When Family Goes Silent: Finding Help When Loved Ones Won’t Step Up
Published on August 25, 2025
Updated on November 7, 2025
Published on August 25, 2025
Updated on November 7, 2025
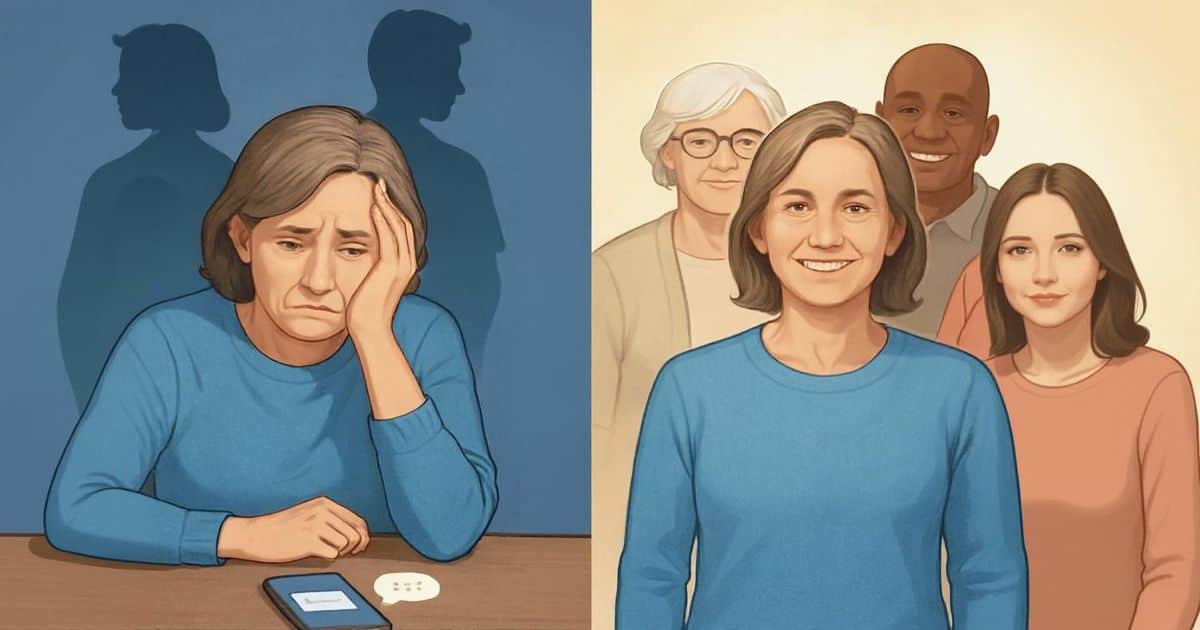
Table of Contents
You’re not alone in feeling abandoned. As you read this, thousands of family caregivers across the country are asking themselves the same heartbreaking question: “Where is everyone?”
Maybe it started slowly. Your siblings stopped returning calls about Mom’s doctor appointments. Your adult children became “too busy” to help with Dad’s medications. Perhaps family members who once promised to help have simply disappeared, leaving you to carry the weight of caregiving completely on your own.
This experience is far more common than you might think. Research shows that in most families facing serious illness, one person ends up shouldering 80% or more of the caregiving responsibilities. The National Alliance for Caregiving found that nearly 7 out of 10 family caregivers report feeling isolated and unsupported by other family members.
You may be experiencing what experts call “caregiver isolation” – a situation where the primary caregiver becomes increasingly cut off from family support, social connections, and sometimes their own needs. This isn’t just about feeling lonely. It’s about carrying an enormous emotional, physical, and financial burden while watching people you expected to help simply walk away.
Your feelings about this situation are entirely valid. Whether you feel angry, hurt, exhausted, or all of these emotions at once, know that these reactions make perfect sense. It’s natural to feel abandoned when family members who should be helping instead choose to stay silent or distant.
