Top Ten Myths About Do Not Resuscitate (DNR) Orders
Published on September 4, 2024
Updated on September 6, 2024
Published on September 4, 2024
Updated on September 6, 2024
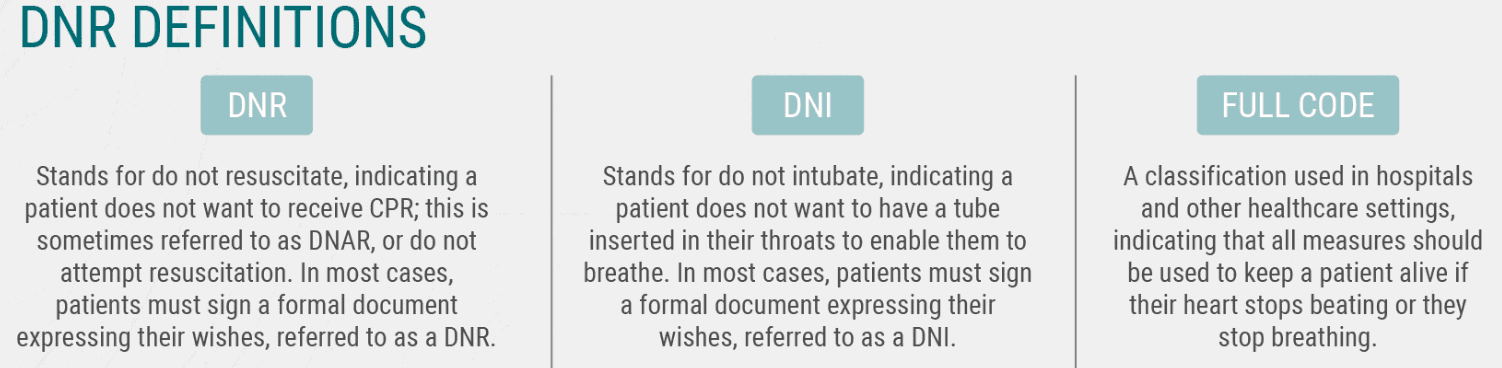
Table of Contents
If you or your loved one has a severe illness, you may have heard about the do not resuscitate (DNR) order. This medical order tells the health care team what to do if the patient’s heart stops beating or they stop breathing. It is an incredibly crucial decision that can affect the quality and length of life. However, many myths and misunderstandings about DNR orders can make it hard to choose what is best for you or your loved one. This article will explain what DNR order means and why it is essential to understand it. We will also debunk the top ten myths about DNR orders and share the facts that can help you make an informed and respectful choice.
Please note that the DNR order is meant to be a refusal to receive CRP; if there is no DNR order, CRP is the default.
One of the most common myths about DNR orders is that they mean do not treat. This is not true. A DNR order only applies to one specific situation: when the patient’s heart stops beating or they stop breathing. In that case, the healthcare team will not perform cardiopulmonary resuscitation (CPR) or use machines to restart the heart or lungs. However, DNR orders do not affect any other treatments that the patient may need or want.
For example, a patient with a DNR order can still receive antibiotics, pain medication, fluids, nutrition, surgery, chemotherapy, or any other treatment that may improve their condition or comfort. DNR orders do not mean giving up on the patient or withholding care. It simply means respecting the patient’s wishes about how they want to die.
Another common myth about DNR orders is that they mean comfort measures only. This is also not true. Comfort measures aim to relieve pain and suffering but do not attempt to cure or prolong life. For example, comfort measures may include morphine, oxygen, sedation, or hospice care. Comfort measures differ from life-sustaining treatments, which try to keep the patient alive but may not improve their quality of life. For example, life-sustaining treatments may include CPR, ventilators, feeding tubes, or dialysis. Comfort measures and life-sustaining treatments are not mutually exclusive. A patient with a DNR order can choose to receive both, neither, or some, depending on their goals and preferences. Comfort measures are only a separate medical order that tells the health care team to focus on palliative care and not to use any life-sustaining treatments, even if the patient is not dying. Comfort measures differ from DNR orders and require a different discussion and documentation.
