient’s attending physician.
GIP can be provided in one of the following three settings:
The hospice must have a written agreement with the hospital or SNF to provide GIP care. The contract must specify the hospice and facility’s roles and responsibilities, such as admission and discharge procedures, billing and payment arrangements, quality assurance, and patient rights.
The common conditions and symptoms that may qualify a patient for GIP include, but are not limited to:
The role of the hospice medical director and the interdisciplinary team is to determine and document the need for GIP. The hospice medical director or the patient’s attending physician must certify that the patient is terminally ill (with a life expectancy of six months or less) and that GIP is medically necessary for pain or symptom management. The hospice interdisciplinary team, which consists of the hospice medical director, the patient’s attending physician (if any), the hospice nurse, the hospice social worker, the hospice chaplain, and the hospice aide, must develop and update a written plan of care that specifies the goals, interventions, and expected outcomes of GIP. The hospice interdisciplinary team must also coordinate and communicate with the facility staff where GIP is provided and regularly monitor the patient’s condition and progress. The hospice interdisciplinary team must document the patient’s status, symptoms, medications, treatments, and response to GIP in the patient’s medical record. The hospice interdisciplinary team must also review the patient’s eligibility and appropriateness for GIP at least every 24 hours and discharge the patient from GIP when the patient’s symptoms improve or when the patient requests to return to another level of care.
False: The GIP level of care is intended for “short-term” interventions. However, there is no limit to the number of days. This level of care can persist as long as necessary to achieve the goals of palliation. CMS heavily scrutinizes GIP care, which lasts longer than five days, to ensure appropriate use.
False: GIP is not an automatic level of care when a patient is imminently dying. There must also be pain or symptom management, and skilled nursing needs must be present that could not be managed at home.
False: It is not intended for caregiver respite, to address unsafe living conditions, or to address the lack of a caregiver. A skilled nurse must manage the symptoms.
GIP hospice is a level of care that can help hospice patients who have severe pain or symptoms that cannot be managed in other settings. GIP hospice is not a place to live but a place to get better. GIP hospice is only for a brief time until the patient’s condition improves or they choose to go back to their home or another setting.
GIP hospice can be provided in one of the following three types of facilities:
The hospice team and the inpatient staff have different roles in coordinating GIP hospice care. The hospice team is responsible for:
The inpatient staff is responsible for the following:
GIP hospice care in a hospital setting can have both benefits and challenges. Some of the benefits are:
Some of the challenges are:
The following are essential requirements to remember for GIP:
Many different scenarios would meet the requirements for GIP care. Each situation is unique and should be discussed with the case manager, clinical supervisor, medical director, and other IDG members to determine if GIP care is appropriate.
The symptoms below require a nurse to observe, intervene, and monitor them to achieve palliation or resolution. Management of the symptoms should not be something that could be provided in the home setting.
Severe, uncontrolled symptoms:
Severe/uncontrolled symptoms require the following for management:
Please remember there are specific times when GIP is not appropriate, such as:
GIP hospice is a level of care that can help hospice patients who have severe pain or symptoms that cannot be managed in other settings. GIP hospice is not a place to live but a place to get better. GIP hospice is only for a brief time until the patient’s condition improves or they choose to go back to their home or another setting.
One of the most frequent questions patients and families have about GIP hospice is: how long does it last? The answer is that it depends. GIP hospice does not have a fixed or predetermined length of stay. GIP hospice is individualized to the needs and preferences of each patient. Some patients may need GIP hospice for only a few days, while others may need it for longer. The average length of stay in GIP hospice is about six to twelve months, but it can vary depending on the disease, the patient’s ability to fight off the disease, and any treatments the patient is receiving.
The hospice team and the inpatient staff assess the patient’s condition and symptoms daily. They also review the patient’s plan of care and treatment goals. They check if the patient is still eligible and appropriate for GIP hospice or ready to be discharged to another level of care. The hospice team and the inpatient staff regularly communicate with the patient and family and involve them in decision-making. They also document the patient’s status, progress, and response to GIP hospice in the patient’s medical record.