The silence from family members often becomes louder than words. Phone calls go unreturned. Text messages about your loved one’s condition get ignored. Family members might even avoid visiting altogether, leaving you to wonder if you’ve done something wrong or if they simply don’t care.
But here’s what’s important to understand: their absence says nothing about your worth as a caregiver or family member. Sometimes family members pull away because they don’t know how to help, feel overwhelmed by the situation, or are dealing with their own fears about illness and death. While this doesn’t excuse their behavior, understanding it can help you find ways to move forward.
You deserve support. You deserve help. And most importantly, you deserve to know that there are practical steps you can take to either reconnect with silent family members or build a strong support network that doesn’t depend on them.
This situation may feel hopeless right now, but you have more options than you realize. We will explore compassionate ways to reach out to distant family members, how to build support systems beyond your immediate family, and most importantly, how to take care of yourself during this challenging time.
Remember: being the only one who stepped up doesn’t make you the only one who matters. Your dedication to your loved one is remarkable, and with the right approach and support, you don’t have to carry this burden alone.
When you’re caring for a terminally ill loved one and other family members have stepped back, you might feel like you’re drowning in emotions. These feelings are completely normal and valid. You’re not being dramatic, weak, or selfish. You’re human, dealing with a challenging situation that would challenge anyone.
Anger is one of the most natural responses when family members disappear during a crisis. You might feel furious that siblings who used to call every week suddenly seem too busy to help. You might be angry that cousins who always showed up for holidays now make excuses when you ask for support.
This anger makes perfect sense. You’re watching someone you love suffer while carrying the entire burden yourself. Your anger doesn’t make you a bad person – it makes you human.
Common thoughts you might have:
These thoughts are entirely understandable. When people we expect to support us let us down during our darkest moments, anger is a natural protective response. Don’t judge yourself for feeling this way.
Caring for someone with a terminal illness is physically and emotionally draining. When you’re doing it alone, the exhaustion becomes overwhelming. You might feel tired in your bones, like you can’t catch your breath or find a moment of peace.
This exhaustion isn’t just about being sleepy. It’s about:
You’re not weak because you’re tired. You’re carrying a load that was meant to be shared. Your exhaustion is your body and mind telling you that you need and deserve support.
Feeling disappointed in family members who aren’t helping is completely normal. You probably had expectations about how people would show up during this difficult time. When those expectations aren’t met, disappointment naturally follows.
You might be disappointed because:
This disappointment doesn’t mean you had unrealistic expectations. It means you believed in the power of family bonds and mutual support. Those are beautiful values, even when others don’t share them.
Your disappointment might feel especially sharp because you’re grieving multiple losses at once – the approaching loss of your loved one and the loss of relationships you thought you could count on.
No one expects to become the sole caregiver for a terminally ill family member. When someone receives a life-limiting diagnosis, most people assume the family will rally together. You probably imagined that others would naturally step forward to help.
The reality is often very different, and that’s not your fault.
| What You Expected | What Often Happens |
|---|---|
| Family members taking turns with care | One person (often you) becomes the primary caregiver |
| Shared emotional support | Feeling isolated in your grief and stress |
| Help with practical tasks | Managing everything from medications to insurance alone |
| Regular check-ins from relatives | Radio silence or surface-level contact |
| Financial contribution for care costs | Bearing all expenses yourself |
You took on this role because you love your family member, not because you were obligated to do it alone. The fact that others aren’t participating doesn’t diminish your choice to care – it highlights your compassion and commitment.
All of your emotions – anger, exhaustion, disappointment, sadness, fear – are valid responses to an incredibly challenging situation. Validation therapy teaches us that feelings don’t need to be fixed or changed; they need to be acknowledged and accepted.
Here’s what validating your own feelings looks like:
You can feel grateful for the opportunity to care for someone you love AND feel angry that you’re doing it alone. These emotions can exist together. You can treasure moments with your loved one AND feel overwhelmed by the responsibility. Both feelings are true and valid.
