The Hidden Costs of Hospice Fraud: Protecting Patients and Families
Published on December 26, 2025
Updated on December 21, 2025
Published on December 26, 2025
Updated on December 21, 2025
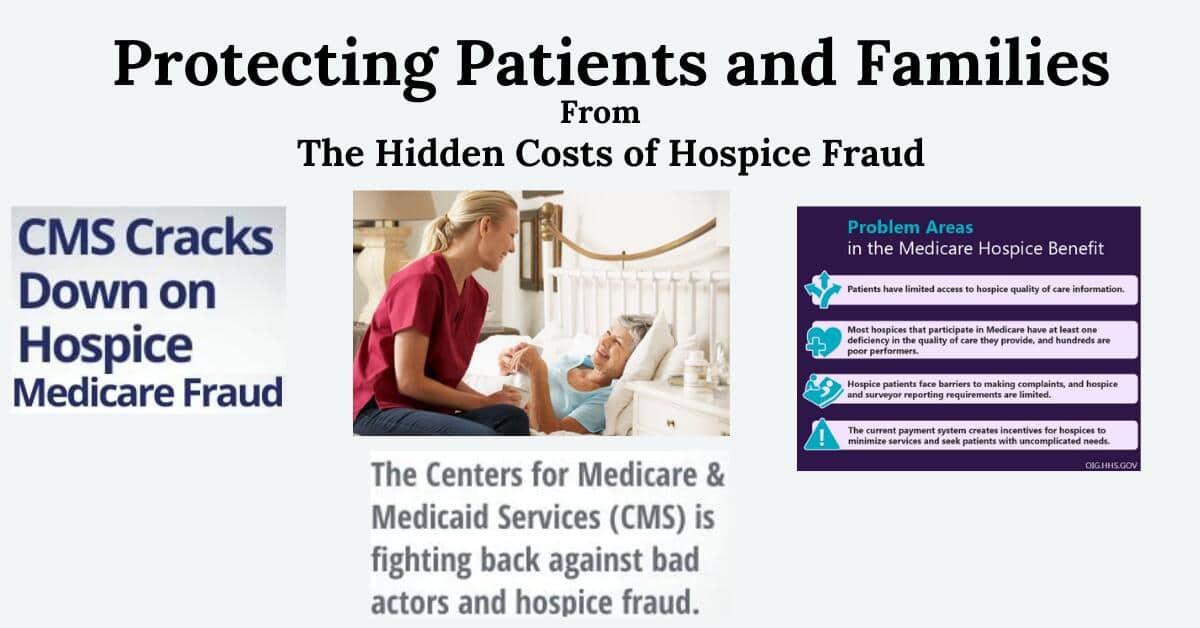
Table of Contents
Hospice care is a compassionate approach designed to support individuals facing life-limiting illnesses. It focuses on providing comfort, dignity, and quality of life during the final stages of life. Unlike traditional medical care, hospice care does not aim to cure the illness but rather to manage symptoms and provide emotional, spiritual, and social support to patients and their families.
Importance of Hospice Care:
While hospice care is vital, it is not immune to fraudulent activities. Hospice fraud involves unethical practices such as billing for services not rendered, enrolling ineligible patients, and overcharging for services. These actions can have devastating impacts on patients and their families, leading to inadequate care, financial burdens, and emotional distress.
Common Types of Hospice Fraud:
This article aims to:
Hospice care is an essential service that provides comfort and dignity to individuals nearing the end of life. However, hospice fraud can undermine the quality of care and trust in the system. This article will guide you in understanding hospice care, recognizing the impacts of fraud, and making informed decisions when choosing a reliable hospice provider.
Hospice fraud occurs when healthcare providers use unethical practices to exploit the hospice care system, often for financial gain. This can lead to significant harm to patients and their families, both emotionally and financially. Here, we will explore the main types of hospice fraud and their implications.
Hospice providers may bill for services that were never rendered to the patient. This fraudulent activity can take several forms:
Implications:
Some hospice providers may enroll patients who do not meet the eligibility criteria for hospice care, which typically requires a prognosis of six months or less to live if the illness runs its normal course. This can happen through:
Implications:
Overcharging involves billing for more expensive services than those provided or needed. This can include:
Implications:
Recent Examples of Hospice Fraud Cases
Hospice fraud is not just a theoretical issue; real-world examples highlight its prevalence and impact.