The hospice team and the inpatient staff also plan for the discharge and transition of the patient from GIP hospice to another level of care. They consider the patient’s wishes, comfort, safety, and quality of life. They also consider the availability and readiness of the patient’s caregivers and the resources and support they may need. The hospice team and the inpatient staff coordinate with the patient, the family, and the receiving facility or agency to ensure a smooth and safe transfer. They also educate the patient and the family on continuing the hospice care at home or in another setting.
After GIP hospice, the patient and the family have different options and resources to continue hospice care. The most common option is to return to the routine home care level of hospice, which is provided in the patient’s home or other residence. The hospice team will visit the patient and the family regularly and provide nursing, hospice aide, and other services as needed. The hospice team will also be available 24/7 by phone for any questions or concerns. The patient and the family can also access other hospice services, such as social work, chaplaincy, grief, and volunteer support.
Another option is to receive a continuous home care level of hospice, which is provided in the patient’s home or other residence when the patient has a crisis or emergency that requires more intensive care. The hospice team will provide continuous nursing care for at least eight hours a day and may also offer other services as needed. The hospice team will stay with the patient and the family until the crisis or emergency is resolved or until the patient is stable enough to return to the routine home care level of hospice.
A third option is to receive respite care level of hospice, which is provided in an inpatient facility for up to five days at a time when the patient’s caregivers need a break or relief from the stress and burden of caregiving. The hospice team will arrange for the patient’s admission and transportation to the inpatient facility and will continue to oversee the patient’s care and care plan. The hospice team will also coordinate with the patient’s caregivers and the inpatient facility to plan for the patient’s discharge and return to the routine home care level of hospice.
The hospice team will provide the patient and the family with information and guidance on the different options and resources for hospice care after GIP hospice. The hospice team will also respect the patients’ and the families’ choices and preferences and honor their rights and dignity. The hospice team will support the patient and the family throughout the hospice journey and help them cope with the physical, emotional, and spiritual challenges of the end of life.
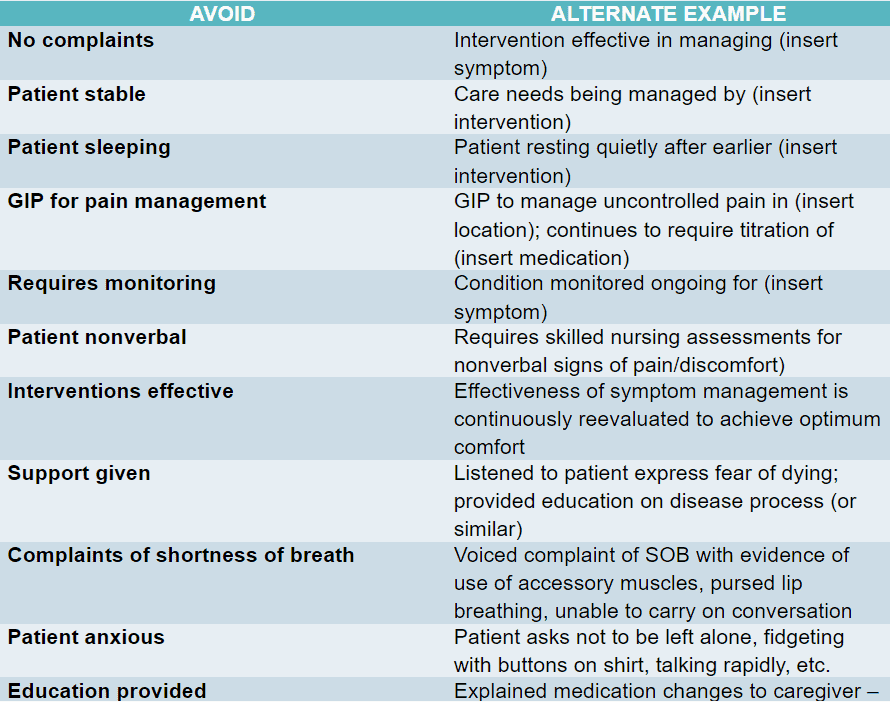
Documentation must support the need for the level of care. This means the documentation must show that the patient’s condition could NOT be
managed in the home setting. Documentation for the GIP level of care should paint a picture of the patient’s appropriateness for hospice and the increased level of care.