Recognizing that your feelings are valid is the first step toward finding the help and support you need. When you stop judging yourself for being angry or disappointed, you can use that energy to solve the practical problems you’re facing.
Your emotions are messengers. They’re telling you that:
Listening to these messages doesn’t make you selfish – it makes you wise. By acknowledging what you’re feeling and what you need, you’re taking the first step toward creating a more sustainable caregiving situation and finding the support you deserve.
Remember: You are doing an incredible job under impossible circumstances. Your feelings are valid, your needs are important, and you deserve help and support during this difficult journey.
When you’re caring for someone you love who is seriously ill, it can feel heartbreaking when other family members seem to disappear. You might wonder why your siblings stopped calling, why your adult children make excuses to avoid visits, or why your spouse’s relatives suddenly became “too busy” to help.
The truth is, when people step back during a health crisis, it’s rarely about not caring. Most often, it’s about not knowing how to cope with their own intense emotions. Understanding the real reasons behind their silence can help you respond with compassion instead of anger, and it might even help you find ways to reconnect with them.
Let’s explore the most common reasons why people withdraw when someone they love is facing a serious illness.
Fear is one of the strongest emotions that drives people away during a health crisis. Your family members might be terrified of seeing their loved one suffer, scared of saying the wrong thing, or frightened by their own mortality. When someone we care about becomes seriously ill, it forces us to face the reality that life is fragile and unpredictable.
Many people feel completely helpless when they don’t know how to “fix” the situation. They might think, “What’s the point of visiting if I can’t make them better?” This helplessness can feel so overwhelming that staying away seems easier than facing it.
Your family members might also be afraid of their own emotional reactions. They worry they’ll break down crying, say something hurtful, or make the situation worse. Some people have never learned healthy ways to express difficult emotions, so they choose avoidance instead.
What you can do:
Modern life already feels overwhelming for many people, and a family health crisis can feel like the final straw. Your family members might be juggling demanding jobs, their own health problems, financial stress, or challenges with their children. Adding caregiving responsibilities or emotional support can feel impossible.
Many people also don’t know what’s expected of them or how to help appropriately. They might think, “I don’t want to get in the way” or “The main caregiver seems to have everything handled.” Without clear guidance about how they can contribute, they might choose to stay on the sidelines.
The uncertainty of the situation makes everything harder. When someone is seriously ill, family members often don’t know what to prepare for, how long the situation might last, or what role they should play. This uncertainty can create paralysis rather than action.
| Signs of Overwhelm | What It Might Look Like |
|---|---|
| Communication changes | Shorter phone calls, delayed responses to texts |
| Excuse-making | “I’m too busy,” “I have my own problems” |
| Emotional shutdown | Seeming distant or detached during conversations |
| Avoidance behaviors | Missing family gatherings, declining invitations |
What you can do:
Some family members might be dealing with their own mental health struggles that make it especially hard to be present during a crisis. Depression can make everything feel impossible, including showing up for others. Anxiety can make the uncertainty of illness feel unbearable.
Past traumatic experiences can also play a huge role. If a family member has lost someone important to them, your loved one’s illness might trigger painful memories and emotions. They might be reliving their own grief or trauma every time they think about the current situation.
Some people develop what looks like PTSD symptoms when faced with a loved one’s serious illness. They might experience intrusive thoughts, nightmares, or panic attacks that make it feel unsafe to engage with the situation. This isn’t weakness – it’s a normal response to overwhelming stress.
Previous experiences with hospitals, medical procedures, or caring for sick relatives can create lasting emotional wounds. Someone who watched a parent suffer through a difficult illness might find it impossible to face that situation again, even when it involves someone else they love.
What you can do:
Grief doesn’t just happen after someone dies – it starts the moment we realize we’re losing someone we love. Your family members might be experiencing what’s called anticipatory grief, mourning the loss of the person they knew before the illness and the future they thought they’d have together.