Statistical Data on the Prevalence of Hospice Fraud
Statistics provide a clearer picture of the extent of hospice fraud and its impact on the healthcare system.
| Type of Fraud | Description | Implications |
|---|---|---|
| Billing for Services Not Provided | Charging for visits or care that never occurred. | Patients miss out on needed care, causing a financial burden on families and a loss of trust. |
| Enrolling Ineligible Patients | Certifying non-terminal patients as eligible for hospice care. | Deprivation of curative treatments, misleading families, resource misallocation. |
| Overcharging for Services | Billing for more expensive or unnecessary services. | The financial strain on families, legal consequences, and misallocation of resources. |
Understanding hospice fraud is crucial for protecting patients and ensuring they receive the compassionate care they deserve. By recognizing the different types of fraud and their implications, patients, caregivers, and families can be better prepared to choose trustworthy hospice providers and advocate for ethical practices in end-of-life care.
Hospice fraud can have profound and far-reaching impacts on terminally ill patients. These effects are not just limited to financial aspects but also emotional, psychological, and physical well-being. Understanding these impacts can help patients and their families navigate this challenging time with greater awareness and preparedness.
Increased Stress and Anxiety
Fraudulent hospice practices can significantly elevate stress and anxiety levels for terminally ill patients. When patients discover that the care they are receiving is not genuine or that they have been misled, it can lead to:
Loss of Trust in Healthcare Providers
Trust is a cornerstone of effective healthcare. Hospice fraud can severely damage this trust, leading to:
| Effect | Description | Implications |
|---|---|---|
| Increased Stress and Anxiety | Elevated worry and emotional distress due to unreliable care. | Heightened worry, emotional distress, feelings of betrayal and vulnerability. |
| Loss of Trust in Healthcare Providers | Damage to the fundamental trust between patients and providers. | Skepticism, reluctance to seek help, difficulty in establishing trust. |
Inadequate Pain Management
One of the primary goals of hospice care is to manage pain effectively. Fraudulent practices can lead to inadequate pain management, resulting in:
Poor Quality of Care
Hospice fraud often means patients do not receive the necessary care. This can manifest in various ways:
| Consequence | Description | Implications |
|---|---|---|
| Inadequate Pain Management | Failure to provide proper pain relief and symptom control. | Uncontrolled pain, reduced quality of life, unnecessary suffering. |
| Poor Quality of Care | Neglect of essential care services and substandard treatment. | Neglect, substandard treatment, and diminished overall care quality. |
Out-of-Pocket Expenses for Non-Existent Services
Hospice fraud can impose significant financial burdens on patients and their families. When billed for services that were never provided:
Legal Costs Associated with Fraud Cases
Pursuing legal action against fraudulent hospice providers can be costly and time-consuming:
| Financial Burden | Description | Implications |
|---|---|---|
| Out-of-Pocket Expenses for Non-Existent Services | Charges for services that were never provided, leading to unexpected costs. | Unexpected costs, financial strain, unjustified medical bills. |
| Legal Costs Associated with Fraud Cases | Expenses related to pursuing legal action against fraudulent providers. | Legal fees, emotional toll, and time-consuming legal processes. |
Hospice fraud has severe impacts on terminally ill patients, affecting their emotional, psychological, physical, and financial well-being. By understanding these potential consequences, patients and their families can better prepare and take proactive steps to ensure they receive the genuine and compassionate care they deserve.
Hospice fraud affects patients, caregivers, and family members. It can have emotional, financial, and ethical impacts, making an already challenging situation even more difficult.
Grief Compounded by Betrayal and Mistrust
The emotional weight of caring for a terminally ill loved one is immense. When hospice fraud is involved, this burden is compounded by feelings of betrayal and mistrust.
The Strain on Family Relationships
Caring for a terminally ill family member is already stressful, and hospice fraud can exacerbate this strain.
| Emotional Impact | Description | Implications |
|---|---|---|
| Grief Compounded by Betrayal and Mistrust | Feelings of betrayal and mistrust due to fraudulent practices. | Emotional distress, difficulty trusting new providers, compounded grief. |
| The Strain on Family Relationships | Increased stress and conflict among family members. | Family conflicts, strained relationships, emotional exhaustion. |
Financial Losses Due to Fraudulent Billing
Hospice fraud can lead to significant financial losses for families. Fraudulent billing practices can drain financial resources and create unexpected expenses.
Costs of Seeking Alternative Care
When fraud is discovered, families often need to find alternative care providers, which can be costly.
| Financial Impact | Description | Implications |
|---|---|---|
| Financial Losses Due to Fraudulent Billing | Unexpected bills for non-existent or unnecessary services. | Depleted savings, financial strain, unexpected expenses. |
| Costs of Seeking Alternative Care | Expenses related to finding and transitioning to a new care provider. | Transition costs, higher fees, and the additional financial burden. |
Navigating Legal Systems to Address Fraud
Addressing hospice fraud often involves navigating complex legal systems, which can overwhelm families.
