Tag: Hospice Care
Articles about hospice care including how to manage comfort at end of life.
Articles about hospice care including how to manage comfort at end of life.

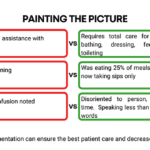
Recognizing the velocity of changes in a patient's condition is crucial for hospice nurses. By understanding the pace of changes in vital signs, symptoms, functionality, and more, nurses can anticipate needs, adjust care plans, and communicate the prognosis effectively with patients and families. The article provides guidelines on interpreting the velocity to estimate the time a patient has left.

This article offers guidance for new visiting hospice nurses struggling with work-life balance. It covers strategies like maintaining a recertification journal, pre-charting before visits, assessing end-of-life status, educating families, and preparing for a "good death." By following these tips, nurses can take less work home while delivering focused, compassionate care.

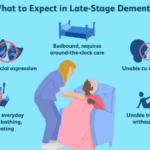
Dementia is a progressive brain disorder that affects a person’s cognitive abilities, memory, and behavior. In the later stages of the disease, some patients can become combative and aggressive, making it difficult for caregivers to provide the necessary care. As a hospice nurse, it’s important to know how to approach and manage combative dementia patients to ensure their comfort and safety. Here are some best practices to consider:

As an experienced hospice nurse, I understand that working in hospice care can be emotionally and physically challenging. In this presentation, I will share my knowledge and expertise on the topics of death and dying, as well as comfort medications including morphine, to help guide you in providing the best care for your patients.
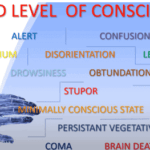
Understanding drowsiness, lethargy, and obtundation is crucial in hospice care. Drowsiness is a normal sleepiness, lethargy is more profound tiredness, and obtundation indicates severe unresponsiveness. Recognizing these levels helps in providing the right care and comfort for terminally ill patients.

Guide to Recognize and Treat Common End of Life Symptoms provides tips on managing symptoms experienced by those at the end of their lives - Topics such as pain, shortness of breath, respiratory distress, and anxiety, and provides suggestions for medications and complementary therapies to help manage these symptoms.

I have worked with countless terminally ill patients and their families. One of the most important aspects of hospice care is ensuring that the patient and their loved ones are prepared for the end of life.
In this article, I will cover the topics that hospice nurses should discuss with patients and caregivers to ensure a good death.
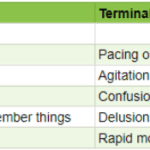
As an experienced hospice nurse, I understand how difficult it can be to distinguish between delirium and terminal restlessness. Both conditions can cause significant distress for the patient and their loved ones, and nurses must be able to tell the difference between them to provide the best possible care. In this article, I will share my knowledge and experience to help new hospice nurses understand the differences between delirium and terminal restlessness and how to rule out delirium.
Explore the ethical dilemma of physical therapy for terminally ill dementia patients. This article examines the potential harm of aggressive interventions, highlighting the importance of comfort-focused care. Learn why hospice professionals often advocate for gentler approaches in end-of-life dementia care.
Hospice care is focused on symptom management, pain relief, emotional support, and spiritual care. It is a privilege to be a part of a patient’s end-of-life journey, and as a new hospice nurse, you may feel overwhelmed, but you can make a difference in a patient’s life. One of the essential skills you need to learn as a hospice nurse is to recognize when to increase the scheduled visit frequency for a terminally ill patient under hospice care.
I keep the bedside documentation to under 15 minutes (admission visits not included) by creating muscle memory by following consistent templates based on the type of visit (routine, PRN, recertification, death, and admission).
I’ve previously shared my recertification template, so let me share my routine visit template for today. For those new, routine visits are scheduled ahead of time, and while you may arrive to find a crisis before you, the visit itself was scheduled and therefore considered routine. It is regarded as part of the four hospice care levels according to Medicare guidelines.