Some people cope with grief by avoiding the source of their pain. If seeing your loved one in their current condition is too painful, family members might choose to remember them as they were rather than face the reality of how they are now. This avoidance might seem selfish, but it’s often a desperate attempt to protect themselves from unbearable emotional pain.
Grief can also make people feel guilty about continuing with their normal lives. They might think, “How can I enjoy my dinner when my loved one is suffering?” or “It feels wrong to laugh when someone I care about is dying.” This guilt can make them withdraw from everyone, including you and the person who is ill.
Different people grieve in different ways. While some might find comfort in staying close and being involved in care, others might need distance to process their emotions. Neither way is right or wrong—they’re just different coping styles.
| Types of Anticipatory Grief | How It Might Show Up |
|---|---|
| Identity grief | “They’re not the same person anymore” |
| Relationship grief | Mourning the loss of shared activities or conversations |
| Future grief | Sadness about plans that won’t happen |
| Role grief | Missing how the person used to function in the family |
What you can do:
When you understand why people step back, it doesn’t necessarily make it hurt less, but it can help you respond with compassion instead of anger. Remember that everyone processes difficult emotions differently; what works for you might not work for others.
The goal isn’t to force people to participate in ways that feel wrong to them. Instead, try to find small ways they can stay connected that feel manageable for their emotional state and life circumstances. Sometimes just knowing they care can provide comfort during difficult times, even from a distance.
Your role as the primary caregiver is demanding enough without the additional burden of resentment toward family members who have stepped back. By understanding their silence with compassion, you free yourself to focus your energy where it matters most—on caring for your loved one and taking care of yourself.
When your family members stay silent or pull away during your loved one’s illness, it hurts deeply. You’re carrying a heavy load alone, wondering why others who claim to care won’t step up to help. This silence doesn’t necessarily mean they don’t care – it often means they’re scared, overwhelmed, or simply don’t know how to help.
Using principles from validation therapy, we can approach resistant family members with empathy while clearly expressing our needs. Here are five proven strategies to bridge that gap and get the support you deserve.
Why “I” statements work better than accusations
When we’re exhausted and frustrated, it’s natural to want to say things like “You never help” or “You don’t care about Mom.” But these statements make people defensive and more likely to shut down completely.
“I” statements focus on your feelings and needs rather than blaming others. This approach validates your own experience while creating space for others to respond with compassion instead of defensiveness.
Examples of effective “I” statements:
Instead of saying “You never visit Dad,” try:
Instead of “You don’t understand how hard this is,” say:
Instead of “You’re being selfish,” try:
Making your “I” statements more effective:
Why vague requests don’t work
When you say “I need help with Mom,” family members often don’t know what that means. They might worry you’re asking them to become a full-time caregiver like you. This uncertainty makes it easier for them to avoid responding altogether.
The power of specific, manageable requests
People are much more likely to say yes to clear, limited tasks that fit into their existing lives. When you make specific requests, you remove the guesswork and make it easier for them to help.
Examples of specific, time-limited requests:
| Instead of This | Try This Specific Request |
|---|---|
| “I need help with Dad” | “Could you sit with Dad next Tuesday from 2-4 pm so I can go to my doctor’s appointment?” |
| “Someone needs to help more” | “Would you be willing to pick up Dad’s prescriptions once a month? I could text you when they’re ready.” |
| “I can’t do this alone” | “Could you call Mom every Sunday evening for 15 minutes? It would give me a break and she’d love to hear from you.” |
| “We need to talk about Mom’s care” | “Can we have a 30-minute phone call this Saturday to discuss Mom’s medication schedule and how we might divide some tasks?” |
Making specific requests more successful:
Understanding why people pull away
Family members often stay silent because they’re dealing with their own fears about illness, death, or inadequacy. They might worry about:
Using validation to address fears
Validation therapy teaches us that acknowledging someone’s fears and concerns creates safety for honest conversation. When you validate their worries, you make it easier for them to open up and potentially help.