Ethical Dilemmas in End-of-Life Care
Hospice fraud can create ethical dilemmas for families trying to ensure their loved ones receive appropriate care.
| Legal and Ethical Concerns | Description | Implications |
|---|---|---|
| Navigating Legal Systems to Address Fraud | The complexity and cost of legal action against fraudulent providers. | Legal fees, time-consuming processes, added stress. |
| Ethical Dilemmas in End-of-Life Care | Moral and ethical conflicts in ensuring appropriate care. | Moral distress, complicated decision-making, ethical conflicts. |
Hospice fraud has severe and multifaceted impacts on caregivers and families, affecting them emotionally, financially, and ethically. By understanding these impacts, families can better prepare for and navigate the challenges of fraudulent hospice practices, ensuring their loved ones receive the compassionate and ethical care they deserve.
Government and regulatory bodies are crucial in ensuring that hospice care providers operate ethically and legally. They enforce laws and regulations designed to protect patients and maintain the integrity of healthcare services. Understanding these laws and the efforts to enforce them can help patients, caregivers, and families make informed decisions and advocate for quality care.
Anti-Kickback Statute
The Anti-Kickback Statute (AKS) is a federal law that prohibits the exchange of remuneration (anything of value) for referrals of services or items covered by federal healthcare programs, such as Medicare and Medicaid.
Physician Self-Referral Law (Stark Law)
The Stark Law prohibits physicians from referring patients to receive designated health services (DHS) payable by Medicare or Medicaid from entities with which the physician or an immediate family member has a financial relationship unless an exception applies.
Physician Payments Sunshine Act
The Physician Payments Sunshine Act requires manufacturers of drugs, medical devices, and biologicals participating in federal healthcare programs to report payments and other value transfers to physicians and teaching hospitals.
| Law | Purpose | Prohibited Actions | Penalties |
|---|---|---|---|
| Anti-Kickback Statute (AKS) | Prevent financial incentives from compromising care quality. | Offering, paying, soliciting, or receiving kickbacks for patient referrals. | Fines, imprisonment, exclusion from federal healthcare programs. |
| Physician Self-Referral Law (Stark Law) | Prevent conflicts of interest and overutilization of services. | Referring patients to entities with which the physician has a financial relationship. | Fines, exclusion from federal healthcare programs. |
| Physician Payments Sunshine Act | Increase transparency in financial relationships between providers and the industry. | Failing to report payments and other transfers of value to physicians and teaching hospitals. | Significant fines for non-compliance. |
Recent Enforcement Actions: Government agencies, including the Department of Justice (DOJ), the Office of Inspector General (OIG), and the Centers for Medicare & Medicaid Services (CMS), actively enforce healthcare fraud and abuse laws. Recent enforcement actions highlight the ongoing efforts to combat hospice fraud.
Challenges in Regulation and Enforcement. Despite these efforts, regulating and enforcing hospice fraud laws present several challenges:
| Enforcement Effort | Description | Challenges |
|---|---|---|
| Recent Enforcement Actions | Actions taken by DOJ, OIG, and CMS to combat hospice fraud. | The complexity of fraud schemes, resource limitations, and evolving tactics. |
| Case Example 1 | Hospice and home health agencies paid over $1.8 million for improper payments. | Detecting sophisticated fraud activities. |
| Case Example 2 | Houston-area doctors paid $1.8 million for submitting medically unnecessary claims. | Limited resources for comprehensive investigations. |
The role of government and regulatory bodies in combating hospice fraud is vital to protecting patients and ensuring the integrity of hospice care. Understanding existing laws and regulations, as well as the challenges of enforcement, can help patients, caregivers, and families navigate the healthcare system more effectively and advocate for ethical care practices.
Selecting a reliable hospice provider is crucial to ensuring that terminally ill patients receive compassionate and ethical care. Here are some tips to help you make an informed decision.
Checking Licenses and Certifications
One of the first steps in choosing a trustworthy hospice provider is to verify their licenses and certifications.
Reading Reviews and Testimonials
Reviews and testimonials from other patients and families can provide valuable insights into the quality of care provided.
| Step | Description | Importance |
|---|---|---|
| Checking Licenses and Certifications | Verify state licenses and accreditations from reputable organizations. | Ensures the provider meets regulatory and quality standards. |
| Reading Reviews and Testimonials | Look for online reviews, testimonials, and word-of-mouth recommendations. | Provides insights into the provider’s quality of care and patient experiences. |
Inquiries About Staff Qualifications and Training
Understanding the qualifications and training of the hospice staff is essential for ensuring high-quality care.
