Introduction
If you have a loved one who has mixed dementia, you may have many questions and concerns. You may wonder what mixed dementia is, how it affects your loved one, and how you can support them. You may also feel overwhelmed, confused, or scared by the changes you see in your loved one. You are not alone. Many people face the same challenges as you do.
In this article, we will help you understand and care for your loved one with mixed dementia. We will explain what mixed dementia is and how it differs from other types of dementia. We will also share some facts and figures about dementia and mixed dementia. We will tell you why it is essential to know and recognize the signs and symptoms of mixed dementia. We will also guide you through the diagnosis and treatment options for mixed dementia. We will provide tips and strategies for caring for your loved one at home and in the community. We will also suggest some activities and hobbies to make your loved one’s life more enjoyable and meaningful. Finally, we will show you where you can find help and resources for mixed dementia.
We hope that this article will help you and your loved one cope with mixed dementia. We want you to know that you are not alone. Many people and organizations can support you and your loved one. We also want you to know that there is hope. Mixed dementia is not a death sentence. There are ways to manage the symptoms and improve your loved one’s quality of life. You and your loved one can still have a fulfilling and loving relationship.
Let’s begin by learning what mixed dementia is and how it differs from other types of dementia.
What is Mixed Dementia?
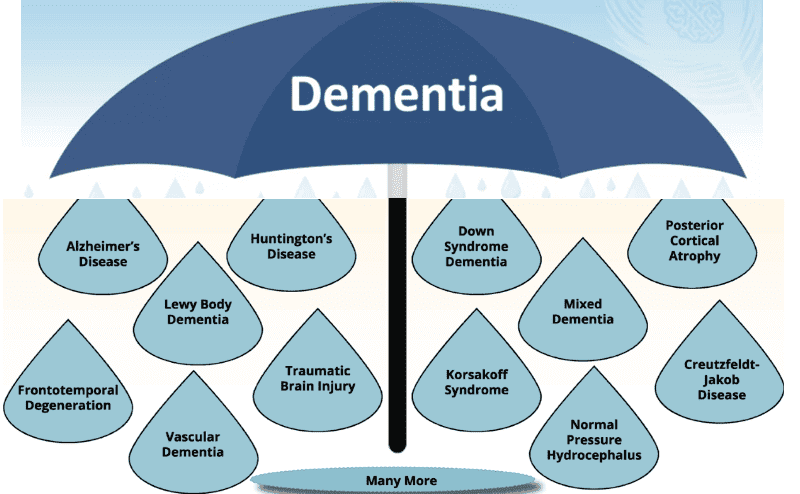
Dementia is a general term for a group of diseases or conditions that affect the brain. Dementia can cause problems with memory, thinking, language, behavior, and mood. There are many types of dementia, such as Alzheimer’s disease, vascular dementia, Lewy body dementia, frontotemporal dementia, and Parkinson’s disease dementia. Each type of dementia has different causes and affects various brain parts.
Mixed dementia is when a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can make it harder for the person to remember things, think clearly, and do everyday tasks. They may also have other problems, depending on the types of dementia they have. For example, they may have trouble with movement, vision, or emotions.
The most common causes of mixed dementia are Alzheimer’s disease and vascular dementia. Alzheimer’s disease is a disease that destroys the brain cells that are responsible for memory and thinking. Vascular dementia is a condition that occurs when the blood vessels that supply oxygen and nutrients to the brain are damaged or blocked. This can cause strokes or mini-strokes that affect various parts of the brain. Other types of dementia that can be involved in mixed dementia are Lewy body dementia, frontotemporal dementia, and Parkinson’s disease dementia. Lewy body dementia is a disease that causes abnormal protein deposits called alpha-synuclein in the brain. These deposits can affect the person’s memory, thinking, behavior, and movement. Frontotemporal dementia is a disease that affects the front and side parts of the brain. These brain parts are involved in personality, language, and behavior. Parkinson’s disease dementia is a condition that occurs when a person with Parkinson’s disease develops dementia. Parkinson’s disease is a disease that affects the nerve cells that control movement.
Mixed dementia is not rare. It is estimated that about 10% to 20% of people with dementia have mixed dementia. However, the exact number is not known because mixed dementia can be hard to diagnose. Some studies suggest that mixed dementia may be more common in older people and people with more severe dementia. Some factors that may increase the risk of mixed dementia are age, family history, genetics, high blood pressure, high cholesterol, diabetes, smoking, and heart disease.
What Observational Changes May Occur in a Loved One with Mixed Dementia?
If your loved one has mixed dementia, you may notice some changes in their memory, thinking, behavior, and mood. These changes may be subtle initially, but they may worsen over time. They may also vary daily or even from hour to hour. These changes may affect your loved one’s ability to do everyday tasks like dressing, cooking, or paying bills. They may also affect your loved one’s relationships, hobbies, and interests.
