Category: Dying Process
Articles on the dying process covering the transitioning stage and the active stage of dying including the last hours of life.
Articles on the dying process covering the transitioning stage and the active stage of dying including the last hours of life.

Navigating the complexities of end-of-life care can be challenging. This article delves into the nuances of terminal agitation and terminal restlessness, providing caregivers and family members with the essential knowledge to better understand and support their loved ones during the final stages of life.
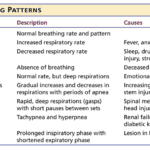
Understanding breathing patterns in end-of-life care is crucial for providing comfort to your loved one. Learn about regular vs. irregular breathing rhythms and when to contact hospice for additional support.

Explore the complex decision of using antibiotics in end-of-life care. This article weighs the potential benefits against risks, considering comfort, quality of life, and ethical concerns. Learn how to make informed choices with your healthcare team for compassionate, patient-centered care in life's final stages.

Hospice nurses are crucial in comforting and supporting patients nearing death and their families. This article explores what to expect from hospice care, focusing on patient assessments, educational discussions, and addressing common family concerns.

Kennedy ulcers are skin lesions that can develop in individuals nearing the end of life. This guide explores their appearance, causes, diagnosis, and treatment. It offers insights into identifying Kennedy ulcers and providing comfort through pain relief, hygiene, and repositioning. Additionally, it addresses the emotional impact and coping strategies for caregivers and loved ones.

The journey towards the end of life can be a challenging and emotional time, both for the individual facing the end of their life and for their caregivers and family members. One aspect of this journey that may be unfamiliar to many is the presence of self-soothing sounds made by the patient during the transition and actively dying phase. These sounds can be puzzling and sometimes unsettling for caregivers and family members who have never witnessed them. This article will explore self-soothing sounds, why they occur, and how caregivers and family members can distinguish between self-soothing sounds and signs of discomfort.

Caring for a terminally ill loved one can be challenging and emotional. As an experienced hospice nurse case manager, you understand the importance of providing compassionate care and support to loved ones and their families. In this educational article, we will explore the common journey that terminally ill loved ones and their caregivers face as they approach the end of life. We will summarize this journey's various aspects, offering guidance and separating fact from fiction.

Explore the profound journey of the actively dying. This article unravels the reasons behind their lingering, examining medical interventions and the emotional need for closure. Gain insight into this delicate phase of life."
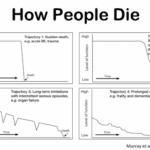
Explore the journey through terminal illness, understanding key signs and symptoms at each stage. This guide offers insight into the physical and emotional changes as life nears its end, helping caregivers provide compassionate support.
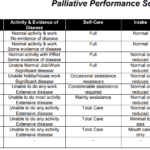
Explore the Palliative Performance Scale (PPS) and its crucial role in end-of-life care. Learn how this tool helps hospice professionals assess patient decline, predict life expectancy, and provide tailored care. Understand the significance of PPS changes in the final six months and how they guide compassionate care decisions.

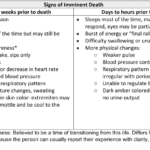
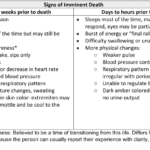
As a caregiver or family member, witnessing the final hour of a loved one's life can be a challenging and emotional experience. It's essential to be prepared and understand what to expect. While each person's journey is unique, some common physical changes may occur in the last hour of life. Here's a guide to help you navigate this sensitive time:
Recognizing end-of-life signs can be challenging. This guide outlines key symptoms indicating a terminally ill patient may have less than two weeks, offering crucial insights for caregivers and families.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.

Witnessing a loved one nearing the end of life can be challenging and emotional for a caregiver. One symptom you may encounter during this time is the death rattle. Understanding what the death rattle is, how to recognize it, and how to manage its symptoms can help you provide comfort and support to your loved one in their final days. This guide will explore the death rattle, its significance, and practical tips for managing it.

As a caregiver or family member, it can be challenging to witness the changes that occur as a loved one approaches the end of their life. One such change that may occur is mottled skin, also known as livedo reticularis. Understanding what mottled skin is and its significance in the dying process can help you provide the best care and support to your loved one during this time.
Explore the journey of functional decline in the natural dying process. This article provides insight for caregivers and families, emphasizing the importance of documenting changes to enhance care and decision-making in life’s final chapter.
Discover key indicators for end-of-life care in hospice. This guide highlights ‘trigger words’ that signal a patient’s final days, aiding nurses and caregivers in providing compassionate support during the most critical moments.
I understand how challenging it can be for terminally ill patients to cope with their fear of impending death. It is crucial for both healthcare providers and family members to take these feelings seriously and respond with compassion and understanding. In this article, we will explore the importance of acknowledging a patient's fear of impending doom and discuss actions that families can take to provide peace and comfort during this grim time.
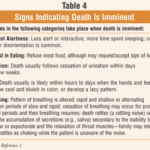
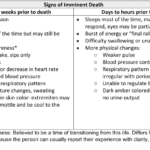
For a non-healthcare professional who has never witnessed death before, it can be unsettling to be present with someone who is nearing the end of their life. However, there are certain signs and observations that you can make using your senses that may indicate that the person you are with may pass away within seconds, minutes, or hours. Understanding these signs can help you provide support and comfort to the individual and their loved ones during this grim time.
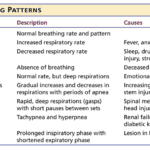
Understanding the final breath: This article explores the critical breathing patterns observed in the last hours of life, offering insights for caregivers and family members to prepare for the end-of-life journey.
Losing a loved one is an incredibly challenging and emotional experience. If you find yourself in the presence of someone in the transitioning phase of the dying process, knowing what signs to look for can be helpful. Although every individual's experience may vary, some common observations may indicate someone is in the transitioning phase. Here's a guide to help you recognize these signs and provide support during this grim time.
Dying doesn’t always hurt. The amount and type of pain there is at the end of life can differ. The specific diagnosis and cause of pain are factors.

One of the hardest portions of the job of a hospice nurse is to identify when a patient has two weeks of life left to live; this can be especially difficult at facilities going through staffing shortages leading to inconsistent caregivers with little to verbally report on a patient’s change of condition. Since being aware of the velocity of declines is extremely important, let’s cover an area that we in hospice (nurses, families, and caregivers alike) can keep an eye on in terms of identifying terminal restlessness which is often a key indicator for one week or less of life.

There is a spiritual connection in hospice, dealing with death and dying forty-plus hours per week. We who are in the field see it often, but there are times when we hear it firmly from the patients and families whom we serve. Let me share the most recent event on Memorial Day, 5/29/2023, week.