Tag: Hospice Care
Articles about hospice care including how to manage comfort at end of life.
Articles about hospice care including how to manage comfort at end of life.
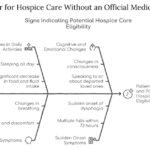
This article aims to provide information and guidance on qualifying for hospice care without an official medical diagnosis. We will explain hospice care, how to access it without a physician’s consent, what to expect, and how to make the most of it.

Hospice care focuses on comfort rather than curative treatments. In emergencies, calling 911 can lead to invasive procedures and disrupt hospice care. This article explores why contacting your hospice provider first is crucial and offers guidance on alternatives to calling 911.

If you are caring for a loved one with pulmonary fibrosis, you may have many questions and concerns about their condition and how to support them best. You may also feel overwhelmed, stressed, or isolated by the challenges and responsibilities of caregiving. You are not alone. Many people face similar situations and emotions when caring for someone with chronic and progressive lung disease.
This article will help you understand pulmonary fibrosis and how it affects your loved one and yourself. It will also provide practical and helpful information on providing the best care for your loved one and yourself.
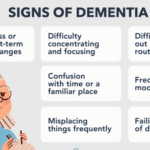
Learn to recognize early dementia signs and explore care options, including hospice. This guide offers insights into dementia, practical care tips, and when to seek professional help.

Caring for a loved one with dementia in rural areas can be challenging when local care facility options are limited. This guide explores alternatives, such as contacting organizations like the Alzheimer's Association, considering different facility types (adult day care, long-term care, respite care, memory care), seeking financial assistance, evaluating hospice eligibility, and assessing life plan/continuing care communities. It also addresses the legal and ethical implications of using hospitals as a last resort.

Emergency admissions in hospice provide rapid care for patients nearing the end of life. This process involves quick referrals, expedited assessments, and immediate provision of necessary equipment and medications. Hospice teams work efficiently to ensure patients receive comfort and support during this critical time.
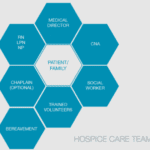
Hospice care is about providing compassionate support and comfort to patients during their end-of-life journey. Interdisciplinary Group (IDG) meetings ensure the highest quality care for hospice patients and their families. These meetings bring together a diverse team of professionals to discuss patient care plans, address concerns, and collaborate on providing holistic support. However, these meetings can sometimes become overwhelming and time-consuming. Let's explore some best practices to make the most of IDG meetings while keeping patient-centered care at the forefront.
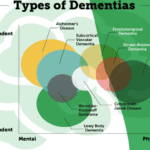
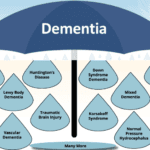
This article summarizes the twelve known types of dementia, which are the most common and well-studied forms of this condition. You will learn about the signs and symptoms of each type, how they are diagnosed, what causes them, and how they are treated. This article is intended for family members and caregivers of people with dementia who may want to understand more about the condition and how to support their loved ones.
Explore the complex world of dementia-related aggression and learn how to identify its underlying causes. This comprehensive guide offers insights into medication-related issues, pain management, and non-pharmacological interventions. Discover compassionate care strategies to support patients and caregivers on this challenging journey.
Hospice care focuses on comfort, not curing illness. But what if an emergency arises? This guide explains when hospice covers emergency care, how to proceed, and how hospice services continue during/after hospitalization - ensuring you make informed decisions without losing benefits.

This article provides a compassionate guide for families and caregivers of individuals with dementia. It aims to offer insight into the progression of dementia and how to recognize when it may be time to consider hospice care. This article seeks to empower you with knowledge and understanding so you can make informed decisions that honor the dignity and comfort of your loved one.
This article is like a flashlight in the dark. It’s here to shine a light on the path ahead, even when we don’t have all the answers. We’ll talk about how dementia can affect people differently and share some common signs that can help you guess what stage your loved one might be in.