How to validate and address common fears:
Fear: “I don’t know what to do if something happens”
Your response: “I understand that worry – I felt the same way at first. What if we start with something simple, like bringing groceries once a week? You wouldn’t need to handle any medical situations.”
Fear: “I can’t handle seeing them so sick”
Your response: “It’s tough to watch someone you love go through this. Would it help to talk on the phone with them instead of visiting? Or maybe you could help with tasks that don’t require being here?”
Fear: “I have my own family responsibilities”
Your response: “I completely understand that you have a lot on your plate. Even small things would help – like a weekly phone call or picking up one prescription when you’re already out running errands.”
Creating conversations that reduce fear:
Why family meetings work for resistant relatives
Sometimes family members stay away because they don’t have complete information about what’s happening. They might think you have everything under control or don’t realize how much help is actually needed. A family meeting creates transparency and shared responsibility.
Setting up successful family meetings:
For in-person or video meetings:
For group chats or emails:
Sample family meeting agenda:
| Topic | Time | Purpose |
|---|---|---|
| Current situation update | 10 minutes | Everyone gets the same information |
| Immediate needs | 10 minutes | Identify where help is most needed |
| How everyone can contribute | 15 minutes | Match tasks to people’s abilities |
| Questions and concerns | 10 minutes | Address fears and misunderstandings |
Making family communication more effective:
Why understanding changes everything
Many family members pull away simply because they don’t understand what’s happening to your loved one. When people don’t know what to expect or how to help, they often choose to stay away rather than risk doing something wrong.
Choosing the right educational resources:
The key is sharing information that helps family members understand both the medical situation and practical ways they can help. Look for resources that:
Effective ways to share information:
Email or text with helpful articles:
“I found this article really helpful in understanding Dad’s condition. It explains what we’re dealing with and has some good suggestions for ways family can help. I’d love to hear your thoughts after you read it.”
Share specific sections of longer resources:
Instead of sending a 20-page booklet, highlight the most relevant sections and explain why you’re sharing them.
Use the information to start conversations:
“I learned that people with Mom’s condition often have good days and bad days. On her good days, she’d really love phone calls from family. Would you be interested in calling her once a week?”
Resources to consider sharing:
Making educational sharing more successful:
Remember: Small steps create big changes
These five strategies work best when used consistently over time rather than trying them once and giving up. People need time to process their fears and figure out how they can help. Your patient, persistent outreach—combined with clear communication about your needs—often opens doors that seemed permanently closed.
The most important thing to remember is that your need for support is valid and reasonable. You’re not asking too much when you reach out for help caring for someone you all love. Sometimes, family members just need guidance on how to step up, and these strategies can provide that bridge.
When family members go silent or refuse to help with caregiving, you might feel abandoned and overwhelmed. You don’t have to carry this burden alone. There are professional services designed specifically for situations like yours that can provide both practical support and help bridge family gaps.
PACE is like having a whole care team in your corner. This special program brings together doctors, nurses, therapists, and social workers under one roof to care for people who qualify for nursing home care but want to stay at home.
PACE provides comprehensive care that goes far beyond what most insurance covers:
Medical and Health Services:
Daily Living Support:
Family Support:
| Traditional Home Care | PACE Program |
|---|---|
| Limited hours of help | Comprehensive daily support |
| Multiple providers to coordinate | One team manages everything |
| Insurance may not cover all needs | All covered services included |
| Family handles medical appointments | Transportation and coordination provided |
PACE serves people who meet specific criteria:
The program is specifically designed for people with limited or unavailable family support. Your situation of having unresponsive family members actually makes you a good candidate for PACE services.
Getting started with PACE involves these steps:
Initial Contact:
Assessment Process:
Enrollment:
The assessment team understands family dynamics. When you explain that family members aren’t available to help, they’ll design your care plan accordingly.
End-of-life doulas are trained companions who support families through serious illness – not just during dying. Many people think doulas only help during the final stages, but they actually provide ongoing support throughout chronic illnesses and can help heal family relationships.
