Category: About Hospice
Articles about hospice dispelling myths and bring more light to end-of-life topics.
Articles about hospice dispelling myths and bring more light to end-of-life topics.

When a loved one is facing a serious illness, it can feel like standing at a crossroads. Each path represents a different way to care for them in their time of need. It’s a moment filled with tough choices and deep emotions. This article thoroughly explains hospice care, its philosophy, and the benefits it provides to patients and families facing terminal illness. Learn about the decision-making process, the hospice experience, and how to navigate this difficult choice with dignity and love.
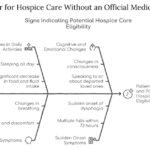
This article aims to provide information and guidance on qualifying for hospice care without an official medical diagnosis. We will explain hospice care, how to access it without a physician’s consent, what to expect, and how to make the most of it.

Hospice care focuses on comfort rather than curative treatments. In emergencies, calling 911 can lead to invasive procedures and disrupt hospice care. This article explores why contacting your hospice provider first is crucial and offers guidance on alternatives to calling 911.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.
Hospice care focuses on comfort, not curing illness. But what if an emergency arises? This guide explains when hospice covers emergency care, how to proceed, and how hospice services continue during/after hospitalization - ensuring you make informed decisions without losing benefits.

Discover the unsung heroes of hospice care: primary caregivers. From family members to trained professionals, these compassionate individuals provide essential support to patients nearing the end of life. Learn about their crucial roles, challenges, and their impact in ensuring comfort and dignity for hospice patients.
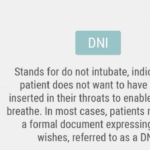
If you or your loved one has a severe illness, you may have heard about do not resuscitate (DNR) orders. This medical order tells the health care team what to do if the patient’s heart stops beating or they stop breathing. It is an incredibly crucial decision that can affect the quality and length of life. However, there are many myths and misunderstandings about DNR orders that can make it hard to choose what is best for you or your loved one. In this article, we will explain what DNR orders means and why it is important to understand it. We will also debunk the top ten myths about DNR orders and share the facts that can help you make an informed and respectful choice.

You may think that CPR is a miracle that can save anyone’s life, but that is not always the case. CPR is not practical for terminally ill patients, and it can cause more harm than good. In fact, studies show that only about 5% of terminally ill patients who receive CPR survive to leave the hospital. Many of them suffer from brain damage, broken ribs, or infections because of CPR.
This article aims to help you understand the truth about CPR for terminally ill patients. We will debunk ten common myths you may have heard or believed about CPR and provide you with accurate and reliable information. We will also help you make informed and respectful decisions about CPR for your loved one based on their wishes and values.

Navigating the prognosis of six months or less for hospice care can be daunting. Learn how to understand, prepare for, and make the most of this crucial time.

Shielding children from death deprives them of understanding this natural part of life, leading to emotional and psychological consequences. This article explores why exposing children to the dying process is essential for their development and highlights the role of hospice care in supporting families during this time.

Hospice General Inpatient Care (GIP) provides short-term, intensive care for patients experiencing severe pain or symptoms that can't be managed at home. Learn about GIP eligibility, benefits, and how it helps both patients and families during challenging times. Discover key details and important considerations for this essential hospice service.
Discover the language of compassionate end-of-life care with this guide to common medical abbreviations and terminology in hospice. From team member roles to levels of care and clinical terms, this article provides valuable insights for patients, families, and caregivers navigating the hospice journey.

Learn about various financial assistance options available for terminally ill patients who need hospice or palliative care but lack Medicare, Medicaid, private insurance, or the means to self-pay.

In this episode of Hospice Explained, host Marie Betcher, RN, interviews Nurse Peter Abraham. Peter shares his extensive experience in cardiac telemetry, skilled nursing, and rural home hospice care. They discuss the significance of early hospice enrollment, the challenges of caring for dementia and Parkinson's patients, and the impactful personal stories from Peter's career. Special focus is given to the educational resources on Peter's website, Compassion Crossing, which aims to support families, caregivers, and new hospice nurses. Peter emphasizes the importance of compassion and understanding in hospice care and reflects on how his faith informs his practice.
Understanding when and how to revoke services is crucial in hospice care. This article aims to shed light on revoking hospice services, why it may be necessary, misconceptions surrounding it, and the potential impact when patients or their families decide to restart hospice care.

Navigating interstate hospice transfers can be complex. This guide explores the process, challenges, and considerations for patients and families. Learn about Medicare regulations, coordination between hospice agencies, and how to ensure continuity of care when moving across state lines during end-of-life care.

Hospice care is a unique medical approach that prioritizes comfort and peace for the terminally ill rather than vital signs or curative treatments. It offers holistic support, addressing physical, emotional, and spiritual needs. This compassionate care improves the quality of life, dignity, and a peaceful end aligned with the patient's values.

Caring for a terminally ill loved one can be challenging and emotional. As an experienced hospice nurse case manager, you understand the importance of providing compassionate care and support to loved ones and their families. In this educational article, we will explore the common journey that terminally ill loved ones and their caregivers face as they approach the end of life. We will summarize this journey's various aspects, offering guidance and separating fact from fiction.
The end-of-life journey can be challenging and emotional for patients and their loved ones. A dedicated team of professionals provides comfort, support, and holistic care in hospice care. Each team member has a unique role, ensuring the patient's physical, emotional, and spiritual needs are met. Let's explore the roles of different hospice team members and how they contribute to your care journey.
In the realm of nursing, the spirit of Florence Nightingale, the pioneer of modern nursing, continues to illuminate the path for nurses across various specialties. Her legacy, rooted in compassion, patient-centered care, and unwavering dedication, resonates deeply with nurses from all walks of life. However, we discover a profound connection to Florence Nightingale's nursing model within hospice nursing. This article will explore the distinctive qualities that set hospice nurses apart, including their remarkable autonomy, acute assessment skills, problem-solving abilities, and holistic approach to patient care.

Hospice is very different from other kinds of nursing and health care. Most of us know that doctors and nurses in hospitals, clinics, nursing homes, and other places care a lot about numbers. They check your heartbeat, blood, and other things to see if they are normal. Sometimes, they do things that make you uncomfortable, like putting a tube in your nose, because they want to fix the numbers. But they don’t always think about how you feel. They are trying to fix the numbers, not you, the person. This short story shows you how non-hospice and hospice nurses are different. A hospice nurse cares more about you, the person.

If you or someone you love has a serious illness that cannot be cured, you may have heard of hospice care. Hospice care is a special kind that focuses on making the patient comfortable and peaceful in their final days. Hospice care also supports the family and caregivers emotionally and spiritually.
When a patient joins hospice care, they will have a special meeting with a hospice nurse. This meeting is called the post-admission visit. It is an especially important visit because it will help the patient and the family get to know the hospice team and learn more about the care they will receive.
This article will explain what to expect and what to ask during the post-admission visit. We will also provide tips and resources to help you and your loved one make the most of this time. We hope this article will help you feel more prepared and confident about the hospice journey.

If you or someone you love is facing a terminal illness, you may feel overwhelmed by the physical, emotional, and spiritual challenges that come with it. You may wonder how to cope with the pain, the fear, the grief, and the loss of control. You may also want to find ways to make the most of the time you have left and to leave a lasting legacy for your loved ones.
Music therapy is a form of therapy that can help you and your family deal with these issues. It involves using music and musical activities to improve the health and well-being of people of all ages and backgrounds. Music therapy can help you express your feelings, communicate with others, relax your body and mind, cope with pain and stress, enhance your spiritual connection, and create a meaningful life story.

Dive into the contrasting philosophies of purist and non-purist hospice nurses and doctors. Understand how their views on medication and patient care differ, shaping the terminal phase of a patient’s journey. This article highlights the delicate balance between medical intervention and quality of life in hospice care.