Some of the common signs and symptoms of mixed dementia are:
- Memory loss: Your loved one may forget recent events, names, faces, appointments, or conversations. They may repeat themselves, ask the same questions, or lose track of time and place. They may also have trouble remembering how to do familiar things, such as using the phone, the remote, or the microwave.
- Language problems: Your loved one may struggle to find the right words or use the wrong words to express themselves. They may also have trouble understanding what others are saying or following instructions. They may mix up languages or speak in a language they learned long ago.
- Reasoning and judgment problems: Your loved one may have trouble making decisions, solving problems, or planning. They may also have difficulty with abstract thinking, such as doing math or understanding jokes or metaphors. They may act impulsively or do inappropriate or risky things, such as giving away money or wandering away from home.
- Personality and behavior changes: Your loved one may act differently than they used to. They may become more irritable, angry, or aggressive. They may also become more apathetic, depressed, or anxious. They may lose interest in things they used to enjoy or show less emotion. They may also develop new habits like hoarding, pacing, or rummaging.
- Mood swings: Your loved one may have sudden changes in their mood, such as going from happy to sad or calm to agitated, without any apparent reason. They may also hallucinate, have delusions, or have paranoia, such as seeing or hearing things that are not there or believing that someone is trying to harm them.
These changes may vary depending on the types and stages of dementia involved in mixed dementia. For example, a person with Alzheimer’s disease and vascular dementia may have more memory loss and confusion than a person with Alzheimer’s disease and Lewy body dementia. A person with Alzheimer’s disease and Lewy body dementia may have more movement and vision problems than a person with Alzheimer’s disease and vascular dementia. A person with Alzheimer’s disease and frontotemporal dementia may have more personality and behavior changes than a person with Alzheimer’s disease and Lewy body dementia. A person with Alzheimer’s disease and Parkinson’s disease dementia may have more tremors and stiffness than a person with Alzheimer’s disease and vascular dementia.
The changes may also vary depending on the stage of dementia. In the early stage, they may be mild and hard to notice. In the middle stage, they may be more noticeable and interfere with daily life. In the late stage, they may be severe and require constant care.
If you notice any changes in your loved one, you should seek medical attention and diagnosis immediately. Mixed dementia can be hard to diagnose, but some tests and scans can help doctors find out what types of dementia your loved one has. Diagnosing can help you and your loved one get the proper treatment and support. It can also help you plan for the future and cope with the changes.
What are the Stages of Mixed Dementia?
Dementia is a progressive disease that worsens over time. It typically follows the stages of dementia, including early-stage dementia, middle-stage dementia, and late-stage dementia. These stages describe how much the symptoms affect a person’s daily life and abilities.
Mixed dementia is a condition where a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can make the symptoms more complex and unpredictable.
To help understand and manage mixed dementia, doctors and caregivers may use staging systems. These are tools that help measure the level of cognitive impairment and functional decline in a person with dementia. There are different staging systems, such as the Global Deterioration Scale (GDS), the Clinical Dementia Rating (CDR), and the Functional Assessment Staging (FAST). Each staging system has its criteria and scales, but they cover the same aspects of dementia, such as memory, language, reasoning, judgment, behavior, and mood.
The Global Deterioration Scale (GDS) is one of the most widely used staging systems for dementia. It consists of seven stages, ranging from 1 (no cognitive decline) to 7 (severe cognitive decline). The GDS is based on the person’s self-reported symptoms and the doctor’s or caregiver’s observations. It helps track the overall progression of dementia and plan the appropriate care and treatment.
The Clinical Dementia Rating (CDR) is another common staging system for dementia. It consists of six stages, ranging from 0 (no dementia) to 5 (severe dementia). The CDR is based on a structured interview with the person and a reliable informant, such as a family member or a friend. The CDR assesses the person’s cognitive and functional abilities in six domains: memory, orientation, judgment, problem-solving, community affairs, home and hobbies, and personal care. The CDR is useful for diagnosing dementia and determining its severity.
Functional Assessment Staging (FAST) is a staging system that focuses on the person’s functional abilities and activities of daily living. It comprises sixteen stages, ranging from 1 (normal adult) to 16 (profound dementia). The FAST is based on the observations of the doctor or caregiver. The FAST evaluates the person’s skills and behaviors in dressing, bathing, eating, toileting, walking, speaking, and socializing. FAST helps identify the specific needs and challenges of the person with dementia and provides the appropriate support and assistance.
Staging systems can have some advantages and limitations for mixed dementia. Some of the advantages are:
- They can help doctors and caregivers better understand the person’s condition and abilities.
- They can help the doctors and caregivers communicate and coordinate the care and treatment more effectively.