End-of-life doulas understand that serious illness affects the whole family system, not just the person who is sick. They provide support that addresses both practical needs and emotional concerns.
Emotional and Practical Support:
Communication Assistance:
Using validation therapy principles, doulas help you:
Doulas are skilled at understanding family dynamics and can sometimes help rebuild connections with distant or resistant family members.
Bridge-Building Approach:
When Bridge-Building Isn’t Possible:
Sometimes family members simply won’t engage, and a doula helps you accept this reality without taking it personally. They support you in:
End-of-life doulas provide hands-on help that fills gaps left by absent family members:
| Practical Support | Emotional Support |
|---|---|
| Accompany to medical appointments | Listen without judgment |
| Help organize medications | Validate your feelings |
| Assist with care planning | Help process anticipatory grief |
| Coordinate with healthcare teams | Support difficult decisions |
| Provide respite care | Teach stress management |
Ongoing Relationship: Unlike other professional services, doulas often work with families for months or even years. This consistency is especially valuable when family support is unreliable. Your doula becomes familiar with your situation and can provide personalized support that adapts as needs change.
Finding and Working with a Doula:
Remember that seeking professional support isn’t giving up on family – it’s taking care of yourself and your loved one. Both PACE and end-of-life doulas understand that families don’t always function the way we hope they will. They’re trained to work with the reality of your situation, not judge it.
These services can provide the comprehensive support you need while potentially creating space for family relationships to heal naturally over time. You deserve support and assistance during this challenging journey, regardless of whether family members choose to participate.
When family members step back or go silent during your loved one’s illness, the weight of caregiving can feel overwhelming. You are not alone, and you have more options than you might realize. Let’s explore how to build a strong support network that goes beyond family members who may not be available to help.
Your support network doesn’t have to be limited to blood relatives. Many caregivers find that their strongest allies come from unexpected places. Feeling disappointed when family doesn’t step up is normal, but this doesn’t mean you’re out of options.
Close friends often become chosen family during difficult times. That neighbor who always asks how you’re doing, the friend from work who offers to bring dinner, or the person from your faith community who calls to check in – these people can become invaluable parts of your support team.
Community resources are designed specifically for situations like yours. Many organizations understand that family support isn’t always available and have programs to fill these gaps:
Professional services exist to supplement family care. When family members aren’t available, professional support becomes even more critical. These services are designed to work with families of all sizes and dynamics.
Hiring professional help is not giving up – it’s being smart about caregiving. Many caregivers feel guilty about seeking paid support, especially when they believe family “should” be helping. Your loved one deserves good care, and you deserve support, regardless of where it comes from.
Professional caregivers bring specialized skills that even willing family members might not have. They understand medical needs, safety concerns, and comfort techniques that can improve your loved one’s quality of life.
| Type of Professional Support | What They Provide | When to Consider |
|---|---|---|
| Home Health Aides | Personal care, meal prep, light housekeeping | When daily tasks become overwhelming |
| Respite Care Workers | Temporary relief so you can rest or handle other needs | When you need breaks to prevent burnout |
| Hospice Teams | Medical care, emotional support, equipment, and supplies | When focused on comfort rather than cure |
| Adult Day Programs | Supervised activities and care during daytime hours | When you need to work or have appointments |
Professional support creates consistency that family members might not be able to provide. Paid caregivers show up reliably, follow care plans, and maintain professional boundaries that can actually reduce family stress.
Financial assistance programs exist to help make professional care more affordable. Don’t assume you can’t afford help without exploring options like:
Working with professionals doesn’t replace your role – it enhances it. You remain the primary advocate and decision-maker while gaining partners to provide care.
Self-care isn’t selfish when you’re the primary caregiver. This is especially true when family support is limited. Taking care of yourself is taking care of your loved one because your well-being directly affects the quality of care you can provide.
Caregiver burnout is real and serious. When you’re handling everything alone, the risk increases significantly. Watch for these warning signs:
Small acts of self-care make a big difference. You don’t need hours of free time to take care of yourself:
Professional support makes self-care possible. When you have reliable help, you can:
Your emotional needs matter too. Caregiving while dealing with absent family members creates complex feelings. It’s normal to feel angry, sad, or abandoned. Consider:
Creating boundaries protects everyone. When family members aren’t helping, you might feel pressure to do everything perfectly. You don’t have to be superhuman. Set realistic expectations for yourself and communicate your limits clearly to others.
| Self-Care Area | Quick Options | Longer-Term Solutions |
|---|---|---|
| Physical Health | Take vitamins, stretch, and drink water | Schedule regular check-ups, and exercise routine |
| Emotional Well-being | Call a friend, listen to music | Join a support group, consider counseling |
| Mental Stimulation | Read a magazine, do a puzzle | Take an online class, learn a new skill |
| Social Connection | Text with friends, video chat | Regular coffee dates, community activities |
Remember that asking for help shows strength, not weakness. Professional caregivers, community volunteers, and support services exist because caregiving is challenging work that no one should handle completely alone.
Your loved one benefits when you have support. They can see when you’re struggling, and your stress affects their comfort. When you have help and feel supported, you can be more present and patient during your time together.
Building a support network takes time, but it’s worth the effort. Start with one small step – maybe calling a local agency for information or accepting one offer of help. Each connection you make creates a stronger foundation for the challenging road ahead.
You are doing important, difficult work. The fact that some family members aren’t participating doesn’t diminish your efforts or your loved one’s worth. By seeking support beyond family, you’re ensuring the best possible care while protecting your own well-being. That’s exactly what a good caregiver does.
When family members go silent or step back during your loved one’s final journey, it can feel like you’re carrying the world alone. But here’s what you need to know: you are not alone and are enough.
Even when your family disappoints you, a whole community of people understands exactly what you’re going through. Professional caregivers, support groups, hospice teams, and other family caregivers are ready to help. These people have walked this path before and know how hard it can be when family doesn’t show up the way you hoped they would.
You don’t have to figure everything out by yourself. There are people who can teach you comfort techniques, help you understand what’s happening with your loved one, and give you breaks when you need them. Asking for help isn’t giving up – it’s being smart about caring for both yourself and your loved one.
When siblings don’t visit, when adult children make excuses, or when extended family suddenly becomes busy with other things, it’s easy to wonder if you’re doing something wrong. You’re not.
Other people’s choices to step back say nothing about you and everything about their own fears, grief, or limitations. Some people handle serious illness by avoiding it. Others feel so helpless that they withdraw completely. Their silence doesn’t mean your care isn’t valuable or that you’re not doing enough.
You are showing up with love and courage every single day. That makes you remarkable, not inadequate.
If you’ve been waiting for family to step up, it might be time to look beyond your family circle. You deserve support, and it’s available when you’re ready to accept it.
Start with one small step:
You don’t have to wait until you’re completely overwhelmed. Getting help now means you can provide better care while taking better care of yourself.
Remember: asking for support shows wisdom, not weakness. Your loved one needs you healthy and present more than they need you to be perfect or to do everything alone.
You’ve already proven your love through your dedication. Now prove your wisdom by reaching out for the help you deserve. There are people waiting to support you – you just have to let them.
Empowering Caregivers: Effective Communication with Healthcare Providers (the concepts can be applied to most situations where another person isn’t listening)
The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma
Crucial End-of-Life Conversations: A Compassionate Guide for End-of-Life Professionals
End-of-Life Doula Care Planning: A Complete Guide to Compassionate Care
Validation and Compassion: A Guide to Connecting with Terminally Ill Loved Ones
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care (the principles apply to more than end-of-life)
PTSD and Its Impact on Family Caregivers
When Love is Not Enough: Addressing the Hidden Crisis of Hospice Family Caregivers
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.