Some patients may prefer comfort measures only over life-sustaining treatments, especially if they have a terminal illness or a poor prognosis. Comfort measures help them die peacefully and with dignity without hastening death and unnecessary interventions or complications. However, comfort measures also have some limitations and risks. Comfort measures may not be enough to control all the symptoms or distress the patient may experience. Comfort measures only may also hasten the patient’s death, as some life-sustaining treatments may prolong survival. Comfort measures are a personal and complex decision that should be made with the help of the health care team, the patient’s family, and the patient’s spiritual or religious advisor. Comfort measures are not a default option for patients with DNR orders, and they should not be assumed or imposed without the patient’s consent.
Another common myth about DNR order is that it means hospice care. This is also not true. Hospice care is a type of care that focuses on improving the quality of life for patients who have a terminal illness and a life expectancy of six months or less. Hospice care provides physical, emotional, social, and spiritual support to the patient and their family at home and in other settings. Hospice care does not aim to cure or prolong life but to help the patient live as comfortably and fully as possible until they die. Hospice care is different from other types of care, such as curative care, palliative care, or long-term care. Curative care tries to treat the underlying cause of the illness and restore health. Palliative care tries to relieve the symptoms and suffering caused by the illness but does not necessarily stop the disease’s progression. Long-term care assists with daily activities and personal care for patients with chronic or disabling conditions. Hospice care is a special kind of palliative care only offered to patients near the end of life.
A common misconception is that hospice care requires a DNR order. This is not true either. Hospice care does not mandate or impose any medical orders on the patient. The patient can choose whether to have a DNR order and any other treatments they want or need. Hospice care respects the patient’s autonomy and dignity and supports the patient’s decisions about end-of-life care. However, hospice care also educates and counsels the patient and their family about the benefits and burdens of different treatments and helps them understand the goals and expectations of hospice care. Hospice care encourages patients to have honest and open conversations about their wishes and values with their healthcare team, family, and spiritual or religious advisors. Hospice care also helps the patient prepare an advance directive, a document that states the patient’s preferences. It appoints a surrogate decision-maker if the patient cannot speak for themselves. Hospice care is not a one-way ticket to death but a compassionate and holistic approach to end-of-life care. Hospice care differs from DNR order and should not be confused or conflated.
There are some hospice agencies whose policy requires DNR orders to be on their service, but this is not a federal mandate or federal law.
Another common myth about DNR orders is that it means giving up hope. This is also not true. Choosing a DNR order does not mean that the patient has lost hope or faith in their recovery or survival. It also does not mean that the patient is depressed or suicidal. Choosing a DNR order is a personal and rational decision that reflects the patient’s realistic assessment of their situation and their preferences for their end-of-life care. Choosing DNR orders can be a sign of hope, as it shows that the patient has hope for a peaceful and dignified death without unnecessary pain or suffering. Choosing DNR orders can also free the patient from the fear and anxiety of unwanted or futile interventions and allow them to focus on the things that matter most to them, such as their family, their friends, their hobbies, their legacy, or their spirituality.
When a patient chooses to have a DNR order, family members may experience feelings of sadness, guilt, confusion, or even anger. However, it is essential to respect the patient’s values and goals and support their decision with compassion and understanding. It is also necessary to communicate and share the patient’s DNR orders with the healthcare team so that they can honor the patient’s wishes and provide the best possible care. Choosing DNR orders does not mean giving up hope but expressing hope for a different outcome. DNR orders are not a pessimistic choice but a positive and courageous one.
Another common myth about DNR orders is that they are irreversible. This is also not true. The patient or their surrogate can change or revoke their DNR order at any time. The patient or their surrogate has the right to change their mind about DNR orders and to request or refuse any treatments that they may want or need. DNR orders are not permanent or binding decisions but flexible and dynamic ones that can be adjusted according to the patient’s condition and preferences.
In some states, a surrogate may not revoke a DNR order that the patient executed for themselves.
However, changing or revoking DNR orders requires clear and effective communication and documentation. The patient or their surrogate should inform the health care team, the family, and the spiritual or religious advisor about any changes in DNR orders and explain the reasons and motivations behind them. The healthcare team should respect and acknowledge the patient’s or surrogate’s decision and update the medical records and charts accordingly. The patient or their surrogate should also ensure the DNR order is visible and accessible to the healthcare team, especially in emergencies. If they have one, the patient or their surrogate should also review and revise the advance directive to reflect any changes in DNR orders. Changing or revoking a DNR order is a valid and legitimate option for the patient or their surrogate, but it should be done carefully and cautiously. Changing or revoking DNR order is not a sign of weakness or inconsistency but a sign of autonomy and empowerment.