Documentation must include:
GIP is a level of care that can help hospice patients with severe pain or symptoms that cannot be managed in other settings. It is not a place to live but a place to get better. GIP is only for a brief time until the patient’s condition improves or they choose to return to their home or another setting.
One of the most important things to remember about GIP is that it is intended to be a short-term intervention, not a permanent placement. GIP is not a substitute for long-term care or custodial care. GIP is also not a choice that patients or families can make alone. GIP requires a medical justification and a written order from the hospice medical director or the patient’s attending physician.
The goal of GIP is to stabilize the patient’s condition and relieve their suffering so that they can return to their home or another setting where they can receive routine hospice care. GIP is not meant to prolong the patient’s life or cure their illness, hasten the patient’s death, or cause them harm. GIP is intended to enhance the patient’s comfort and dignity and support the patient’s and the family’s wishes and preferences.
The hospice team and the inpatient staff work together to plan for the discharge and transition of the patient from GIP to another level of care. They consider the following criteria for discontinuing GIP:
The hospice team and the inpatient staff regularly communicate with the patient and family and involve them in decision-making. They also document the patient’s status, progress, and response to GIP in the patient’s medical record. They also educate the patient and the family on continuing hospice care at home or in another setting.
The hospice team and the inpatient staff also provide tips and resources for ensuring a smooth and safe transition from GIP to home or another level of care. Some of the tips and resources are:
The hospice IDG is responsible for the professional management of the patient’s care by the hospice plan of care. To ensure effective
management and continued eligibility for the GIP level of care, consider the following:
In conclusion, Hospice General Inpatient Care (GIP) is a crucial level of care that aims to stabilize a patient’s condition and relieve their suffering when severe pain or symptoms cannot be managed in other settings. This article has provided comprehensive information on GIP, including eligibility criteria, the role of the hospice team, myths about GIP care, where and how GIP hospice is provided, documentation requirements, and the discharge and transition from GIP. It emphasizes the temporary nature of GIP and the importance of patient preference, symptom improvement, and changes in prognosis in determining the transition from GIP to another level of care.
The article underscores the collaborative approach between the hospice team and inpatient staff in coordinating GIP care and planning for the patient’s discharge. It also highlights the assorted options available for continuing hospice care after GIP, such as routine home care, continuous home care, and respite care, focusing on respecting the patient’s and family’s choices and preferences.
This article addresses the essential requirements and considerations for GIP to empower families and nurses to make informed decisions and ensure a smooth and safe patient transition. It emphasizes the compassionate and person-centered approach of hospice care, aligning with the values of empathy and compassion that are fundamental to end-of-life care.
For further information or support regarding GIP, readers are encouraged to contact their hospice provider or refer to their hospice handbook. This article is a valuable resource for those navigating the complexities of hospice care, aiming to enhance the quality of life for patients with life-limiting illnesses and their families.
General Inpatient (GIP) Level Of Care For Hospice Explained
NHPCO_GIP_Compliance_Guide (PDF
GIP_FAQs (PDF)
Carolinas_Center_GIP_Resource_Guide (PDF)
GIP Documentation Toolkit (PDF)
How Long Will Hospice Care Last? What is The Average Time in Hospice for Cancer Patients
How Long Does a Hospice Patient Live?
How Long Does the Average Hospice Patient Stay Under Care?
Live_Discharge_Toolkit (PDF)
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
The Importance of Caregiver Journaling
Reporting Changes in Condition to Hospice
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death