DNR and the Terminally Ill
Published on June 7, 2020
Updated on September 7, 2024
Published on June 7, 2020
Updated on September 7, 2024
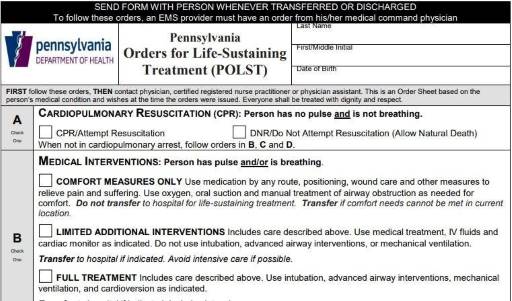
Table of Contents
Navigating conversations about Do Not Resuscitate (DNR) orders with terminally ill patients and their families can be challenging yet crucial for ensuring that the patient’s wishes and comfort are prioritized. Choosing between DNR or full code often involves delicate emotions, medical considerations, and ethical concerns. This article will delve into a methodology that has proven effective in facilitating these discussions, particularly in hospice care. Drawing from years of experience and successful outcomes, we’ll explore approaches prioritizing compassion, clarity, and patient-centered care. Additionally, we’ll reference valuable resources to enhance understanding and guide these critical conversations.
Before discussing DNR, it’s essential to establish a foundational understanding of hospice care. This involves emphasizing that hospice focuses on comfort, peace, and quality of life rather than curative treatments or frequent hospital visits.
Each patient’s situation is unique, so tailoring the conversation accordingly is vital. Use the patient’s primary diagnosis to guide the discussion, ensuring relevance and clarity. For instance, you might say, “When [patient’s name], the [terminal disease], takes your life, would you prefer to remain comfortable and allow a natural passing?”
Simplify the information instead of inundating patients and families with statistics about CPR success rates in different settings. Explain that while CPR aims to restart the heart and breathing, it doesn’t cure the underlying terminal illness. Highlighting this can help set realistic expectations without causing unnecessary fear or confusion.
If patients or families hesitate or express uncertainty, provide reassurance and additional information. Discuss potential scenarios, such as the physical toll of CPR or the possibility of ending up on life support, to help them make an informed decision.
Recognize that these decisions are deeply personal and may require time for reflection. Provide patients and families with the opportunity to revisit and revise their choices as needed, ensuring that their wishes align with their values and comfort levels.
Discussing DNR orders with terminally ill patients and their families requires a compassionate, tailored approach that prioritizes clarity, empathy, and patient-centered care. By starting with a clear understanding of hospice’s focus on comfort and peace, tailoring conversations to individual needs, simplifying complex information, addressing concerns, and allowing time for reflection, healthcare providers can guide these discussions effectively. This methodology, grounded in experience and successful outcomes, honors patients’ wishes while ensuring compassionate end-of-life care.
Pennsylvania Orders for Life-Sustaining Treatment (POLST)
https://www.kevinmd.com/blog/2016/07/family-said-everything.html
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death