- They can help doctors and caregivers monitor the changes and progression of dementia more accurately.
- They can help doctors and caregivers plan for the future and cope with the challenges more realistically.
Some of the limitations are:
- They may not capture the complexity and variability of mixed dementia symptoms and behaviors.
- They may not reflect the individual differences and preferences of the person with dementia and their family.
- They may not account for the effects of other factors, such as medications, comorbidities, environment, and mood, on the person’s cognitive and functional abilities.
- They may not provide a precise or reliable prognosis or outcome for the person with dementia.
The stages of mixed dementia may vary depending on the types and causes of dementia involved. However, some general guidelines and expectations for each stage are:
- Early-stage dementia: The person may have mild memory loss, language problems, reasoning and judgment difficulties, and personality and behavior changes. They may still be able to function independently but may need assistance and reminders for some tasks. They may also benefit from cognitive and social stimulation like puzzles, games, and hobbies.
- Middle-stage dementia: The person may have moderate memory loss, language problems, reasoning and judgment difficulties, and personality and behavior changes. They may also have mood swings, hallucinations, delusions, or paranoia. They may need more assistance and supervision for most tasks, such as dressing, cooking, or paying bills. They may also benefit from physical and emotional support, such as exercise, music, and massage.
- Late-stage dementia: The person may have severe memory loss, language problems, reasoning and judgment difficulties, and personality and behavior changes. They may also have movement and vision problems, incontinence, and infections. They may need constant care and attention for all tasks, such as eating, bathing, or toileting. They may also benefit from comfort and dignity care, such as pain relief, hygiene, and palliative care.
How Does Mixed Dementia Affect the Person and Their Family?
Mixed dementia is a condition in which a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can cause various symptoms and challenges for the person and their family.
Mixed dementia can affect a person’s memory, thinking, behavior, mood, and physical health. Some of the symptoms and challenges of mixed dementia are:
- Memory loss: The person may forget recent events, names, faces, appointments, or conversations. They may also have trouble remembering how to do familiar things, such as using the phone, the remote, or the microwave.
- Language problems: People may struggle to find the right words or use the wrong words to express themselves. They may also have trouble understanding what others are saying or following instructions.
- Reasoning and judgment problems: The person may have trouble making decisions, solving problems, or planning. They may also have difficulty with abstract thinking, such as doing math or understanding jokes or metaphors.
- Personality and behavior changes: The person may act differently than they used to. They may become more irritable, angry, or aggressive. They may also become more apathetic, depressed, or anxious. They may lose interest in things they used to enjoy or show less emotion. They may also develop new habits like hoarding, pacing, or rummaging.
- Mood swings: The person may have sudden changes in their mood, such as going from happy to sad or calm to agitated, without any apparent reason. They may also have hallucinations, delusions, or paranoia, such as seeing or hearing things that are not there or believing that someone is trying to harm them.
- Movement and vision problems: The person may have movement problems, such as walking, balance, or coordination. They may also have trouble with vision, such as seeing double, blurry, or distorted images.
- Physical health problems: The person may have other health problems, such as high blood pressure, high cholesterol, diabetes, heart disease, stroke, or infection. They may also have trouble eating, swallowing, sleeping, or breathing.
These symptoms and challenges can greatly impact the person’s daily life and abilities. They may need more assistance and supervision for most tasks, such as dressing, cooking, or paying bills. They may also need more medical care and treatment for their condition. The changes they experience may make them feel frustrated, confused, or scared. They may also feel isolated, lonely, or hopeless.
Mixed dementia can also affect the family and caregivers of the person. They may face emotional and practical difficulties, such as:
- Emotional difficulties: The family and caregivers may feel sad, angry, or guilty about the person’s condition. They may also feel stressed, overwhelmed, or exhausted by the demands of caring for the person. They may have trouble coping with the person’s mood swings, behavior changes, or hallucinations. They may also worry about the person’s safety, health, or future.
- Practical difficulties: The family and caregivers may have to change their lifestyle, work, or finances to care for the person. They may have to spend more time, money, or energy on the person’s needs, such as medical appointments, medications, or equipment. They may also have to deal with legal, financial, or medical issues, such as power of attorney, wills, or insurance. They may also have to seek help and support, such as home care, respite care, or support groups.
These difficulties can affect the well-being and relationships of the family and caregivers. They may feel depressed, anxious, or burned out. They may also feel lonely, isolated, or unsupported. They may have less time, energy, or interest in their hobbies, interests, or social life.
Mixed dementia can be hard to understand and manage for the person and their family. But there are ways to help them live better. In the next sections, we will talk about how mixed dementia can be diagnosed and treated and how you can support your loved one with mixed dementia.
How Can Mixed Dementia Be Diagnosed and Treated?