Discover the unsung heroes of hospice care: primary caregivers. From family members to trained professionals, these compassionate individuals provide essential support to patients nearing the end of life. Learn about their crucial roles, challenges, and their impact in ensuring comfort and dignity for hospice patients.
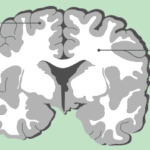
Discover the essentials of white matter disease, its impact on brain health, and how to support affected loved ones. This comprehensive guide offers insights into symptoms, diagnosis, treatment options, and practical tips for caregivers, empowering families to navigate this challenging condition with knowledge and compassion.
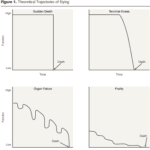
Have you ever wondered how different illnesses affect our lives and deaths? How do we cope with the uncertainty and unpredictability of our health? How do we plan for our future and make the best decisions for ourselves and our loved ones?
In this article, we will summarize and discuss the main points and findings of the paper and explore how they relate to our own lives and deaths. We will also provide practical and actionable suggestions for you to cope with and plan for your and your loved ones’ trajectories. We aim to help you understand the different types of illness trajectories, how they affect our lives and deaths, and how we can prepare for them.

Dementia is a complex and challenging condition that affects millions of individuals, often requiring specialized care. When it comes to supporting a loved one with dementia, understanding the types of healthcare providers available is essential. Each specialist brings a unique set of skills and expertise to the table. In this article, we will delve into the various types of healthcare providers for dementia and help you understand when to consider one specialist over another.
Discover the truth behind the myth that medications can keep terminally ill patients alive indefinitely. This article explores the psychological factors behind this belief and its consequences while providing compassionate strategies to cope with the reality of losing a loved one while ensuring quality end-of-life care.

Medications like anticoagulants, antidepressants, and NSAIDs can cause harm to hospice patients. Learn how to balance comfort and safety with individualized care.
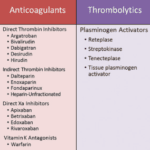
Anticoagulants can prevent blood clots but also cause bleeding risks for terminally ill patients. This article explains why these medications should be regularly reviewed for deprescribing, outlining factors like prognosis, preferences, and palliative care options to consider when making informed, compassionate choices aligned with the patient's goals.

This article discusses the importance of quarterly medication reconciliation for terminal patients and their families. It explains the benefits, such as improving patient safety, quality of life, symptom management, and the challenges and solutions. It also addresses the need to re-evaluate certain medications, like donepezil and memantine, for patients with dementia as their disease progresses.
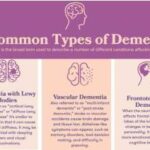
Explore the five most common types of dementia: Alzheimer's, Vascular, Lewy Body, Frontotemporal, and Mixed. Learn about their unique characteristics, symptoms, and progression. Understanding these differences is crucial for proper diagnosis, treatment, and care of individuals affected by dementia.
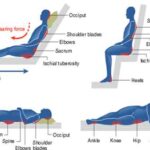
This guide provides practical strategies for preventing and managing pressure injuries in terminally ill patients. Learn how to assess risk, optimize nutrition, reposition properly, choose support surfaces, and care for the skin. Get recommendations for home, hospice, and hospital settings, as well as pain management and infection control. Empower yourself with evidence-based tips to improve your loved one's comfort and quality of life.

Delve into the world of blood-based biomarkers for dementia detection. This article examines the science behind these tests, their potential to revolutionize early diagnosis, and the complex ethical considerations surrounding their use. Discover how these tests might shape the future of Alzheimer's care and research.
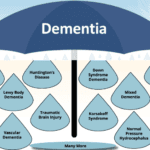
Mixed dementia combines symptoms of multiple types of dementia, presenting unique challenges for patients and caregivers. This article explores the complexities of mixed dementia, its symptoms, diagnosis, and treatment options. Learn practical tips for providing compassionate care and support to loved ones affected by this condition.