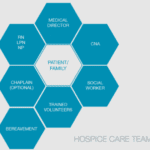
Category: Hospice Care Team
Articles about the makeup of the hospice care team such as the bereavement coordinator, CNA’s, Registered Nurses, Social Workers, Medical Directors and so on.
Articles about the makeup of the hospice care team such as the bereavement coordinator, CNA’s, Registered Nurses, Social Workers, Medical Directors and so on.

Recent University of Michigan research found that benzodiazepines and antipsychotics commonly prescribed in hospice care may significantly increase mortality risk for people with dementia. This article explores these findings and provides essential advocacy guidance for families, caregivers, and hospice professionals.

Caring for a terminally ill loved one at home is an incredibly challenging and emotional journey for family caregivers. This guide acknowledges the struggles you may face and offers compassionate solutions. It explores valuable resources, such as end-of-life doulas, PACE programs, and professional home care services, all designed to help ease your burden and provide support during this difficult time. You are not alone in this experience; there are ways to find relief and comfort as you navigate these profound challenges.

Discover the art of crafting hospice prayers that resonate with patients’ beliefs, providing comfort and solace in their final journey. Learn from hospice professionals about personalizing this sacred support.

In this article, we will explore whether medical-surgical or critical care experience is necessary to become a hospice nurse, the benefits and challenges of working in hospice care, the educational and licensure requirements for hospice nurses, and the resources and opportunities for professional development and networking in hospice nursing.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.
Hospice care is about providing compassionate support and comfort to patients during their end-of-life journey. Interdisciplinary Group (IDG) meetings ensure the highest quality care for hospice patients and their families. These meetings bring together a diverse team of professionals to discuss patient care plans, address concerns, and collaborate on providing holistic support. However, these meetings can sometimes become overwhelming and time-consuming. Let's explore some best practices to make the most of IDG meetings while keeping patient-centered care at the forefront.
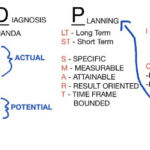
As a hospice nurse, you are vital in providing compassionate care to terminally ill patients and their families. To ensure the best possible outcomes, you rely on a systematic approach known as ADPIE: Assessment, Diagnosis, Planning, Implementation, and Evaluation. This process guides you in delivering holistic and individualized care, addressing not only the physical needs of patients but also their emotional, spiritual, and psychosocial well-being.

Discover essential time management strategies for hospice visiting nurses. Learn how to balance patient care, documentation, and self-care while navigating the unique challenges of rural hospice work. Improve your efficiency and effectiveness in providing compassionate end-of-life care.
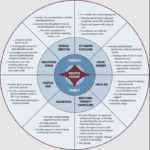
The end-of-life journey can be challenging and emotional for patients and their loved ones. A dedicated team of professionals provides comfort, support, and holistic care in hospice care. Each team member has a unique role, ensuring the patient's physical, emotional, and spiritual needs are met. Let's explore the roles of different hospice team members and how they contribute to your care journey.

As a seasoned hospice nurse, I recognize the significance of adhering to Medicare guidelines to ensure top-notch patient care. Medicare guidelines offer a roadmap for hospice providers to offer exceptional care to terminally ill patients and their loved ones. Nonetheless, upholding compliance with these guidelines can be a hurdle, especially for smaller hospice providers with limited resources. In this article, we'll delve into how RN case managers can effectively ensure compliance with Medicare guidelines.

If you or someone you love has a serious illness that cannot be cured, you may have heard of hospice care. Hospice care is a special kind that focuses on making the patient comfortable and peaceful in their final days. Hospice care also supports the family and caregivers emotionally and spiritually.
When a patient joins hospice care, they will have a special meeting with a hospice nurse. This meeting is called the post-admission visit. It is an especially important visit because it will help the patient and the family get to know the hospice team and learn more about the care they will receive.
This article will explain what to expect and what to ask during the post-admission visit. We will also provide tips and resources to help you and your loved one make the most of this time. We hope this article will help you feel more prepared and confident about the hospice journey.