Mixed dementia is a condition in which a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can cause various symptoms and challenges for the person and their family.
To diagnose mixed dementia, the doctor will ask the person and their family about their medical history, symptoms, and lifestyle. The doctor will also do a physical exam and some tests to check the person’s cognitive and functional abilities. These tests may include:
- Memory and thinking tests measure a person’s memory, language, reasoning, judgment, and other mental skills. They may involve answering questions, naming objects, drawing shapes, or following instructions. The doctor may use standardized tests, such as the Mini-Mental State Examination (MMSE) or the Montreal Cognitive Assessment (MoCA), or informal tests, such as asking the person to recall the date or the president’s and prime minister’s names.
- Blood tests: These are tests that check the person’s blood for any signs of infection, inflammation, vitamin deficiency, thyroid problems, or other conditions that may affect the brain. They may also check the person’s blood sugar, cholesterol, and blood pressure levels, which may indicate the risk of vascular dementia.
- Brain scans: These tests take pictures of the person’s brain using machines, such as magnetic resonance imaging (MRI) or computed tomography (CT). They can show the brain’s size, shape, and structure and reveal any damage, bleeding, or blockage in the blood vessels. They can also show the presence of abnormal protein deposits, such as amyloid plaques or Lewy bodies, which are linked to Alzheimer’s disease and Lewy body dementia.
Diagnosing mixed dementia can be hard because the symptoms may overlap or change over time. Sometimes, the doctor may not know that a person has mixed dementia until they look at their brain after they die. However, some tests and scans can help the doctor determine what types of dementia a person has. Diagnosing can help the person and their family get the right treatment and support. It can also help them plan for the future and cope with the changes.
There is no cure for mixed dementia, but there are ways to treat the symptoms and slow down the progression of the disease. The treatment may depend on the types and causes of dementia involved in mixed dementia. Some of the medicines and treatments that may help are:
- Cholinesterase inhibitors: These drugs increase the level of a chemical called acetylcholine in the brain. This chemical helps the brain cells communicate with each other. These drugs may help with memory, thinking, and behavior problems in people with Alzheimer’s disease and Lewy body dementia. Some examples of these drugs are donepezil, rivastigmine, and galantamine. Please be aware that if these medications are not stopped when the person reaches the latter stages of the disease, the loved one with mixed dementia may exhibit extreme paranoia, agitation, and combative behaviors, including becoming physically violent, increased anxiety, continuing crying spells, and have grave discomfort as these medications are only meant for the early to middle stages of the disease.
- Memantine: This drug blocks the action of a glutamate chemical in the brain. This chemical can damage the brain cells when it is too high. This drug may help with memory, thinking, and behavior problems in people with moderate to severe Alzheimer’s disease. It may also help with vascular dementia and Lewy body dementia. It can be used alone or with a cholinesterase inhibitor. Please be aware that if these medications are not stopped when the person reaches the latter stages of the disease, the loved one with mixed dementia may exhibit extreme paranoia, agitation, and combative behaviors, including becoming physically violent, increased anxiety, including crying spells, and have grave discomfort as these medications are only meant for the early to middle stages of the disease.
- Antipsychotics: These are drugs that affect the level of a chemical called dopamine in the brain. This chemical helps the brain control movement and emotions. These drugs may help with hallucinations, delusions, paranoia, or aggression in people with Lewy body dementia or Alzheimer’s disease. However, these drugs can also cause serious side effects, such as an increased risk of stroke, infection, or death. They should be used with caution and only when necessary. Some examples of these drugs are risperidone, quetiapine, and olanzapine.
- Antidepressants: These are drugs that affect the level of chemicals called serotonin and norepinephrine in the brain. These chemicals help the brain regulate mood and emotions. These drugs may help with depression, anxiety, or apathy in people with mixed dementia. Some examples of these drugs are citalopram, sertraline, and venlafaxine.
- Blood pressure and cholesterol-lowering drugs: These lower the person’s blood pressure and cholesterol levels. These levels may affect the health of the blood vessels and the blood flow to the brain. These drugs may help prevent or reduce the risk of strokes or mini-strokes, which can cause vascular dementia. Some examples of these drugs are lisinopril, atorvastatin, and clopidogrel. Please be aware that science shows the actual absolute risk reduction of statin medications for reducing all forms of mortality is only 0.8%, not the falsely elevated via using the relative risk reduction numbers, and that statins can induce dementia or make dementia worse in addition to the side effects of pre-diabetes or worsening diabetes, muscle pain and tendon rupture.
In addition to medicines, other treatments can help the person with mixed dementia. These include:
- Cognitive stimulation and rehabilitation: These activities stimulate and train the person’s memory, thinking, and other mental skills. They may involve puzzles, games, exercises, or tasks that challenge the person’s brain. They may also involve strategies and techniques that help the person cope with cognitive difficulties, such as calendars, lists, or reminders. These activities may help the person maintain or improve their cognitive abilities and quality of life.
