Hospice Care Eligibility: Understanding the Six-Month Rule
Published on April 12, 2024
Updated on August 28, 2024
Published on April 12, 2024
Updated on August 28, 2024
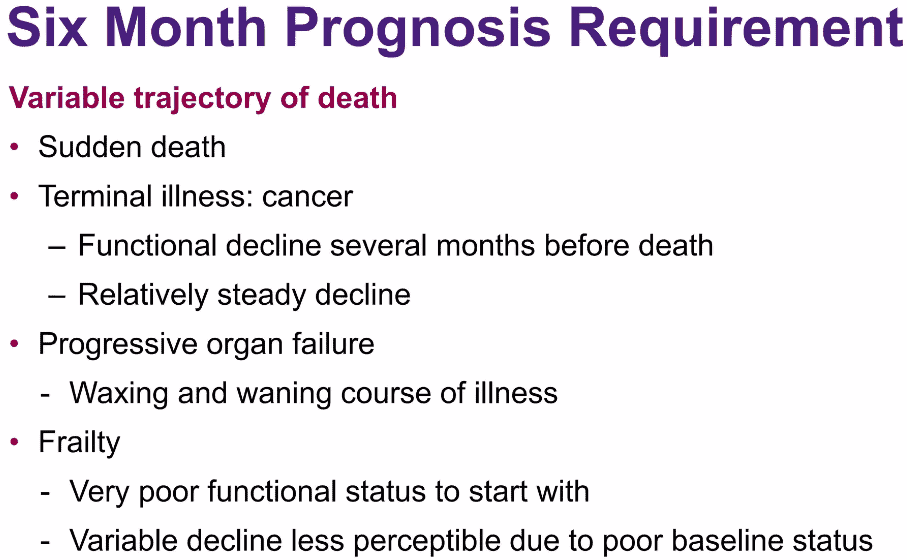
Table of Contents
When a loved one is facing a serious illness, understanding the care options available can be overwhelming. Hospice care is one such option that often comes with many questions and, sometimes, misunderstandings. Let’s take a moment to clear the air.
Hospice care is designed to provide comfort and support to people in the final phase of a terminal illness. It focuses on caring, not curing. The goal is to enable patients to be comfortable and pain-free and live as fully as possible daily.
You might have heard that hospice is only for the last moments of life, but that’s not the whole story. In the United States, hospice care is available to those with a prognosis of six months or less to live if the disease follows its usual course. But it’s not just about counting days; it’s about making days count.
Hospice care teams are compassionate professionals who offer medical care, pain management, and emotional and spiritual support tailored to the patient’s needs and wishes. They also support family members, helping them cope with their unique challenges.
It’s important to know that while there are different levels of care within the hospice system, these levels are about the intensity of care, not how soon someone needs to be in hospice. The six-month prognosis is a guideline for eligibility, not a strict deadline.
We hope this introduction helps you understand the heart of hospice care. It’s about bringing quality to your time with your loved one, surrounded by care and support.
When we talk about hospice care, there’s a vital piece of information that often comes up: the six-month terminal prognosis criterion. It might sound technical, but it’s a simple and important concept.
Doctors and hospice care teams use this six-month guideline to determine when a patient may be ready for hospice. It means that if a patient’s illness is likely to follow its natural course, as understood by their doctor, they could have six months or less to live. It’s not a strict rule but rather a way to help families and patients plan for hospice care at the right time.
It’s important to remember that this is just a guideline. Some patients may live longer than six months once they start hospice care, and that’s okay. The focus is on the quality of life, not the quantity of days. Hospice care is about providing comfort, dignity, and respect to your loved one during their final chapter.
The six-month prognosis also doesn’t mean that care stops if your loved one lives beyond six months. Hospice care continues as long as the care team and the patient’s doctor agree it’s still the right choice.
We know that thinking about hospice care can bring a mix of emotions. It’s a time of tender moments and tough decisions. However, knowing the six-month prognosis criterion can help you feel more prepared and informed. It’s a step towards ensuring your loved one receives the care they need when needed.
To be eligible for hospice services, a patient must be considered terminally ill, meaning they have a life expectancy of six months or less if their illness runs its normal course. This six-month terminal prognosis is a key requirement, distinct from simply having a terminal diagnosis. A terminal diagnosis indicates that a patient has an incurable, progressive illness that will ultimately lead to death. However, a terminal diagnosis alone does not guarantee a six-month or less prognosis. Patients with chronic, life-limiting conditions may have a terminal diagnosis but a longer life expectancy. The six-month terminal prognosis is a clinical judgment made by the physician based on the patient’s overall health status, disease progression, and other factors. This prognosis must be supported by documentation in the medical record, including details on the patient’s condition, symptoms, and trajectory of decline.