Discover essential educational topics for hospice nurses during admission and follow-up visits. Learn how to effectively communicate with patients and families, manage symptoms, provide emotional support, and navigate end-of-life care. Enhance your skills to deliver compassionate, comprehensive hospice care.
As a hospice nurse, determining the appropriate frequency of scheduled nurse visits for your patients is essential to providing effective and compassionate end-of-life care. Patients and their families often rely on your expertise to ensure comfort and well-being during this sensitive time. In this article, we'll discuss suggested starting scheduled nurse visit frequencies, when to decrease or increase frequencies, and factors to consider based on patient acuity and changes in their condition.

Discover how hospice patients can safely travel and create lasting memories with loved ones. Learn about essential preparations, medical considerations, and tips for a smooth journey. Explore ways to make the most of precious moments together while ensuring comfort and care during travel.
Hospice volunteer coordinators ensure hospice patients receive the compassionate care and support they need during their end-of-life journey. In this article, we will explore the responsibilities of a hospice volunteer coordinator, address common misconceptions about hospice volunteers, and share insights from Hope Eberly, Volunteer Coordinator for Grane Hospice.

This position involves being the first point of contact for families, patients, and facilities, making a lasting impression by offering both compassion and confidence in explaining hospice services. In this discussion, we will delve into the various aspects of the role of the Hospice Liaison, bringing insight from forever Christmas-loving Kathy Naccarato, including its dynamic nature, your dedication to dispelling misconceptions, and the importance of building relationships within the healthcare community.

In this article, we will explore the vital role of a hospice chaplain, as explained by Katherine Seiler, an experienced and compassionate hospice chaplain. Hospice chaplains play a significant role in providing emotional, social, and spiritual support to terminally ill patients and their families during their end-of-life journey.

This article delves into hospice care with Andrew Viozzi, an adept hospice admission registered nurse. Andrew brings valuable insights into the hospice admission process and the broader spectrum of hospice care. Although Andrew's current position revolves around admissions, his extensive experience encompasses case management, preceptorship, mentorship, and the guidance of new hospice nurses. In this article, we dispel misconceptions, highlight the advantages of hospice care, outline the admission procedure, and emphasize the pivotal role of hospice in end-of-life care.

In the realm of hospice care, compassion and comfort take precedence. A team of skilled professionals comes together to offer comprehensive support to patients, their families, and caregivers. Among these essential contributors, Certified Nursing Assistants (CNAs) stand out as unsung heroes, bringing immeasurable value to the field of hospice care. This article delves into the distinctive role CNAs play in hospice, their frequent and meaningful interactions, and their leadership within the hospice team.

It's common in nursing to be told by others that you shouldn't be a nurse, and some may even call you a "fake nurse" if you don't meet their standards of what they think is required to be a nurse. The first time I was told I could not be a nurse was by an elderly woman who believed only women could be nurses.
This article provides valuable insights for hospice nurses on improving documentation to conquer Medicare audits and ensure claims are not denied due to insufficient evidence of terminal prognosis. The author shares real-life examples of visit narratives before and after implementing documentation best practices learned from an expert. The tips focus on capturing negative condition changes, disorientation levels, and functional decline to paint a clear picture of the patient's terminal state, ultimately leading to better patient care.

Whether you are a new hospice nurse or an experienced one like me, I would hope that it is your desire to prove and support continued hospice eligibility for your patients and families. In my years as a hospice nurse, I've always felt the training on what words and phrases to use to support hospice eligibility was weak compared to the training received in other areas of nursing. Now, you have a means of getting the education you need in a very portable setup that you can take with you, use as you see fit, and bloom!

What does a typical day, a typical week look like for a visiting hospice registered nurse case manager look like?

One crucial aspect for new hospice nurses to grasp is the Hospice Item Set (HIS) requirements. In this article, I’ll explain the HIS requirements for Medicare, providing you with a comprehensive understanding to ensure compliance and quality care delivery.