Our primary focus for our patients is comfort at the end of life as hospice nurses. We work tirelessly to ensure that our patients receive the best possible care during their end-of-life journey. An aspect of that care that is often overlooked, but incredibly important is timely documentation.
Documenting hospice visits at the bedside is crucial for several reasons. Not only does it help ensure that our patients are receiving the best possible care, but it also helps the hospice team as a whole and reduces issues when the caregiver must be involved in triage services. Here are just a few reasons why documenting hospice visits at the bedside is so important:
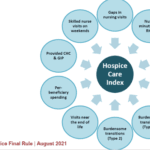
As an experienced hospice nurse, I understand how overwhelming and emotional it can be for terminally ill patients and their loved ones to navigate the hospice process. Hospice care is a compassionate and comprehensive approach to end-of-life care, designed to provide comfort, pain management, and emotional support to patients and their families. However, many people have questions about hospice eligibility and hospice recertification. In this article, I will provide a generalized guide to help you understand these important aspects of hospice care.
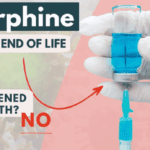
As a hospice nurse with years of experience, I have encountered many situations where family members are hesitant to allow their loved ones to receive medications such as morphine and lorazepam. One of the main reasons for this hesitancy is the belief that these medications will hasten death, leading to euthanasia.
In this article, I want to address this concern and help family members and friends understand the use of morphine and lorazepam in hospice care.

I’ve seen firsthand how important it is to understand comfort and discomfort in hospice care. Let’s dive into these terms and how they relate to end-of-life care.

Hospice comfort medications play a vital role in managing end-of-life symptoms. From morphine for pain and breathing difficulties to lorazepam for anxiety and restlessness, these medications are carefully administered to enhance quality of life while ensuring patient comfort and dignity.
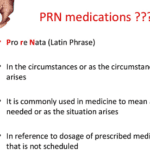
Hey there, my friend! As an experienced hospice nurse, I understand that managing symptoms for comfort is crucial for terminally ill patients. One of the ways we do this is through PRN medications. Today, I want to help you understand PRN medications and how they can be used in conjunction with scheduled medications.

Hospice care offers a specialized service known as the Continuous Care Benefit. This unique care type provides crucial 24-hour support to patients who are going through an acute symptom crisis. In this article, we'll delve into what Continuous Care Benefit is, who's eligible for it, how it operates, why it's important, how to access it, and its duration.
Understanding Hospice Care: A Guide for Families
If you or your loved one is facing a serious illness and needs extra care and support, hospice care may be the right choice. Hospice is a special kind of care that helps people who are nearing the end of their lives feel as comfortable and peaceful as possible.

I remember having some nurses tell me that nurses who go into hospice lose their critical thinking skills because they are dealing with people who are dying. Little did they know that hospice nurses often need to think far more critically than other nurses. Let’s outline some key critical thinking areas as a hospice nurse.

Terminal restlessness is a common phenomenon that occurs in the final stages of life. It is characterized by agitation, confusion, and distress. It can be challenging to recognize and manage, especially in patients who cannot communicate verbally. This article aims to share insights and tips from a hospice worker who learned how terminal restlessness can manifest differently in nonverbal patients and how to cope.
When a loved one is diagnosed with a terminal illness, hospice care can provide comfort and dignity in their final days. Hospice care is a type of palliative care that focuses on relieving pain and symptoms rather than curing the disease. It also offers emotional and spiritual support to the patient and their family.
However, choosing a hospice agency is not easy. Many factors must be considered, such as the quality of care, the agency's location, the level of services, and the patient’s rights. This article will discuss these factors and provide tips on choosing the best hospice agency for your loved one.

Hospice care focuses on providing comfort and quality of life for people with terminal illnesses and life expectancies of six months or less. While hospice care can be a difficult decision for families, it can also be a source of support and relief during a challenging time. In this article, we will explain the process of getting your loved one into hospice care and answer some common questions.
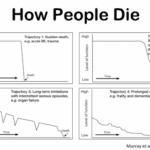
Admitting a patient to hospice services is a complex and sensitive process that requires careful assessment and communication. One of the challenges that hospice nurses face is to determine if the patient is close to the transitioning phase of dying, which is the final stage of life when death is imminent. This phase usually lasts for one to two weeks, and it is essential to prepare the family and provide a plan for increased hospice involvement during this time. However, on admission, hospice nurses do not have the luxury of having visited with the patient over the past several weeks to months to observe the changes that often signal that death is approaching. Therefore, they need to rely on other indicators to help them identify whether the patient is transitioning.