Another common myth about DNR orders is that it applies to all situations. This is also not true. DNR orders are not a one-size-fits-all order but a context-specific one that depends on the setting and the circumstances. Several types of DNR orders have different meanings and implications. For example, some of the common types of DNR orders are:
If you want others to know about your DNR orders, it’s a good idea to wear a bracelet or necklace indicating so.
DNR orders can vary depending on the state or the country where the patient lives or travels. States or countries may have different laws, regulations, forms, or protocols for DNR orders. Therefore, checking and confirming the validity and recognition of DNR orders across different jurisdictions is essential. It is also vital to carry and display the DNR order or a copy of it in a visible and accessible place, such as a wallet, a bracelet, a necklace, or a refrigerator, so that the health care team and the EMS or the first responders can identify and honor it.
DNR orders can also be challenging and limited in emergencies. Sometimes, the health care team, the EMS, or the first responders may not be aware of or able to find the DNR order in time, and they may start CPR or use machines to restart the heart or lungs by default. Sometimes, the patient or their surrogate may change their mind about the DNR order in the heat of the moment, and they may request or refuse CPR or machines to restart the heart or lungs contrary to the DNR order. Sometimes, the health care team, the EMS, or the first responders may have doubts or conflicts about the DNR order’s validity or appropriateness and hesitate or refuse to follow it. These situations can create confusion, frustration, or distress for the patient, their family, the health care team, the EMS, or the first responders. Therefore, it is essential to communicate and document the DNR orders clearly and consistently and resolve any issues or concerns as soon as possible. DNR orders are not a universal or absolute order but a situational and relative one.
Another common myth about DNR orders is that they are legally binding. This is close to the truth, but not always. DNR is a medical order that tells the health care team what to do if the patient’s heart stops beating or they stop breathing. It is based on the patient’s informed consent, which means the patient has the right to accept or refuse any medical treatment, including CPR. However, DNR orders are not a contract or a guarantee. The patient or their surrogate can change or revoke it anytime if they can make decisions. It can also be challenged or overridden by the health care team in some situations, such as when the patient’s condition changes, when the DNR order is unclear or invalid, or when the DNR order conflicts with the professional judgment or ethical principles of the health care team.
DNR orders have legal and ethical implications for the patient, the family, and the healthcare team. The patient and the family should understand the benefits and risks of DNR orders and the consequences of changing or revoking them. They should also communicate and document their wishes and preferences clearly and consistently and respect each other’s views and values. The healthcare team should respect and honor the patient’s DNR orders and provide the best possible care for the patient. They should also educate and counsel the patient and the family about DNR orders and help them make informed and appropriate decisions. They should also follow the laws and regulations of their state or country regarding DNR orders and seek legal or ethical advice if they have any doubts or conflicts about DNR orders.
DNR orders are not simple or final decisions but complex and dynamic. They require careful consideration and communication among the patient, the family, and the health care team. They also demand respect and trust among all the parties involved. DNR orders are a legal obligation and a moral responsibility.
Under the law, if a person has a valid DNR order but still receives CPR, they may sue for wrongful life or have the provider charged with battery.
Another common myth about DNR orders is that they are the same as advance directives. This is also not true. Advance directives explain how you want medical decisions about you to be made if you cannot make the decisions yourself. An advance directive can include a living will and a health care power of attorney. A living will tell the healthcare team what treatments you would and would not want to be used to keep you alive, such as CPR, but since these are statements, they are not the same as a medical order. An advance directive is more comprehensive, but considering it is not a medical order, the DNR order has more meaning to healthcare professionals.
An advance directive can help you plan and get the medical care you want at the end of life. It can also help your family and healthcare team understand your wishes and values and avoid confusion or conflict. You or your surrogate can change or revoke an advance directive anytime if you can make decisions. An advance directive is not a mandatory document but a voluntary one. However, it is highly recommended that you have one, especially if you have a severe or chronic illness or if you are older than 18. An advance directive differs from DNR orders and should not be overlooked or ignored.
Another common myth about DNR orders is that they are universally understood. This is also not true. DNR orders are a complex and sensitive topic that can vary depending on the culture and religion of the patient and their family. Different cultures and religions may have different beliefs and values about life, death, and medical interventions. Some cultures and religions may view DNR orders as a sign of respect and dignity, while others may view it as a sign of disrespect and abandonment. Some cultures and religions may accept DNR orders as a personal choice, while others may reject it as violating divine will. Some cultures and religions may have rituals or practices that must be followed before or after the DNR orders are implemented. These differences can affect how the patient and their family understand and communicate about DNR orders and how they interact with the healthcare team.
Since the DNR order is a medical directive, it should incorporate religious and cultural preferences.
DNR orders require cultural and religious diversity and sensitivity from the patient, the family, and the healthcare team. They should all be aware of and respectful of their different perspectives and preferences and avoid making assumptions or judgments based on their views. They should also be open and honest about their expectations and concerns and listen and learn from each other. They should also seek help from cultural or religious experts, such as interpreters, chaplains, or community leaders, if they need guidance or clarification. They should also use clear, straightforward language and avoid medical jargon or acronyms when discussing DNR orders. They should also use visual aids, such as pictures, diagrams, or videos, to explain or demonstrate DNR orders. They should also confirm and repeat the information and ask for feedback to ensure they understand each other correctly. DNR orders are diverse and nuanced and not a universal or straightforward concept.
Another common myth about DNR orders is that they are one-time decisions. This is also not true. DNR orders are a flexible and dynamic decision that can and should be revisited and updated as the patient’s condition and preferences change. The patient or their surrogate has the right and the responsibility to review and revise their DNR orders regularly, especially when they experience a significant change in their health orders, prognosis, goals, or values. For example, a patient may choose to have a DNR order when they have a terminal illness and a poor quality of life, but they may change their mind if they have a chance of recovery or a new treatment option. Conversely, a patient may choose not to have a DNR order when they have a chronic illness and a good quality of life, but they may change their mind if they have a sudden deterioration or a complication. DNR orders are not a fixed or final decision but a continuous and ongoing process.
Revisiting and updating DNR orders can be challenging and stressful for the patient and their family. It can also be confusing and conflicting for the healthcare team. Therefore, it is essential to use shared decision-making and palliative care consultation to facilitate DNR discussions. Shared decision-making is a collaborative approach that involves the patient, the family, and the healthcare team in making informed and respectful decisions about DNR orders and other end-of-life issues. Palliative care consultation is a specialized service that provides expert advice and support on symptom management, communication, and psychosocial and spiritual care for patients with severe or life-limiting illnesses. Shared decision-making and palliative care consultation can help the patient and their family understand the benefits and burdens of DNR orders and other treatments, explore their values and preferences, and reach a consensus consistent with their wishes and best interests. Revisiting and updating DNR orders is not a one-time decision but a repeated and revised one.
A DNR order is a medical order that tells the health care team what to do if your heart stops beating or you stop breathing. It is a crucial decision affecting your quality and length of life. However, many myths and misunderstandings about DNR orders can make it hard to choose what is best for you or your loved one. In this article, we have debunked the top ten myths about DNR orders and shared the facts that can help you make an informed and respectful choice. Here are the main points to remember:
We hope this article has helped you better understand DNR orders and make the best decision for yourself or your loved one. We encourage you to learn more and talk to your healthcare providers about DNR orders and other end-of-life issues. Remember that DNR orders are not a pessimistic choice but a positive and courageous one. It is a way of expressing your wishes and values and respecting your dignity and autonomy. Thank you for reading this article, and we wish you all the best.
The dark side of CPR: Docs say it could be worse than death
Resuscitation is futile in terminally ill patients
CPR and terminal illness: What the public needs to know
CPR’s true survival rate is lower than many people think
Outcomes of In-Hospital CPR: Not as Rosy as Some May Say
CPR on Elderly: Long-term Side Effects of CPR – Potential Complications of CPR – Understanding the Risks – Consequences of Survival After Cardiac Arrest
Psychotherapeutic Considerations for Patients With Terminal Illness (PDF)
CPR Survival Rates – Development and Validation of the Good Outcome Following Attempted Resuscitation (GO-FAR) Score to Predict Neurologically Intact Survival After In-Hospital Cardiopulmonary Resuscitation – Long-Term Outcomes in Elderly Survivors of In-Hospital Cardiac Arrest
Free Advance Directive Forms by State
Living wills and advance directives for medical decisions
Impact of Do-Not-Resuscitate Orders on Nursing Clinical Decision Making (PDF)
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?