Questions on Care Plans and Patient Monitoring
A comprehensive care plan and effective patient monitoring are critical components of quality hospice care.
| Question | Description | Importance |
|---|---|---|
| Staff Qualifications and Training | Ask about the credentials and ongoing training of hospice staff. | Ensures that staff are well-qualified and up-to-date with best practices. |
| Care Plans and Patient Monitoring | Inquire about how care plans are developed and how patients are monitored. | Ensures that care is personalized and symptoms are effectively managed. |
Unclear Billing Practices
Transparency in billing is essential to avoid unexpected costs and ensure that you are not being overcharged.
Lack of Transparency in Services Offered
A trustworthy hospice provider should be transparent about the services they offer and how they deliver care.
| Red Flag | Description | Implications |
|---|---|---|
| Unclear Billing Practices | Lack of detailed billing statements and unclear billing policies. | This may indicate the potential for overcharging and unexpected costs. |
| Lack of Transparency in Services Offered | Vague descriptions of services and unclear availability of staff. | This may indicate poor quality of care and inadequate support for patients. |
Choosing a trustworthy hospice provider involves thorough research, asking the right questions, and being vigilant for red flags. By checking licenses and certifications, reading reviews, inquiring about staff qualifications and care plans, and ensuring transparency in billing and services, you can make an informed decision that ensures your loved one receives the compassionate and ethical care they deserve.
Empowering patients and families involves equipping them with the knowledge and resources to navigate hospice care with confidence and effectiveness. Understanding legal rights, reporting fraud, and accessing support systems are crucial.
Understanding Patient Rights
Patients receiving hospice care have specific rights that ensure they receive respectful, ethical, and high-quality care. These rights are protected by federal and state laws and are designed to safeguard the well-being of patients and their families.
Key Patient Rights Include:
| Patient Right | Description | Importance |
|---|---|---|
| Informed Consent | Right to receive all necessary information to make informed decisions. | Ensures patients understand the risks and benefits of treatments. |
| Right to Refuse Treatment | Right to refuse any treatment and be informed of the consequences. | Empower patients to make choices about their care. |
| Confidentiality | Right to privacy regarding medical, social, and financial information. | Protects patient privacy and dignity. |
| Participation in Care Planning | Right to be involved in developing and modifying the care plan. | Ensures care is tailored to the patient’s needs and preferences. |
| Grievance Procedures | Right to voice grievances and suggest changes without fear of reprisal. | Provides a mechanism for addressing concerns and improving care quality. |
Resources for Reporting Fraud: If you suspect hospice fraud, you must report it to the appropriate authorities to protect yourself and others from unethical practices.
Steps to Report Fraud:
| Resource | Contact Information | Purpose |
|---|---|---|
| Office of Inspector General (OIG) Hotline | Call 1-800-447-8477 or submit an online complaint. | Report fraud, waste, and abuse in Medicare and Medicaid programs. |
| Senior Medicare Patrol (SMP) Resource Center | Call 877-808-2468 or visit their website. | Report hospice fraud and receive guidance on preventing Medicare fraud. |
Counseling and Support Groups for Affected Families. Emotional support is crucial for families dealing with the challenges of hospice care and the potential impact of fraud. Counseling and support groups can provide a safe space to share experiences and receive emotional support.
Types of Support Available:
Benefits of Support Systems:
Financial and Legal Assistance Programs. Navigating the financial and legal aspects of hospice care can be overwhelming, especially when dealing with fraud. Various programs and resources are available to assist.
Types of Assistance Available:
How to Access Assistance:
| Support System | Description | Benefits |
|---|---|---|
| Individual Counseling | One-on-one sessions with a licensed therapist. | Provides personal emotional support and coping strategies. |
| Family Counseling | Sessions involving family members to address collective concerns. | Improves family dynamics and collective coping. |
| Support Groups | Group meetings are held to share experiences and receive support. | It fosters a sense of community and reduces isolation. |
| Financial Assistance Programs | Programs to help cover the costs of hospice care. | Reduces financial burden and ensures access to necessary care. |
| Legal Aid Services | Legal advice and representation for hospice-related issues. | Provides legal support and helps navigate complex legal matters. |
| Non-Profit Organizations | Organizations offering financial and legal support to families. | Provides additional resources and support tailored to hospice care needs. |
Empowering patients and families involves understanding legal rights, reporting fraud, and accessing support systems. By being informed and proactive, families can ensure their loved ones receive the compassionate, ethical care they deserve and navigate the challenges of hospice care with confidence and support.
As you navigate the challenging journey of hospice care, being informed and vigilant can make a significant difference in ensuring your loved one receives the compassionate and ethical care they deserve. Let’s summarize the key points discussed and reflect on the importance of making informed decisions.
Understanding Hospice Fraud
Hospice fraud can have devastating impacts on terminally ill patients and their families. Recognizing the different types of fraud, such as billing for services not provided, enrolling ineligible patients, and overcharging for services, is crucial for protecting your loved ones.
Impact on Terminally Ill Patients: The emotional, psychological, physical, and financial toll of hospice fraud on patients can be severe. From increased stress and anxiety to inadequate pain management and unexpected financial burdens, the consequences are far-reaching.
Impact on Caregivers and Families. Caregivers and families also suffer from the effects of hospice fraud. Emotional distress, financial losses, and legal and ethical dilemmas can add to the already challenging task of caring for a terminally ill loved one.
Government and Regulatory Bodies: Government and regulatory bodies play a vital role in combating hospice fraud through laws such as the Anti-Kickback Statute, Stark Law, and the Physician Payments Sunshine Act. Despite the challenges in enforcement, recent actions highlight ongoing efforts to protect patients.
Tips for Choosing a Trustworthy Hospice Provider: Selecting a reliable hospice provider involves thorough research, asking the right questions, and being vigilant for red flags. Checking licenses and certifications, reading reviews, inquiring about staff qualifications, and ensuring transparency in billing and services are essential steps.
Empowering Patients and Families: Understanding patient rights, knowing how to report fraud, and accessing support systems can empower patients and families. Counseling, support groups, financial assistance programs, and legal aid services provide the necessary support to navigate hospice care confidently.
| Topic | Key Points | Importance |
|---|---|---|
| Understanding Hospice Fraud | Recognize types of fraud and their impacts. | Protects patients from unethical practices. |
| Impact on Terminally Ill Patients | Emotional, psychological, physical, and financial toll of fraud. | Ensures awareness of potential consequences. |
| Impact on Caregivers and Families | Emotional distress, financial losses, legal and ethical dilemmas. | Highlights the broader impact of fraud. |
| The Role of Government and Regulatory Bodies | Laws and enforcement efforts to combat hospice fraud. | Provides a framework for legal protection. |
| Tips for Choosing a Trustworthy Hospice Provider | Research, ask questions, and watch for red flags. | Ensures informed decision-making for quality care. |
| Empowering Patients and Families | Understand rights, report fraud, and access support systems. | Provides tools and resources for navigating hospice care. |
Choosing hospice care for a loved one is a deeply personal and often difficult decision. Ensuring ethical, compassionate, and high-quality care requires vigilance and informed decision-making. Here are some final thoughts to keep in mind:
By staying informed, vigilant, and proactive, you can ensure your loved one receives compassionate, ethical care during their final days. Remember, you are not alone in this journey—support and resources are available to help you every step of the way.
| Final Thought | Description | Importance |
|---|---|---|
| Stay Informed | Knowledge about hospice care and potential risks. | Empowers better decision-making. |
| Be Vigilant | Watch for red flags and ask questions. | Ensures transparency and quality care. |
| Advocate for Your Loved One | Speak up and address concerns. | Improves the quality of care and safeguards patient rights. |
| Seek Support | Utilize counseling, support groups, and other resources. | Provides emotional and practical assistance. |
| Trust Your Instincts | Follow your intuition if something feels off. | Guides you in making the right decisions for your loved one. |
In conclusion, navigating hospice care requires knowledge, vigilance, and support. By understanding potential risks, advocating for your loved one, and using available resources, you can ensure they receive the compassionate, ethical care they deserve. Remember, you can make a difference in their final journey.
CMS Cracks Down on Hospice Medicare Fraud
OIG Submit a Hotline Complaint
Office of Inspector General (OIG) – What problems has OIG identified with the hospice program?
Bereaved Families Face ‘Devastating’ Impacts of Hospice Fraud
One at Large, Another Facing 10-Year Sentence in California $30M Hospice Fraud Scheme
Dying or Lying? For-Profit Hospices and End of Life Care
Hospice and the False Claims Act: Paradoxes in End-of-Life Care
“Dueling” Experts and the False Claims Act: Weaponizing Legal Falsity to Combat Hospice Fraud
Healthcare Fraud and the Erosion of Trust
Hospice Fraud: Predicting Ability and Intent
Hospice fraud: The Betrayal of Trust: Investigating Hospice Fraud Cases
How Hospice Became a For-Profit Hustle
Beneficiaries Pay the Price for Hospice Fraud
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series