- Physical therapy and exercise: These activities improve the person’s physical health and fitness. They may involve exercises, stretches, or massages that help the person with movement, balance, or coordination. They may also involve aerobic exercises, such as walking, cycling, or swimming, which help the person with blood circulation and oxygen supply to the brain. These activities may help the person prevent or reduce the risk of falls, injuries, or infections, which can worsen dementia.
- Occupational therapy and assistive devices: These services and tools help people with daily tasks and activities. They may involve an occupational therapist who assesses the person’s needs and abilities and provides guidance and training on doing things safely and independently. They may also involve assistive devices, such as walkers, canes, or wheelchairs, which help the person with mobility and stability. These services and tools may help the person maintain or improve their functional abilities and quality of life.
It is important for the person with mixed dementia to have regular check-ups and monitoring of their condition. The doctor may adjust the dose or type of medicines and treatments based on the person’s symptoms and response. The doctor may also check for any side effects or complications of the medicines and treatments. The doctor may also recommend other tests or scans to track the changes and progression of dementia. Regular check-ups and monitoring can help the person and their family manage mixed dementia better and plan for the future.
How Can You Support a Loved One with Mixed Dementia?
Mixed dementia is a condition in which a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can cause various symptoms and challenges for the person and their family.
If you have a loved one with mixed dementia, you may wonder how you can support them. You may want to help them maintain their dignity, independence, and quality of life. You may also want them to feel loved, valued, and respected. You may also want to take care of yourself and your well-being. Here are some tips and strategies that may help you and your loved one with mixed dementia:
- Caring for a person with mixed dementia at home and in the community: You may want to create a safe, comfortable, and familiar environment for your loved one at home. You may want to remove any potential hazards, such as sharp objects, slippery floors, or loose wires. You may also want to install locks, alarms, or sensors to prevent wandering or accidents. You may want to label the rooms, doors, drawers, or cabinets to help your loved one find their way around. You may also want to use clocks, calendars, or photos to help your loved one remember the time, date, or people. You may want to involve your loved one in simple household chores, such as folding clothes, setting the table, or watering the plants. You may also want to encourage your loved one to go out and socialize with others, such as family, friends, neighbors, or community members. You may want to accompany your loved one to places they enjoy, such as parks, libraries, or cafes. You may also want to join support groups or programs that cater to people with dementia and their families, such as dementia cafes, memory clubs, or respite care.
- Communicating, interacting, and engaging with a person with mixed dementia: You may want to communicate clearly and respectfully with your loved one. You may want to use short sentences, simple words, and gestures. You may also want to avoid jargon, slang, or metaphors. You may want to speak slowly, calmly, and gently. You may also want to use a positive and friendly tone. You may want to maintain eye contact, smile, and nod. You may also want to touch, hug, or hold hands. You may want to listen attentively, patiently, and empathetically. You may also want to acknowledge, validate, and reassure. You may want to avoid arguing, correcting, or criticizing. You may also want to avoid asking too many questions or questions that test their memory or logic. You may want to interact with your loved one meaningfully and enjoyably. You may want to use their name and remind them of who you are and how you are related. You may also want to discuss their past, interests, or preferences. You may want to engage your loved one in activities stimulating and enriching their life. You may want to choose activities that suit their abilities, needs, and moods. You may also want to vary the activities to keep them interested and motivated. You may want to do activities that involve music, art, games, puzzles, or crafts. You may also want to do activities that involve nature, animals, or children.
- Planning for the future and coping with changes: You may want to plan for the future and cope with the changes that mixed dementia may bring. You may want to discuss their wishes, preferences, and values with your loved one. You may also want to involve them in making decisions about their care and treatment if they can. You may want to consult their doctor, lawyer, or financial advisor about their medical, legal, or financial matters. You may also want to prepare the necessary documents, such as a will, power of attorney, or an advance directive. You may want to cope with the changes that mixed dementia may bring. You may want to accept that your loved one may not be the same as they used to be. You may also want to adapt to their changing needs and abilities. You may want to seek help and support from others, such as family, friends, professionals, or organizations. You may also want to take care of yourself and your well-being. You may want to eat, sleep, exercise, and relax often. You may also want to pursue hobbies, interests, or social life.
Where Can You Find Help and Resources for Mixed Dementia?
Mixed dementia is a condition in which a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can cause various symptoms and challenges for the person and their family.
If you have a loved one with mixed dementia, you may need help and resources to understand and manage the condition. You may also need help and resources to care for yourself and your well-being. Fortunately, many sources and organizations offer information, guidance, and support for mixed dementia. Some of them are:
- The Alzheimer’s Association: This is a national organization that provides reliable information, education, referral, and support to millions of people affected by Alzheimer’s disease and other types of dementia, including mixed dementia.
