Tag: Restlessness
Articles about managing restlessness including terminal restlessness in the terminally ill.
Articles about managing restlessness including terminal restlessness in the terminally ill.

This comprehensive guide provides essential insights into recognizing and addressing delirium in terminally ill individuals. It’s an invaluable resource for nurses, caregivers, and families, offering practical advice and empathetic support.
Discover how oral ketamine is emerging as a game-changer in palliative care, offering rapid relief for severe depression, anxiety, and emotional distress. This comprehensive guide explores its potential benefits, administration methods, and important considerations for patients and healthcare providers.

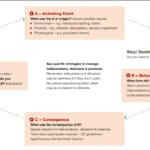
Discover effective strategies for managing end-of-life crises in hospice care. Learn how to recognize signs of distress, implement calming techniques, and provide compassionate support to patients and families. This guide offers practical tips for hospice nurses and caregivers to navigate challenging situations with confidence and empathy.
Learn effective strategies for managing hallucinations in terminally ill patients. This guide covers pharmacological and non-pharmacological methods to improve comfort and quality of life.

Caring for a loved one with dementia can be both rewarding and challenging. If your loved one has been restless throughout their life, this restlessness may continue as a symptom of their dementia. As an experienced hospice nurse, I understand the difficulties you may face in managing habitual restlessness while ensuring the safety and welfare of your loved one. In this article, I'll provide you with practical tips and evidence-based practices to create a calming environment for your loved one, even if they have trouble with fine motor control due to arthritis or other factors.

Losing a loved one is an incredibly challenging experience, and witnessing changes in their behavior and well-being can be distressing. As a hospice nurse, I've supported many families and caregivers through this grim time. One common symptom that may arise towards the end of life is restlessness. In this article, I will explain the different types of restlessness and offer guidance on how to manage them. Understanding these distinctions can provide valuable insights into your loved one's condition and help you navigate the final stages of their life with compassion and care.

One of the hardest portions of the job of a hospice nurse is to identify when a patient has two weeks of life left to live; this can be especially difficult at facilities going through staffing shortages leading to inconsistent caregivers with little to verbally report on a patient’s change of condition. Since being aware of the velocity of declines is extremely important, let’s cover an area that we in hospice (nurses, families, and caregivers alike) can keep an eye on in terms of identifying terminal restlessness which is often a key indicator for one week or less of life.

Dementia is a progressive brain disorder that affects a person’s cognitive abilities, memory, and behavior. In the later stages of the disease, some patients can become combative and aggressive, making it difficult for caregivers to provide the necessary care. As a hospice nurse, it’s important to know how to approach and manage combative dementia patients to ensure their comfort and safety. Here are some best practices to consider:

Guide to Recognize and Treat Common End of Life Symptoms provides tips on managing symptoms experienced by those at the end of their lives - Topics such as pain, shortness of breath, respiratory distress, and anxiety, and provides suggestions for medications and complementary therapies to help manage these symptoms.
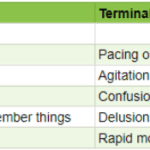
As an experienced hospice nurse, I understand how difficult it can be to distinguish between delirium and terminal restlessness. Both conditions can cause significant distress for the patient and their loved ones, and nurses must be able to tell the difference between them to provide the best possible care. In this article, I will share my knowledge and experience to help new hospice nurses understand the differences between delirium and terminal restlessness and how to rule out delirium.

Terminal restlessness is a common phenomenon that occurs in the final stages of life. It is characterized by agitation, confusion, and distress. It can be challenging to recognize and manage, especially in patients who cannot communicate verbally. This article aims to share insights and tips from a hospice worker who learned how terminal restlessness can manifest differently in nonverbal patients and how to cope.

Naomi Feil is an expert in gerontology and the creator of validation therapy, which is a means of communicating and acknowledging the internal reality of patients with dementia. When properly utilized, validation therapy can enhance the quality of life of patients with dementia as well as reduce stress on the family and caregivers.
While Naomi Feil and her followers (of which the writer of this article may be considered one, at least in form) focus on using this method of communication to maintain health with the potential for a level of restorative health, I want to share how the concepts of this method can be used during times of crisis.

Navigating the final days of a loved one's life can be a challenging and emotional journey. One of the signs that can be observed during this time is known as terminal restlessness. As someone deeply rooted in hospice care, I have witnessed various manifestations of this restlessness. Understanding its types, causes, and management strategies is crucial for providing compassionate end-of-life care. This article aims to illuminate the different kinds of terminal restlessness, identify reversible causes, and discuss effective management techniques. By equipping caregivers, families, and healthcare professionals with this knowledge, we can ensure that terminally ill individuals experience comfort and dignity in their final days.