Understanding Risk Reduction in Terminal Illness
Published on January 22, 2025
Updated on January 18, 2025
Published on January 22, 2025
Updated on January 18, 2025
Table of Contents
When a loved one is facing a terminal illness, every decision about their care feels significant. It’s natural to want to do everything possible to help them. One way to make informed decisions is to understand risk reduction, which involves knowing the chances that a treatment will be beneficial or harmful.
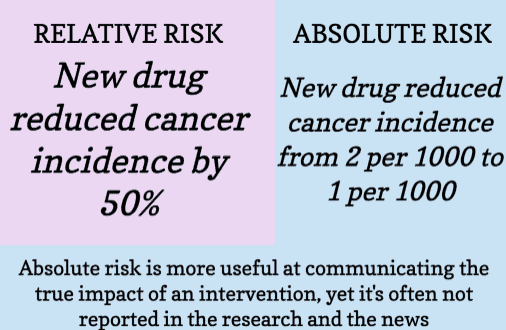
Absolute risk reduction is a straightforward measure that tells us about the actual decrease in risk due to treatment. It’s the difference in the event rate between two groups: one that gets the treatment and one that doesn’t. This number is crucial because it clearly shows the treatment’s effectiveness.
Relative risk reduction is a bit trickier. It’s the percentage decrease in risk when comparing the treatment group to the control group. While it can seem impressive, it doesn’t tell the whole story. It’s essential to look at the absolute numbers to understand the true benefit of a treatment.
By focusing on absolute risk reduction, you can better understand the potential impact of treatment on your loved one’s health and, in collaboration with their healthcare team, make more informed decisions.
Understanding the effects of treatments can be a beacon of hope when a family member is facing a terminal illness. Absolute Risk Reduction (ARR) is one such concept that can illuminate the path ahead.
Absolute Risk Reduction (ARR) tells us how much a treatment can decrease the chance of a specific health event. It’s like looking at a before-and-after picture: before the treatment, the risk might be higher, and after, we hope it’s lower. In medical terms, ARR is the difference in risk between those who received the treatment and those who didn’t.
Knowing the ARR helps doctors and families decide if a treatment is worth it. A medicine with a high ARR could make a significant difference for your loved one. But if the ARR is low, it might not be as helpful as we’d like. This number helps us weigh the benefits against the side effects or burdens of the treatment.
Let’s talk about real people, not just numbers. Imagine a medication that helps prevent heart problems. If one hundred people take it with an ARR of 2%, two out of those one hundred might avoid a heart issue because of the medicine. That’s two families who get more time with their loved ones. That’s why ARR matters—it’s about the actual impact on lives, not just statistics.
In the journey of terminal illness, ARR is a compass that can help guide your decisions. It’s a piece of the puzzle that, along with love and care, can help you and your healthcare team choose the best path for your loved one.
When we care for someone with a terminal illness, we often hear about treatments and how they can reduce risks. Relative Risk Reduction (RRR) can sound complicated, but it’s essential to understand as it can influence treatment decisions.
Relative Risk Reduction tells us how much treatment can lower the risk of a health event compared to not getting the treatment in percentage terms. It’s like comparing two pictures: one with the treatment and one without. The difference in what can happen in these two scenarios is what RRR is all about.
For example, if a new drug reduces the risk of a heart attack from 4% to 2%, the RRR is 50%. That sounds huge, right? But remember, this doesn’t tell us the actual risk—just how much it’s reduced compared to the original risk.
In terminal illness, RRR can help us think about treatments differently. It’s not just about how significant the percentage is but what it means for our loved one’s life. A high RRR might make treatment seem better than it is, so it’s also essential to know the actual risk, or the Absolute Risk Reduction, to make the best choice.
Let’s look at some real-life examples. Imagine a medicine with a high RRR—it seems it could make a big difference. But when we look closer, we see that the number of people it helps is tiny. That’s why doctors and families must look at RRR and ARR. It’s not just about percentages but about real people and choices.
Understanding RRR and ARR gives us a fuller picture of a treatment’s potential benefits and helps us make the right decisions for our loved ones. It’s a tool that, when used wisely, can guide us through the tough choices we face in caring for someone with a terminal illness.
Understanding medical information can be as challenging as the situation itself when we’re helping a loved one through a terminal illness. Two terms often arise: Absolute Risk Reduction (ARR) and Relative Risk Reduction (RRR). Although they may sound similar, they differ and can significantly affect treatment decisions.
Absolute Risk Reduction gives us the number of people out of one hundred who will benefit from treatment. It’s like saying, “This medicine will help 3 out of every 100 people avoid a heart attack.” It’s clear and helps us see the actual effect of a treatment.
Relative Risk Reduction is more about comparison. It tells us how much the risk decreases in percentage compared to something else, like a different treatment or no treatment. It’s like saying, “This medicine cuts the risk of a heart attack by half.” But remember, if the original risk is exceedingly small, cutting it by half might not mean much in real numbers.
The implications are huge. ARR helps us make decisions based on real-life chances, while RRR can sometimes make a treatment look better than it might be.
Some common misunderstandings about ARR and RRR can trip us up. Some people think a high RRR means treatment is super effective, but we can’t see the whole picture without knowing the ARR. It’s like hearing that a sale is “50% off” but not knowing the original price—it sounds great, but we need more information to understand the value.
Another misconception is that ARR and RRR are always related but can tell different stories about the same treatment. That’s why it’s important to consider both when you’re considering treatment options for your loved one.
By understanding ARR and RRR, you can have more meaningful conversations with doctors and make choices that genuinely fit your loved one’s needs and wishes. It’s not just about the numbers but what those numbers mean for your family’s journey.
Anticoagulants are used to prevent blood clots and reduce the risk of stroke, especially in patients with atrial fibrillation.
| Anticoagulant | ARR | RRR |
|---|---|---|
| Apixaban | 0.77 for thromboembolic events | 38% for major bleeding |
| Dabigatran | 0.6% per year for stroke/systemic embolism | Not specified |
| Edoxaban | 0.72 | Not specified |
| Rivaroxaban | 0.6 | Not specified |
| Warfarin | 1.95% | Not specified |
Antidepressants are prescribed to treat various psychiatric conditions, including depression and anxiety disorders.
| Antidepressant | ARR | RRR |
|---|---|---|
| Citalopram | 1.12% | 12% |
| Fluoxetine | 1.10% | 58% |
| Paroxetine | 0.87% | 12% |
| Sertraline | 10% | Not specified |
| Venlafaxine | 3% | Not specified |
These medications are used to manage symptoms of Alzheimer’s disease and other types of dementia.
| Medication | ARR | RRR |
|---|---|---|
| Donepezil | 3% | 3% |
| Galantamine | 15.5% | 59% |
| Lecanemab | 31% | 37% |
| Memantine | 13.8% | 31% |
| Rivastigmine | 2.3% | Not specified |
Statins are commonly prescribed to lower cholesterol and reduce the risk of cardiovascular events. Here’s a comparison of absolute and relative risk reductions for various statins (keep in mind the side effects of worsening cognition leading to dementia, worsening blood sugar levels leading to pre-diabetes or worsening diabetes, muscle aches and pains, muscle tendon rupture:
| Statin | Absolute Risk Reduction (ARR) | Relative Risk Reduction (RRR) |
|---|---|---|
| Atorvastatin | 0.8% for all-cause mortality | 9% for all-cause mortality |
| Fluvastatin | 0.6% for major vascular events | Estimated 30% for moderate intensity |
| Lovastatin | Similar to Atorvastatin | Similar to Atorvastatin |
| Pravastatin | 0.8% for all-cause mortality | 9% for all-cause mortality |
| Rosuvastatin | Proportional to patient’s cardiovascular disease risk | Approximately 30% |
| Simvastatin | 0.8% for all-cause mortality | 9% for all-cause mortality |
In the journey of terminal illness, making treatment decisions can be one of the most complex parts. It’s a road walked with doctors, nurses, and most importantly, your loved one. Here’s how to navigate these choices with care and understanding.
Talking with healthcare professionals is key. They can explain things like Absolute Risk Reduction (ARR) and Relative Risk Reduction (RRR) in a way that makes sense. They’ll help you understand what treatments can do and what they can’t. Finding the best path forward is a team effort; these conversations are the map.
Quality of life is just as important as length of life. Sometimes, the goal might be to have more good days, even if it means having fewer days overall. It’s about what feels right for your loved one—trying every possible treatment or focusing on comfort and cherished moments.
Deciding whether to continue, taper, or stop medications can be challenging. Look at the ARR to see the real benefits. If a medicine is truly helping, it might be worth the side effects. But if the ARR is small and the medicine is causing discomfort, it might be time to discuss easing off or stopping it.
Remember, these decisions are deeply personal. They’re about your loved one’s wishes, beliefs, and what makes life meaningful for them. With the guidance of healthcare professionals and a clear understanding of ARR and RRR, you can make informed choices that honor those wishes and celebrate the life they’ve lived.
As we conclude our guide on risk reduction, it’s important to consider how this knowledge can empower you and your family during a time that may feel overwhelming.
Knowledge is a powerful tool, especially when it comes to making healthcare decisions for a loved one with a terminal illness. Understanding the concepts of Absolute Risk Reduction (ARR) and Relative Risk Reduction (RRR) can help you see through the numbers and focus on what they mean for your loved one’s care. It’s about being equipped to have open, informed conversations with doctors and feeling confident in the choices you make together.
The journey ahead with terminal illness is a personal one, and no two paths are the same. As you move forward, remember that it’s not just about the length of time but the quality of the moments shared. Decisions about treatments and medications are not just medical choices; they’re choices about life and how your loved one wants to live it.
In this journey, you’re not alone. Healthcare professionals, support groups, and resources are available to help you. With the knowledge you’ve gained about ARR and RRR, you’re better prepared to navigate the road ahead, making decisions that honor your loved one’s wishes and bring peace to your family.
Thank you for taking the time to learn and understand these critical concepts. May this knowledge bring you strength and guidance as you support your loved one through this chapter of life.
Absolute Risk Reduction: Your Secret Weapon in Literature Evaluation
Reporting the findings: Absolute vs. relative risk
Sneaky Research? Absolute Versus Relative Risk Reduction: The Way It Can Be Used To Trick You (Youtube)
Understanding the Risks of Medical Interventions
Calculating absolute risk and relative risk
REVEALED: How Doctors and Medicine FOOL YOU (YouTube)
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series