- The National Institute on Aging (NIA): This federal agency conducts and supports research on aging and health, including Alzheimer’s disease and other types of dementia, including mixed dementia.
- The Lewy Body Dementia Association (LBDA) is a national organization that provides information, education, advocacy, and support to people affected by Lewy body dementia, one of the types of dementia that can be involved in mixed dementia. You can visit their website to learn more about Lewy body dementia, find a support group, or join their online forum.
- The Association for Frontotemporal Degeneration (AFTD) is a national organization that provides information, education, advocacy, and support to people affected by frontotemporal degeneration, one of the types of dementia that can be involved in mixed dementia. You can visit their website to learn about frontotemporal degeneration, find a support group, or join their online community.
- The Parkinson’s Foundation: This is a national organization that provides information, education, research, and support to people affected by Parkinson’s disease, a condition that can cause dementia and can be involved in mixed dementia. You can visit their website to learn more about Parkinson’s disease and dementia, find a support group, or join their online forum.
These are just some sources and organizations offering help and resources for mixed dementia. You can find many more online or in your local area. We encourage you to seek help and join support networks for mixed dementia. You are not alone. Many people and organizations can support you and your loved one. You can also help others by sharing your experiences and insights with mixed dementia. Together, we can make a difference.
End-of-Life Planning and Hospice for Mixed Dementia
Mixed dementia is a condition in which a person has more than one type of dementia at the same time. This means that their brain is affected by different diseases or conditions that damage the brain cells. For example, a person may have Alzheimer’s disease and vascular dementia or Alzheimer’s disease and Lewy body dementia. Mixed dementia can cause various symptoms and challenges for the person and their family.
As mixed dementia progresses, the person may reach the final stage of the disease, where they may need more intensive and specialized care. This is the time to consider end-of-life planning and hospice for mixed dementia. End-of-life planning is discussing and documenting the person’s wishes, preferences, and values regarding their care and treatment at the end of life. Hospice focuses on bringing comfort, self-respect, and peace to the person and their family in the last months, weeks, or days of life.
End-of-life planning and hospice for mixed dementia can help the person and their family prepare for the inevitable and cope with the changes. They can also help the person and their family receive the best care and support matching their needs and goals. Here are some tips and strategies for end-of-life planning and hospice for mixed dementia:
- Start the conversation early: It is important to start the conversation about end-of-life planning and hospice as soon as possible after a diagnosis of mixed dementia. This can help the person and their family express their wishes and make informed decisions while the person can still communicate and participate. It can also help the person and their family avoid conflicts, confusion, or regrets later. The person, family, doctor, or care team can initiate the conversation. The conversation can be ongoing and revisited as the person’s condition changes.
- Complete the legal documents: As part of end-of-life planning, the person and their family should complete the legal documents that enable them to document their preferences and appoint someone to make decisions for them if they cannot. These documents include a living will, a health care power of attorney, a do-not-resuscitate (DNR) order, and an advance directive. These documents can help the person and their family ensure their wishes are respected and followed by the health care team and the hospice staff. They can also help the person and their family avoid unwanted or unnecessary treatments or interventions that may cause more harm than good.
- Seek the signs and symptoms: To be eligible for hospice, the person with mixed dementia must have a life expectancy of six months or less, as determined by their doctor. This can be hard to predict, especially for mixed dementia, as the symptoms and progression may vary depending on the types and causes of dementia involved. However, there are some signs and symptoms that may indicate that the person is nearing the end of life, such as:
- Severe memory loss, confusion, or disorientation
- Difficulty recognizing familiar people, places, or objects
- Loss of speech or communication
- Difficulty swallowing, eating, or drinking
- Weight loss, dehydration, or malnutrition
- Infections, such as pneumonia or urinary tract infection
- Fever, pain, or discomfort
- Breathing problems, such as shortness of breath or congestion
- Skin problems, such as pressure ulcers or bruises
- Sleep problems, such as insomnia or excessive sleeping
- Withdrawal, apathy, or depression
- Agitation, restlessness, or delirium
- Changes in vital signs, such as blood pressure, pulse, or temperature
If the person shows signs and symptoms, the family or the care team should consult the doctor and ask about hospice eligibility and referral. The doctor may comprehensively assess the person’s condition and prognosis and determine if hospice is appropriate and beneficial for them and their family.
- Choose the hospice provider: Once the person is eligible and referred for hospice, the family or the care team should choose the one that best suits their needs and preferences. Several hospice providers exist, such as home, inpatient, or hospice in a long-term care facility. The family or the care team should consider the following factors when choosing the hospice provider:
- The location, accessibility, and availability of the hospice provider
- The services, programs, and resources offered by the hospice provider
- The quality, experience, and reputation of the hospice provider
- The cost, coverage, and payment options of the hospice provider
- The compatibility, communication, and coordination of the hospice provider with the person, their family, and their care team
The family or the care team should interview and compare different hospice providers and ask questions such as:- How long have you been providing hospice care for people with mixed dementia?
- What are the qualifications and training of your hospice staff?
- How do you assess and manage the symptoms and needs of people with mixed dementia?
- How do you communicate and collaborate with the person, family, and care team?
- How do you respect and honor the wishes and values of people with mixed dementia and their family?
- How do you support the emotional and spiritual needs of people with mixed dementia and their family?
- How do you handle emergencies or complications that may arise?
- How do you measure and ensure the quality and satisfaction of your hospice care?
The family or the care team should choose the hospice provider with whom they feel comfortable and confident and who can provide the best possible care and support for the person and their family.
- Receive hospice care: Once the hospice provider is chosen, the person and their family should receive the care they need and deserve. Hospice care focuses on bringing comfort, self-respect, and peace to the person and their family in the last months, weeks, or days of life. Hospice care is provided by professionals and volunteers, such as doctors, nurses, social workers, counselors, chaplains, and aides. Hospice care may include the following services and supports:
- Medical care and treatment that aim to relieve the pain and symptoms of mixed dementia and other conditions, such as medications, oxygen, or equipment
- Personal care and assistance that help the person with their daily activities, such as bathing, dressing, feeding, or toileting
- Emotional and spiritual care and counseling that help the person and their family cope with the emotional and spiritual issues and challenges of mixed dementia and end of life, such as grief, loss, or faith
- Social and recreational care and activities that help the person and their family enjoy and celebrate their life and relationships, such as music, art, games, or visits
- Practical and legal care and guidance that help the person and their family deal with the practical and legal matters and arrangements of mixed dementia and end of life, such as finances, insurance, or funeral
- Bereavement care and support that help the family cope with the grief and loss of their loved one after their death, such as follow-up calls, visits, or groups
Hospice care is not a one-size-fits-all approach. Hospice care is tailored to the individual needs and preferences of the person and their family. Hospice care is flexible and adaptable to the changing needs and preferences of the person and their family. Hospice care is respectful and compassionate to the wishes and values of the person and their family.
Hospice Care for Your Loved One with Dementia
If you are caring for a loved one with dementia, you may have heard of hospice care, but you may not know what it is or when it is appropriate. Hospice care is a special type that focuses on providing comfort and support to people with life-limiting illnesses and their families. It does not aim to cure the disease but to ease the symptoms and improve the quality of life in the final stages.
Hospice care can benefit people with dementia and their families in many ways. It can help manage the pain, agitation, and distress common in advanced dementia. Hospice care can also provide emotional and spiritual support to the person with dementia and their loved ones and practical assistance with daily tasks and caregiving. Depending on the patient’s and family’s needs and preferences, hospice care can be provided at home, in a hospice facility, or a nursing home.
Hospice care is available to people with a life expectancy of six months or less, as determined by a physician. However, this does not mean hospice care will end after six months. Hospice care can continue if the person meets the eligibility criteria and the family wishes to receive it. For people with dementia, the eligibility criteria may include experiencing multiple physical and mental declines, such as losing weight, having difficulty swallowing, being bedridden, or having severe cognitive impairment. Hospice care may also be appropriate for people with dementia who require frequent nursing care or who have recurrent infections that are hard to treat or prevent.
Signs and Symptoms that Indicate Hospice Care May Be Appropriate for Someone with Dementia
Dementia is a progressive disease that affects the brain and causes memory loss, confusion, and behavioral changes. There are different types and stages of dementia, but one of the most common and severe forms is Alzheimer’s disease. Alzheimer’s disease can be measured by the FAST Scale, which stands for Functional Assessment Staging. The FAST Scale has seven stages, from 1 to 7, that describe the functional decline of people with Alzheimer’s disease. Stage 7 is the most advanced, indicating that the person may benefit from hospice care.
Some of the signs and symptoms that are typical of stage 7 on the FAST Scale are:
- Incontinence: People who need diapers or pads cannot control their bladder or bowel movements.
- Inability to communicate: The person cannot speak or understand language and may only make sounds or gestures.
- Loss of all intelligible vocabulary: The person cannot say any words that make sense and may only repeat sounds or phrases.
Another sign that hospice care may be appropriate for someone with dementia is severe cognitive impairment. This means that the person has no awareness of self, environment, or time and cannot recognize familiar people or objects. The person may not respond to their name, not know where they are or what day it is, and may not remember their spouse, children, or friends. The person may also hallucinate, have delusions or paranoia, and may become agitated or aggressive.
Other signs and symptoms that indicate hospice care may be appropriate for someone with dementia are recurrent infections and difficulty swallowing, eating, or drinking. Recurrent infections, such as pneumonia, urinary tract infections, or sepsis, are common in people with advanced dementia, and they can be life-threatening or cause complications. Difficulty swallowing, eating, or drinking can lead to weight loss, dehydration, or malnutrition and can also increase the risk of choking or aspiration. These conditions can affect the person’s comfort and well-being and may require hospice care to manage them.
Pain, agitation, or distress are also signs and symptoms that indicate hospice care may be appropriate for someone with dementia. Pain can be caused by various factors, such as infections, injuries, pressure ulcers, or arthritis, and it can be hard to detect or measure in people with dementia, who may not be able to express or report it. Agitation or distress can be caused by cognitive impairment, environmental factors, or unmet needs, and they can manifest as restlessness, anxiety, anger, or depression. Pain, agitation, or distress can affect the person’s quality of life and comfort and may require hospice care to relieve them with medication or other interventions.
The Importance of Hospice Care for People with Dementia and Their Families
Hospice care can make a difference for people with dementia and their families in the final stages of the disease. Hospice care can help improve the person’s comfort and dignity and reduce their suffering and stress. Hospice care can also help the family cope with the emotional and practical challenges of caring for a loved one with dementia and provide them with guidance and support. Hospice care can help the family prepare for the end of life and the grief process and offer them bereavement services after the death of their loved one.
If you think that hospice care may be right for your loved one with dementia, you should talk to your physician and hospice team about your options and preferences. They can help you determine the eligibility and availability of hospice care and explain the benefits and services that hospice care can provide. They can also help you find and select a hospice provider that meets your needs and expectations.
There are many resources and contact information that you can use to learn more about hospice care and find a hospice provider near you. Some of them are:
Hospice care can be a valuable option for your loved one with dementia and your family. Hospice care can help you make the most of the time you have left with your loved one and provide you with comfort and support. Hospice care can help you honor your loved one’s wishes and values and celebrate their life and legacy. Hospice care can help you say goodbye to your loved one with peace and grace.
Conclusion
In this article, we have learned about mixed dementia, a condition where a person has more than one type of dementia at the same time. We have explained what mixed dementia is, how it affects the person and their family, how it can be diagnosed and treated, and how you can support your loved one with mixed dementia. We have also shared some sources and organizations that offer help and resources for mixed dementia.
We hope that this article has helped you understand and care for your loved one with mixed dementia. We want you to know that you are not alone. Many people and organizations can support you and your loved one. We also want you to know that there is hope. Mixed dementia is not a death sentence. There are ways to manage the symptoms and improve the quality of life of your loved one. You and your loved one can still have a fulfilling and loving relationship.
We encourage you to seek help and join support networks for mixed dementia. You can also help others by sharing your experiences and insights with mixed dementia. Together, we can make a difference.
Resources
A Complete Guide to Mixed Dementia: What You Need to Know
Mixed Dementia | Symptoms & Treatments
What is Mixed Dementia? Symptoms, Causes, Diagnosis and Treatment
End-of-Life Planning from the Alzheimer’s Association
End-of-Life Care for People With Dementia
Development of a Dementia-Focused End-of-Life Planning Tool: The LEAD Guide (Life-Planning in Early Alzheimer’s and Dementia)
Trivia Games – Caregiver Activities for Alzheimer’s and Dementia
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
The 36-Hour Day: A Family Guide to Caring for People Who Have Alzheimer’s Disease and Other Dementias
Caregiver Support Book Series
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Holistic Nurse: Skills for Excellence book series
The Validation Breakthrough: Simple Techniques for Communicating with People with ‘Alzheimer’s-Type Dementia’
Dementia Home Care: How to Prepare Before, During, and After
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Fading Reflection: Understanding the complexities of Dementia
Dementia Caregiving: A Self Help Book for Dementia Caregivers Offering Practical Coping Strategies and Support to Overcome Burnout, Increase Awareness, and Build Mental & Emotional Resilience
Navigating the Dementia Journey: A Compassionate Guide to Understanding, Supporting, and Living With Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Caregiver Support Book Series
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
My Loved One with Dementia
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
The Validation Breakthrough: Simple Techniques for Communicating with People with Alzheimer’s Disease and Other Dementias
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
How Do I Know You? Dementia at the End of Life
The Dementia Caregiver: A Guide to Caring for Someone with Alzheimer’s Disease and Other Neurocognitive Disorders (Guides to Caregiving)
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
The Caregiver’s Guide to Dementia: Practical Advice for Caring for Yourself and Your Loved One (Caregiver’s Guides)
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare