Category: Best Practice
Articles about best practices often in the field of hospice with the goal to maintain Medicare compliance.
Articles about best practices often in the field of hospice with the goal to maintain Medicare compliance.

This article discusses the importance of quarterly medication reconciliation for terminal patients and their families. It explains the benefits, such as improving patient safety, quality of life, symptom management, and the challenges and solutions. It also addresses the need to re-evaluate certain medications, like donepezil and memantine, for patients with dementia as their disease progresses.

Navigating the intricate path of hospice care involves a nuanced understanding of the unique needs of terminally ill patients. The frequency and nature of nursing visits are crucial in ensuring optimal comfort and support during the final stages of life. This article will delve into the variations in hospice nursing visits, explicitly comparing the last two weeks to the preceding six months.
Hospice care is often misunderstood. A common myth suggests that once a patient with a terminal illness enters hospice, they lose control over their care. This article aims to dispel this misconception and highlight the central role of patient and family autonomy in hospice settings. It's important to note that this discussion primarily applies to patients receiving care at home or in non-facility settings, as facility-based patients may have less control over their care decisions.
Compliance-based, Eligibility Driven Hospice Documentation: Tips for Hospice Nurses" offers comprehensive guidance for hospice professionals. This valuable resource provides practical examples for various aspects of hospice care documentation, including admissions, recertifications, IDG/IDT notes, continuous care, and GIP records. Enhance your documentation skills while ensuring regulatory compliance.

Hospice General Inpatient Care (GIP) provides short-term, intensive care for patients experiencing severe pain or symptoms that can't be managed at home. Learn about GIP eligibility, benefits, and how it helps both patients and families during challenging times. Discover key details and important considerations for this essential hospice service.

End-of-life wound care is crucial for patient comfort and dignity. This guide covers practical tips for preventing infection, managing symptoms, and supporting caregivers during this sensitive time. Learn how to make wound care a compassionate part of hospice and palliative care.

This guide covers how to write effective hospice nursing narratives, key documentation areas, and the importance of detailed and negative-based wording to support continued hospice eligibility.
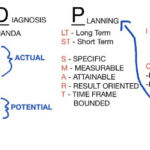
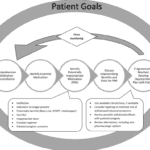
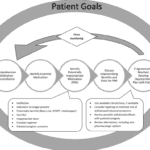
As a hospice nurse, you are vital in providing compassionate care to terminally ill patients and their families. To ensure the best possible outcomes, you rely on a systematic approach known as ADPIE: Assessment, Diagnosis, Planning, Implementation, and Evaluation. This process guides you in delivering holistic and individualized care, addressing not only the physical needs of patients but also their emotional, spiritual, and psychosocial well-being.

As a hospice admission nurse, asking the right questions is crucial for assessing patients' eligibility and providing compassionate care. This article explores critical questions to understand the patient's condition, decline timeline, hospitalizations, functional abilities, cognitive status, and comorbidities. By gathering this information, nurses can support informed decisions, tailor interventions, and ensure a "good death" for patients and families.
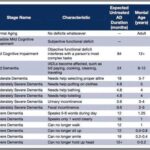
As a nurse who has cared for many terminally ill individuals with Alzheimer's disease over the years, I understand the importance of accurately assessing their functional decline using the Functional Assessment Staging Tool (FAST). The FAST scale provides valuable information about the progression of Alzheimer's disease and helps guide appropriate care planning for patients and their families. In this guide, I will walk you through the process of assessing patients on the FAST scale, starting from stage 1 and discussing when to stop reading the scale for determination. I will also provide three examples of patients at various stages of the FAST scale.

Discover essential time management strategies for hospice visiting nurses. Learn how to balance patient care, documentation, and self-care while navigating the unique challenges of rural hospice work. Improve your efficiency and effectiveness in providing compassionate end-of-life care.
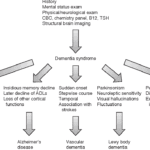
Exploring Hospice Eligibility Criteria for Alzheimer's, Vascular, Lewy Body, Frontotemporal and other Dementias: Empowering Hospice Nurses to Provide Compassionate End-of-Life Care
Uncover the importance of regular care plan meetings at healthcare facilities. This guide details participants, goals, benefits, and risks of non-participation.

As a seasoned hospice nurse, I recognize the significance of adhering to Medicare guidelines to ensure top-notch patient care. Medicare guidelines offer a roadmap for hospice providers to offer exceptional care to terminally ill patients and their loved ones. Nonetheless, upholding compliance with these guidelines can be a hurdle, especially for smaller hospice providers with limited resources. In this article, we'll delve into how RN case managers can effectively ensure compliance with Medicare guidelines.

Discover essential educational topics for hospice nurses during admission and follow-up visits. Learn how to effectively communicate with patients and families, manage symptoms, provide emotional support, and navigate end-of-life care. Enhance your skills to deliver compassionate, comprehensive hospice care.

Discover the potential side effects of dementia medications and how to support your loved one. Stay informed!
In the world of healthcare, when a provider writes an order to "Eval and Treat" for hospice, they are asking for a thorough evaluation and a tailored treatment plan. This is specifically meant for patients who are being considered for hospice care. Let's delve into what this means and why it's crucial.
What Does "Eval and Treat" for Hospice Mean?
As a hospice nurse, determining the appropriate frequency of scheduled nurse visits for your patients is essential to providing effective and compassionate end-of-life care. Patients and their families often rely on your expertise to ensure comfort and well-being during this sensitive time. In this article, we'll discuss suggested starting scheduled nurse visit frequencies, when to decrease or increase frequencies, and factors to consider based on patient acuity and changes in their condition.
In this article, we will discuss how to use the Beers Criteria to identify PIMs and potential prescribing omissions (PPOs) in hospice patients. PPOs are medications that are indicated but not prescribed for a specific patient or population, or that are prescribed at a suboptimal dose or duration. We will also present 10 case studies to illustrate the medication reconciliation and deprescribing process and the outcomes of medication changes in different scenarios.
Caring for a comatose loved one during their hospice journey requires special attention, particularly when it comes to oral care. In this guide, we'll explore best practices for oral care, considering the unique needs of comatose patients, and provide you with valuable resources for further guidance.

Navigating hospice eligibility for non-Alzheimer's dementia patients demands a personalized approach. Unlike Alzheimer's, there's no definitive scale, necessitating assessments of functional decline, mobility, communication, incontinence, weight loss, overall condition, and comorbidities. Effective documentation, clinical judgment, and compassionate care are crucial for supporting these patients and families.
Navigating the tender journey of hospice care, Compassion Crossing offers guidance on addressing the pivotal question of “when?”—a beacon for caregivers seeking solace and understanding in life’s final chapter.
If you are caring for a terminally ill patient in hospice, you know how challenging it can be to manage their medications. You want to make sure they are getting the best possible care, but you also want to avoid unnecessary or harmful drugs that may worsen their quality of life or cause adverse effects.
That’s where medication reconciliation and deprescribing come in. Medication reconciliation is the process of reviewing and updating the patient’s medication list to ensure accuracy and completeness. Deprescribing is the process of reducing or stopping medications that are no longer needed, effective, or appropriate for the patient’s condition and goals of care.
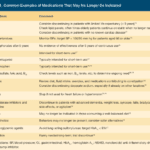
I know how important it is to provide comfort and support during this challenging journey. One aspect of hospice care that often raises concerns is deprescribing medications. In this article, we'll explore what deprescribing is and why it can benefit patients nearing the end of life.