Once a patient is admitted to hospice, the hospice provider must continue to demonstrate that the patient’s prognosis remains six months or less. This is typically done through regular clinical assessments and documentation of the patient’s changing condition. Hospice providers must submit this evidence to Medicare to justify the patient’s continued eligibility for hospice benefits. Failure to adequately document the terminal prognosis can result in denial of payment for hospice services. The documentation should include objective, quantifiable measures of the patient’s decline, such as changes in weight, diagnostic test results, pain levels, functional status, and other clinical indicators. Vague statements about “disease progression” or “slow decline” are not sufficient to support the terminal prognosis. By maintaining thorough documentation and demonstrating the patient’s terminal prognosis, hospice providers can ensure that eligible patients receive the compassionate, end-of-life care they need during their final months.
As we navigate the journey of hospice care together, it’s important to understand that different levels of care are available. These levels are designed to meet the changing needs of your loved one as they progress through their illness.
Routine Home Care This is the most common level of hospice care. It involves regular visits from hospice staff to your loved one’s home, whether that’s a private residence, nursing home, or assisted living facility. The focus here is on managing symptoms and providing emotional and spiritual support.
Continuous Home Care is available when your loved one needs more support. This means that hospice staff may stay at home for extended periods, sometimes 24 hours, to manage acute symptoms that can’t be handled with routine care.
Inpatient Respite Care Caring for a loved one can be intense; sometimes, caregivers need a break. Inpatient respite care allows your loved one to be temporarily cared for in a hospice facility, hospital, or nursing home, giving you time to rest and recharge.
General Inpatient Care If pain or symptoms become too difficult to manage at home, general inpatient care may be necessary. This level of care is provided in a hospice facility or hospital where specialized staff can address complex needs.
It’s crucial to know that these levels of care are not about eligibility; they’re about providing the right care at the right time. Your loved one’s eligibility for hospice is based on their medical condition and the six-month prognosis, but once they’re in hospice, the level of care can adjust based on their needs.
We’re here to ensure your loved one receives compassionate care that respects their dignity and choices. Each level of care is a step we take together, ensuring comfort and support every step of the way.
It’s common to hear the terms palliative care and hospice care used interchangeably, but they are not quite the same. Both focus on comfort and quality of life but serve unique needs at various times in a patient’s journey.
Palliative Care: Comfort at Any Stage Palliative care is specialized medical care for people with serious illnesses. This type of care focuses on relieving the illness’s symptoms and stress, to improve the patient’s and family’s quality of life.
Palliative care can be provided at any stage of illness, along with treatment meant to cure you. It involves a team of doctors, nurses, and other specialists working with a patient’s other doctors to provide extra support. It is appropriate for any age and stage of a serious illness and can be provided alongside curative treatment.
Hospice Care: Support When Cure Is Not Possible Hospice care, on the other hand, is a type of palliative care for people nearing the end of life. When a cure is no longer possible, and a patient is expected to have six months or less to live, hospice care becomes the option. It provides comprehensive comfort care as well as support for the family, but treatments aimed at curing the illness are stopped.
The Overlap between palliative and hospice care provides comfort. Palliative care can begin at diagnosis and at the same time as treatment. Hospice care begins after treatment of the disease is stopped and when the person is not going to survive the illness.
The Difference The main difference is the stage of the disease. Palliative care is available to you at any time during your illness. Hospice care is available when you are expected to live six months or less.
Understanding these differences can help you make the best choices for your loved one’s care. Remember, it’s about adding life to days, not just days to life. We’re here to support you and your loved one every step of the way.
Finding your way through the hospice care system can seem daunting, but it’s a path you don’t have to walk alone. Here are some steps to help you access the care and support your loved one needs.
Step 1: Understanding Eligibility: The first step is understanding that hospice care is for patients with terminal illnesses who have a physician-determined prognosis of six months or less to live. It’s about quality of life, ensuring comfort and dignity.
Step 2: Starting the Conversation Talk with your loved one’s doctor about their health and whether hospice care might be the right choice. This conversation can be tough, but planning for your loved one’s care is crucial.
Step 3: Choosing a Hospice Provider Once you’ve decided on hospice care, you must choose a provider. Look for one that fits your loved one’s needs and values. Don’t hesitate to ask questions about their services and support.
Step 4: Coordinating with Insurance Check with your insurance provider to understand what hospice services are covered. Most costs are typically covered under Medicare, Medicaid, or private insurance plans.
Step 5: Developing a Care Plan Work with the hospice care team to develop a personalized care plan. This plan will outline the types of care your loved one will receive, focusing on comfort and managing symptoms.
Step 6: Receiving Care at Home Most hospice care is provided at home, allowing your loved one to be in a familiar and comfortable setting. The hospice team will make regular visits and be available for support 24/7.
Step 7: Adjusting Care as Needed As your loved one’s needs change, the hospice team can adjust the level of care. Whether it’s routine care or more intensive support, they will ensure your loved one’s needs are met.
Step 8: Supporting the Family Remember, hospice care is also there for you, the family. From counseling services to help with daily tasks, the hospice team is there to support you through this journey.
Navigating the hospice care system is about finding the best way to support your loved one’s final chapter with grace and love. It’s a journey of care, comfort, and compassion, and we’re here to guide you every step.
Navigating the healthcare system can be complex, especially when understanding coverage for hospice care. Let’s break down how Medicare supports this essential service.
Medicare Coverage for Hospice Care Medicare Part A (Hospital Insurance) covers hospice care for patients with certain conditions. This means that if your loved one is eligible, Medicare can help cover the costs of care designed to provide comfort and support during a terminal illness.
Conditions for Hospice Care To qualify for hospice care under Medicare, two main conditions must be met:
Signing Up for Hospice Care Once the doctors provide certification, you must sign a statement choosing hospice care. This choice means opting for comfort over cure, focusing on quality of life.
Where Hospice Care Can Be Provided Medicare-certified hospice care can be provided in various settings, including your loved one’s home, a nursing home, or an inpatient hospice facility.
Costs Covered by Medicare With Medicare, you pay nothing for hospice care services. This includes doctor services, nursing care, medical equipment, and supplies for symptom control and pain relief. There may be a small copayment for outpatient drugs and inpatient respite care, but these costs are minimal.
Certifications Required For ongoing hospice care, the medical director or hospice physician must periodically recertify that your loved one is still terminally ill. This is a standard part of maintaining eligibility for hospice benefits under Medicare.
Understanding these Medicare and hospice care aspects can provide peace of mind during a challenging time. It ensures that your loved one receives the compassionate care they deserve without the added stress of financial burden.
When it comes to hospice care, many families have questions. Here are some answers to common concerns that might help you feel more at ease.
Can we still see our regular doctor after starting hospice?
Absolutely. Hospice care is an addition to the care you’re already receiving. Your regular doctor can work with the hospice team to ensure your loved one’s comfort and care.
What if my loved one lives longer than six months?
If your loved one lives beyond six months, they can still receive hospice care if they are in a terminal state. The care team will review their condition and can recertify them for additional time in hospice IF they are still considered to be in a terminal state.
Does hospice mean giving up hope?
Not at all. Hospice is about hope for quality of life, making the most of each day, and ensuring your loved one is comfortable and dignified.
Will hospice help with non-medical needs?
Yes, hospice provides comprehensive support, including help with daily activities, counseling, and spiritual care for patients and families.
Can hospice care happen at home?
Yes, most hospice care is provided at home, but it can also be given in a facility if that’s what your loved one needs.
How do we pay for hospice?
Medicare, Medicaid, and most private insurance plans cover hospice care. The hospice team can help you understand your coverage.
Is it possible to leave hospice care if we change our minds?
Yes, you can stop hospice care at any time if you decide to return to curative treatments or for any other reason.
As we conclude our guide, we want you to feel empowered and equipped with the knowledge and resources to confidently navigate this part of your loved one’s journey.
Hospice care is a compassionate choice that honors the dignity of those nearing the end of life. It’s a decision made from love, offering peace and comfort when needed. Remember, choosing hospice care isn’t about giving up; it’s about choosing the quality of life for the remaining time.
We’ve explored the essential aspects of hospice care, from the six-month prognosis requirement to the different levels of care available. We’ve clarified the distinctions between palliative and hospice care and outlined the steps to access the support you and your loved one need.
Medicare and other insurance plans can provide financial support for hospice care, ensuring that you focus on your loved one and not on bills and paperwork. The hospice care team is your partner, offering expertise, empathy, and emotional support.
As you move forward, take comfort in knowing you’re not alone. Many resources are available, from the hospice care team to support groups and counseling services. Don’t hesitate to ask for help or information—you deserve that support.
In the end, it’s the love and memories shared with your loved one that matter most. Hospice care helps create a space where those moments can be cherished, where every day is an opportunity to express love, share stories, and say the important things that need to be said.
Denial Reason – Six-Month Terminal Prognosis Not Supported (PDF)
How long you can get hospice care
Documentation Requirements for the Hospice Physician Certification/Recertification (PDF)
Hospice Certification / Recertification Requirements
Medicare Hospice Certification and Recertification Compliance Guide (PDF)
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying