Understanding and Coping with End-of-Life Anger: A Guide for Caregivers
Published on July 20, 2024
Updated on June 20, 2025
Published on July 20, 2024
Updated on June 20, 2025
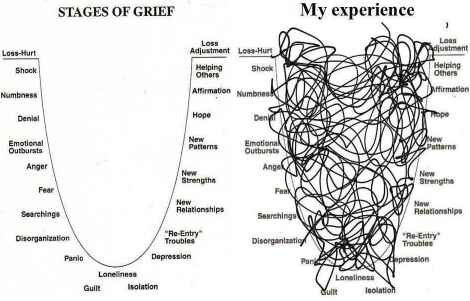
Table of Contents
Watching a loved one approach the end of their life is never easy. It’s even harder when they act differently than someone you’ve known and loved for so long. These changes can be confusing and upsetting, but understanding them can help you navigate this challenging time with more compassion and patience.
End-of-life personality changes are behavior, mood, or character shifts often occurring in people nearing death. These sudden or gradual changes may surprise family members and caregivers.
It’s important to remember that these changes:
Some common end-of-life personality changes include:
Various factors can cause these changes:
| Physical Factors | Emotional Factors | Mental Factors |
|---|---|---|
| Pain | Fear of death | Confusion |
| Medication side effects | Loss of independence | Dementia |
| Organ failure | Unresolved issues | Delirium |
Anger is one of the most challenging emotions for caregivers and family members. It’s hard not to take it personally when someone you care for lashes out in anger. But remember, this anger usually isn’t about you – it’s about the situation.
Anger in terminally ill patients can manifest in various ways:
It’s crucial to understand that these manifestations of anger often stem from:
Here’s a breakdown of how anger might manifest at different stages:
| Stage | Common Anger Manifestations |
|---|---|
| Early Stage | Irritability, snapping at loved ones, expressing frustration with diagnosis. |
| Middle Stage | Refusal of care, verbal outbursts, withdrawal from activities |
| Late Stage | Physical restlessness, agitation, attempts to leave |
Remember, as a caregiver or family member, your role is crucial. By understanding these changes and manifestations of anger, you can:
In the following sections, we’ll explore strategies to help you cope with these challenges and support your loved one through their end-of-life journey.
Understanding why your loved one might be experiencing anger can help you respond with more compassion and patience. End-of-life anger is often complex, with multiple factors contributing to these difficult emotions. Let’s explore the leading causes:
Physical discomfort can significantly impact a person’s mood and behavior. Here are three key physical factors that can contribute to anger:
Chronic pain can be incredibly frustrating and exhausting for your loved one. It can lead to:
Remember, your loved one might not always be able to express their pain clearly. Watch for non-verbal signs of discomfort, such as:
Many medications used in end-of-life care can have side effects that affect mood and behavior. Some common examples include:
| Medication Type | Possible Side Effects |
|---|---|
| Pain medications (opioids) | Confusion, agitation, hallucinations |
| Steroids | Mood swings, irritability, aggression |
| Anti-nausea drugs | Restlessness, anxiety |
| Anticholinesterase (medications to slow dementia progression) | Agitation, anxiety, restlessness |
| Antidepressants (SSRIs) | Anxiety, agitation, restlessness |
| Anticonvulsants (like Gabapentin) | Agitation, irritability, restlessness |
If you notice sudden changes in your loved one’s behavior, discussing this with their healthcare team is essential. They may be able to adjust medications or dosages to help manage these side effects.
Terminal delirium is a state of confusion that can occur in the final days or hours of life. It can cause:
Terminal delirium can be very distressing for both the patient and their loved ones. It’s important to remember that this is a common part of the dying process and not a reflection of your care.
Emotional factors play a significant role in end-of-life anger. Here are three key emotional causes:
Facing mortality can bring up intense emotions. Your loved one might be experiencing:
These fears can manifest as anger, which might feel easier to express than vulnerability.
As their illness progresses, your loved one may feel like they’re losing control over:
This loss of control can be incredibly frustrating and may lead to angry outbursts or attempts to exert control in other ways.
Near the end of life, people often reflect on their past. This can bring up:
These unresolved issues can lead to anger, guilt, or frustration.
Changes in cognitive function can also contribute to anger and challenging behaviors. Here are two main cognitive factors:
Confusion can be caused by various factors, including:
When confused, your loved one might become:
Dementia can significantly affect behavior and mood. Different types of dementia can cause different symptoms:
| Type of Dementia | Common Behavioral Changes |
|---|---|
| Alzheimer’s Disease | Aggression, mood swings, wandering |
| Vascular Dementia | Depression, apathy, emotional lability |
| Lewy Body Dementia | Hallucinations, sleep disturbances, paranoia |
| Frontotemporal Dementia | Impulsivity, loss of empathy, socially inappropriate behavior |
In the context of end-of-life care, dementia can make it even more challenging for your loved one to understand and cope with their situation, potentially leading to increased anger and agitation.
Understanding these causes doesn’t make dealing with anger easy, but it can help you approach your loved one with more empathy and patience. The following sections will explore strategies for managing these challenging behaviors and emotions.
As a caregiver or family member, understanding how anger manifests in your loved one can help you respond more effectively and compassionately. Anger at the end of life can take various forms, and it’s essential to recognize that these expressions of anger are often rooted in fear, frustration, or pain rather than directed at you.
Let’s explore the three main types of anger you might encounter:
Internally directed anger is when your loved one turns it inward, often blaming themselves or feeling guilty about their situation. This type of anger can be harder to spot because it might not involve outward displays of frustration.
Signs of internally directed anger:
Here’s how internally directed anger might manifest at different stages:
| Stage of Illness | Possible Manifestations |
|---|---|
| Early Stage | Self-blame for illness, expressions of regret about past choices |
| Middle Stage | Refusing treatment, isolating from loved ones |
| Late Stage | Giving up on life, refusing food or medication |
How you can help:
Externally directed anger is when your loved one expresses it outwardly, often targeting those closest to them, including caregivers and family members. This type of anger can be challenging, but remember, it’s frequently not about you.
Signs of externally directed anger:
Here’s a breakdown of how externally directed anger might escalate:
| Level of Anger | Behaviors | How to Respond |
|---|---|---|
| Mild | Irritability, sarcasm, complaining | Listen actively, acknowledge feelings |
| Moderate | Yelling, criticizing, refusing care | Stay calm, offer choices, give space if safe |
| Severe | Physical aggression, violent outbursts | Ensure safety, seek help, use de-escalation techniques |
How you can help:
Terminal agitation and restlessness are common end-of-life symptoms that can be distressing for both the patient and their loved ones. While not always associated with anger, these symptoms can manifest as irritability or aggression.
Signs of terminal agitation and restlessness:
It’s important to note that terminal agitation often occurs in the final days or hours of life. Here’s how it might progress:
| Time Frame | Possible Symptoms |
|---|---|
| Days Before | Increased anxiety, difficulty sleeping, mild confusion |
| Hours Before | Restlessness, agitation, attempting to leave, hallucinations |
| Final Moments | Severe agitation, delirium, unresponsiveness |
How you can help:
Recognizing these different types of anger is the first step in providing compassionate care. Each person’s experience is unique, and your loved one may display a combination of these anger types or shift between them.
In the following sections, we’ll explore strategies for managing these types of anger and supporting your loved one through this challenging time. Always remember to take care of yourself, too – caregiving can be emotionally and physically demanding, and seeking support when needed is essential.
Caring for a loved one at the end of their life is a profound act of love and compassion. However, it can also be incredibly challenging, especially when dealing with anger and problematic behaviors. Recognizing the impact this can have on you as a caregiver or family member is essential. Understanding these effects can help you take better care of yourself and, in turn, provide better care for your loved one.
The emotional impact of caring for an angry or agitated loved one can be significant. You might experience a range of intense emotions, including:
These emotions can manifest in different ways:
| Emotion | How It Might Manifest | Self-Care Strategies |
|---|---|---|
| Sadness | Crying frequently, loss of interest in activities | Allow yourself to grieve, seek support from friends or a counselor |
| Guilt | Overworking yourself, neglecting self-care | Practice self-compassion, remind yourself you’re doing your best |
| Anxiety | Trouble sleeping, racing thoughts | Try relaxation techniques, consider talking to a therapist |
| Anger | Irritability, outbursts | Find healthy outlets for anger (exercise, journaling), take breaks when needed |
| Helplessness | Feeling overwhelmed, wanting to give up | Focus on what you can control, celebrate small victories |
Remember, it’s normal and okay to have these feelings. Acknowledging them is the first step in managing them effectively.
Caregiving can be physically demanding, especially when your loved one is experiencing anger or agitation. The physical toll can include:
Here are some signs that you might be experiencing physical exhaustion:
To combat physical exhaustion:
Caring for an angry or agitated loved one can strain your relationships with the person you care for and others in your life.
With the person you’re caring for:
With other family members:
With friends and your social life:
Here’s how relationships might be affected at different stages of caregiving:
| Stage of Caregiving | Potential Relationship Challenges |
|---|---|
| Early Stage | Adjusting to new roles, initial family conflicts over care decisions |
| Middle Stage | Increasing isolation from friends, growing resentment among family members |
| Late Stage | Severe strain on relationships with loved ones, potential breakdown of family relationships |
Strategies for managing relationship strain:
Remember, taking care of yourself is not selfish – it’s necessary. By recognizing and addressing the impact of caregiving on your emotional and physical well-being and relationships, you can better sustain your ability to provide compassionate care for your loved one.
In the following sections, we’ll explore specific strategies for coping with these challenges and finding support during this difficult time.
Caring for a loved one who is experiencing anger at the end of life can be challenging. However, there are strategies you can use to make this difficult time more manageable for both you and your loved one. Remember, every situation is unique, so feel free to adapt these strategies to fit your specific circumstances.
One of the most powerful things you can do as a caregiver is to understand and validate your loved one’s emotions. This doesn’t mean you agree with everything they say or do, but rather that you recognize their feelings as real and vital.
Steps to understand and validate emotions:
Here’s how you might validate different emotions:
| Emotion | Validation Statement |
|---|---|
| Anger | “I can see how upset you are. This situation is really difficult.” |
| Fear | “It’s understandable to be scared. This is a big unknown.” |
| Frustration | “I understand how frustrating this must be for you. You’re dealing with a lot.” |
| Sadness | “It’s okay to feel sad. This is a huge loss.” |
Good communication is key when dealing with end-of-life anger. Two instrumental techniques are active listening and the BATHE approach.
Active listening involves fully concentrating on what your loved one is saying rather than passively hearing it.
Steps for active listening:
The BATHE technique is a valuable tool for addressing emotional concerns. Here’s how to use it:
A peaceful environment can help reduce agitation and anger. Here are some ways to create a calming atmosphere:
Here’s a quick guide to creating a calm environment at different times of day:
| Time of Day | Environmental Adjustments |
|---|---|
| Morning | Open curtains for natural light, play soft morning music |
| Afternoon | Ensure comfortable room temperature, offer a cozy space for rest |
| Evening | Dim lights, reduce noise, create a peaceful bedtime routine |
While caring for your loved one, it is crucial to take care of yourself. This includes setting healthy boundaries and practicing self-care.
Setting boundaries:
Self-care strategies:
Remember, self-care isn’t selfish. You’ll be better equipped to care for your loved one by taking care of yourself.
| Self-Care Area | Examples |
|---|---|
| Physical | Regular exercise, balanced meals, adequate sleep |
| Emotional | Journaling, talking with friends, counseling |
| Social | Maintaining friendships, joining support groups |
| Spiritual | Meditation, prayer, spending time in nature |
By implementing these strategies, you can better manage the challenges of caregiving and provide compassionate care for your loved one while also taking care of yourself. Remember, it’s okay to ask for help when needed, and it’s essential to be kind to yourself during this difficult time.
Caring for a loved one at the end of life can sometimes involve dealing with challenging behaviors. These behaviors are often a result of the physical and emotional stress your loved one is experiencing. Understanding how to manage these behaviors can help you provide better care and reduce stress for you and your loved one.
Medication refusal is a common issue in end-of-life care. Your loved one might refuse medication for various reasons:
Strategies to manage medication refusal:
| Reason for Refusal | Possible Solution |
|---|---|
| Difficulty swallowing | Ask about liquid or patch alternatives. |
| Forgetfulness | Discuss concerns with the healthcare provider and consider adjusting dosage or timing. |
| Fear of side effects | Discuss concerns with the healthcare provider and consider adjusting dosage or timing. |
| Feeling overwhelmed | Work with the doctor to simplify the medication regimen if possible. |
Your loved one might resist care for various reasons, including fear, confusion, pain, or a desire for independence. This can be particularly challenging regarding essential care like bathing or changing clothes.
Strategies to manage resistance to care:
Remember, forcing care can lead to more resistance and distress. If the care isn’t immediately essential, it’s okay to try again later.
Verbal aggression can be hurtful and challenging to deal with. It’s important to remember that this behavior is often a result of the person’s illness or situation, not a reflection on you.
Strategies to manage verbal aggression:
| Type of Verbal Aggression | Example Response |
|---|---|
| Accusations | “I understand you’re upset. Let’s talk about what’s bothering you.” |
| Name-calling | “I know you’re frustrated. How can I help you feel more comfortable?” |
| Threats | “I can see you’re angry. I want to help. Let’s take a few deep breaths together.” |
Physical aggression can be scary and potentially dangerous. Your safety and the safety of your loved one are the top priorities.
Strategies to manage physical outbursts:
If physical aggression is frequent or severe, it’s crucial to discuss this with your loved one’s healthcare team. They may be able to adjust medications or suggest other interventions.
General tips for all challenging behaviors:
| Behavior | Do | Don’t |
|---|---|---|
| Medication Refusal | Explain importance, offer choices | Force medication, get angry |
| Resistance to Care | Be patient, offer options | Rush or force care |
| Verbal Aggression | Stay calm, validate feelings | Argue or take it personally |
| Physical Outbursts | Ensure safety, use de-escalation techniques | Restrain or confront physically |
Remember, these challenging behaviors are often a result of the illness, not a reflection of your loved one’s true feelings or your caregiving abilities. By approaching these situations with patience, understanding, and the right strategies, you can help manage these behaviors and provide compassionate care during this difficult time.
As a caregiver or family member of a loved one experiencing end-of-life anger, it’s crucial to recognize when additional support is needed. This section will guide you through seeking professional help, including when to involve healthcare professionals, the benefits of palliative care and hospice support, and the importance of counseling for caregivers.
Knowing when to reach out to healthcare professionals can make a significant difference in managing your loved one’s anger and improving their quality of life. Here are some signs that indicate it’s time to seek help:
Who to contact:
Remember: Seeking help early is always better than waiting for a crisis.
Palliative care and hospice services can provide invaluable support for both your loved one and your family during this challenging time.
| Aspect | Description |
|---|---|
| Focus | Improving quality of life for patients with serious illnesses |
| Timing | Can be provided at any stage of illness, alongside curative treatments |
| Services | Pain management, symptom control, emotional support, care coordination |
| Team | Doctors, nurses, social workers, chaplains, and other specialists |
| Aspect | Description |
|---|---|
| Focus | Comfort and quality of life for patients with terminal illnesses |
| Timing | Typically, for patients with a life expectancy of six months or less |
| Services | Pain relief, symptom management, emotional and spiritual support |
| Team | Similar to palliative care, with an added focus on end-of-life needs |
Benefits of palliative care and hospice for managing anger:
How to access these services:
Caring for a loved one experiencing end-of-life anger can take a significant emotional toll. Seeking counseling for yourself is not selfish – it’s essential for your well-being and ability to provide the best care possible.
Benefits of counseling for caregivers:
Types of counseling to consider:
Finding the proper counseling support:
Remember: Taking care of your mental health is crucial. It allows you to be more present and effectively support your loved one through their end-of-life journey.
By seeking professional help when needed, you’re not admitting defeat or failing your loved one. Instead, ensure you and your loved one receive the best support during this challenging time. Remember, you don’t have to face this journey alone – professionals are ready to help you navigate end-of-life care’s complex emotions and challenges.
Caring for a loved one at the end of their life is an emotionally challenging journey. It’s natural to experience a wide range of intense feelings, including guilt, grief, and a sense of overwhelming responsibility. This section will help you navigate these complex emotions and find the support you need during this difficult time.
Guilt is a common emotion for caregivers and family members of those nearing the end of life. You might feel guilty for various reasons:
Remember: These feelings are normal and don’t make you a bad person or caregiver.
Here are some strategies to help you cope with guilt:
| Guilt-Inducing Thought | Reframing the Thought |
|---|---|
| “I’m not doing enough.” | “I’m doing the best I can with the resources I have.” |
| “I shouldn’t need a break.” | “Taking care of myself allows me to provide better care.” |
| “I should have done things differently in the past.” | “I made the best decisions I could with the information I had at the time.” |
| “I shouldn’t feel angry or frustrated.” | “It’s normal to have a range of emotions in this challenging situation.” |
Grief is a complex emotion that often begins before your loved one passes away. This is known as anticipatory grief. It’s important to recognize and process these feelings as they arise.
Stages of Grief
While everyone experiences grief differently, understanding the common stages can help you navigate your emotions:
Remember: These stages are not linear, and you may move back and forth between them.
Here are some strategies to help you process your grief:
A strong support system is crucial when caring for a loved one at the end of life. Here are some ways to build and maintain your support network:
| Type of Support | Examples | How to Access |
|---|---|---|
| Emotional Support | Friends, family, support groups, therapists | Reach out directly, join local groups, ask for referrals |
| Practical Help | Neighbors, church members, volunteer organizations | Ask for specific tasks, use online care calendars |
| Medical Support | Doctors, nurses, home health aides | Consult with healthcare providers, contact local agencies |
| Spiritual Support | Clergy, spiritual advisors, meditation groups | Contact local religious organizations, seek out community centers |
Remember: Seeking support is a sign of strength, not weakness. You don’t have to face this challenging time alone.
By actively coping with your own emotions, processing your grief, and building a strong support system, you’ll be better equipped to care for your loved one while also taking care of yourself. Remember to be patient and kind to yourself throughout this journey. Your well-being is just as important as that of your loved one.
As your loved one approaches the end of their life, you may face a mix of emotions and practical challenges. This section will guide you through having difficult conversations, making necessary arrangements, and finding meaningful moments of connection during this profound time.
Engaging in open, honest conversations about end-of-life matters can be daunting. Still, it’s crucial to ensure your loved one’s wishes are respected and to provide closure for all involved.
Key topics to discuss:
Tips for initiating and navigating these conversations:
| Topic | Conversation Starter |
|---|---|
| Medical Decisions | “Have you thought about what kind of medical care you’d want if you couldn’t speak for yourself?” |
| Legal Matters | “I want to make sure we respect your wishes. Have you considered creating or updating your will?” |
| Funeral Wishes | “I know it’s not easy to talk about, but do you have any preferences for your memorial service?” |
| Personal Legacy | “What are the most important things you’d like people to remember about you?” |
| Unresolved Issues | “Is there anything you’d like to discuss or resolve before it’s too late?” |
Remember, these conversations can be emotional for everyone involved. Take breaks if needed, and don’t hesitate to seek support from a counselor or spiritual advisor to help guide these discussions.
While it may feel overwhelming, addressing practical matters can provide peace of mind for you and your loved one. Here’s a checklist of essential arrangements to consider:
Tips for managing these arrangements:
| Category | Tasks | Status |
|---|---|---|
| Legal | Will, Advance Directive, Power of Attorney | |
| Financial | Account List, Bill Payment Plan | |
| Healthcare | Hospice Setup, Equipment Needs | |
| After-Death | Funeral Plans, Obituary | |
| Personal Affairs | Document Location, Digital Legacy |
Amidst the practical concerns and emotional challenges, creating opportunities for meaningful connection and moments of peace with your loved one is crucial.
Ways to foster connection and create lasting memories:
Finding peace in difficult moments:
Remember, peace and connection can be found in small, everyday moments. Don’t underestimate the power of your presence and caring touch.
| Hold hands, offer light massages, or sit close by | Description | Benefits |
|---|---|---|
| Memory Sharing | Look through photo albums together, sharing stories and laughter | Strengthens bonds, provides joy, creates new memories |
| Music Therapy | Listen to favorite songs or have live music performances | Reduces anxiety, improves mood, facilitates emotional expression |
| Nature Connection | Bring flowers, plants, or natural objects indoors; sit by a window | Promotes calm, connects to larger world, stimulates senses |
| Gentle Touch | Promotes calm, connects to the larger world, stimulates senses | It provides comfort, reduces pain, enhances the feeling of connection |
| Legacy Project | Create a memory book, record stories, or write letters together | It gives a sense of purpose and leaves lasting memories for the family |
As you navigate this challenging time, remember that there is no “right” way to prepare for the end of a loved one’s life. Be gentle with yourself and your loved one, allowing space for all emotions and experiences. By addressing practical matters, having meaningful conversations, and creating moments of connection, you can help ensure a peaceful and meaningful transition for your loved one while also finding solace and closure for yourself.
As we reach the end of our exploration into understanding and managing end-of-life anger in loved ones, it’s essential to step back and reflect on the broader context of this challenging experience. Let’s consider how we can reframe anger as part of the journey and focus on compassion and understanding.
When faced with a loved one’s anger during their final days, it’s natural to feel hurt, frustrated, or resentful. However, by reframing this anger, we can find a more peaceful and meaningful way to navigate this difficult time.
Key points to remember about end-of-life anger:
Strategies for reframing anger:
| Instead of Thinking… | Try Reframing It As… |
|---|---|
| “They’re always so angry at me.” | “They’re struggling with difficult emotions and feel safe expressing them around me.” |
| “Why can’t they be more grateful?” | “What unmet needs might they be trying to communicate through this anger?” |
| “This anger is ruining our last days together.” | “This is one part of a complex emotional journey we’re going through together.” |
| “I can’t handle their anger anymore.” | “This is challenging, but it’s an opportunity for me to practice patience and understanding.” |
| “Their anger means they don’t care about me.” | “They can feel angry and still love and appreciate me simultaneously.” |
As challenging as it can be to face anger from a dying loved one, approaching the situation with compassion and understanding can make a world of difference. It can help ease your loved one’s distress, strengthen your connection, and bring peace to both of you during this difficult time.
Ways to cultivate compassion and understanding:
Remember: Your compassion and understanding are powerful gifts you can offer your loved one during this time.
Dealing with end-of-life anger is undoubtedly one of the most challenging aspects of caring for a dying loved one. It requires patience, resilience, and a great deal of emotional strength. But by reframing this anger as part of the journey and approaching it with compassion and understanding, you can transform these difficult moments into opportunities for deeper connection and healing.
As you navigate this path, remember to be kind to yourself. Seek support when needed, take time for self-care, and honor your feelings along the way. Even in the face of anger, your presence and care is a profound act of love.
Ultimately, what matters most is not the absence of difficult emotions but the presence of love, understanding, and compassion. By focusing on these, you can help create a peaceful and meaningful end-of-life experience for your loved one and find solace in knowing you’ve supported them through one of life’s most challenging transitions.
Dealing With the Angry Dying Patient
End-of-Life Personality Changes: Dealing with Anger Before Death
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
On Grief and Grieving: Finding the Meaning of Grief Through the Five Stages of Loss
Finding Meaning: The Sixth Stage of Grief
It’s OK That You’re Not OK: Meeting Grief and Loss in a Culture That Doesn’t Understand
Need Help Dealing with Grief? GriefShare Grief & Loss Support Groups Are Here for You
Children’s Grief Resources
For Ages 4-6
For Ages 6-8
For Ages 8-10
For Ages 11-13
For Ages 13-18
Specialized Grief Resources
Young Adult Literature Exploring Grief:
Helpful Online Resources
Enhanced Online Resources for Teens
Specialized Teen Platforms
Comprehensive Teen Support Centers
Interactive Support Options
Educational Resources for Teens and Families
Oral Ketamine in Palliative Care: A Promising Approach for Emotional and Psychological Distress
Crisis Management at End-of-Life
The Dying Process at the End of Life
The Transitioning Phase Of The Dying Process
Understanding Terminal Restlessness
Delirium vs Terminal Restlessness
Managing Terminal Restlessness
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Anger Stage of Grief: Examples, What to Expect, & How to Cope
The Importance of Understanding the Five Stages of Grief
Why the Five Stages of Grief Theory Is Wrong
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.