Tag: Hospice Care
Articles about hospice care including how to manage comfort at end of life.
Articles about hospice care including how to manage comfort at end of life.

An article that guides families through understanding and exercising their rights to choose the best hospice care for their loved ones, ensuring their final chapter is written with compassion and respect.

Discover gentle methods to encourage dementia patients to bathe. Learn how to create a positive bathing experience, use distraction techniques, and maintain a consistent routine. These compassionate approaches help caregivers navigate hygiene challenges while preserving dignity and reducing stress for both patient and caregiver.
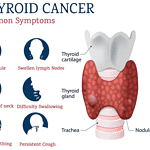
Thyroid cancer presents challenges not just for patients, but also for their families. My role is to be your guide, as a dedicated hospice registered nurse case manager, throughout the various stages of this disease. I'm here to equip you with the essential knowledge needed to provide compassionate care for your loved one. In this article, we will delve into what you should anticipate during the course of thyroid cancer, how to identify changes in your loved one's condition, and how to offer optimal care from the initial diagnosis to the end-of-life journey.

Welcome to our discussion on a topic close to many hearts: the care of our loved ones with dementia. When a family member is diagnosed with dementia, it feels like a part of them slowly fades away. But as they lose parts of themselves, your role in their life becomes even more crucial. This article isn’t just words on a page; it’s a beacon of hope and understanding, shining a light on why your voice, as a family member, is vital in the care of your loved one.

Welcome to our guide on hospice care for undocumented immigrants. This article is crafted with the utmost empathy to support family members and caregivers as they navigate the complexities of end-of-life care. Our goal is to provide a clear understanding of hospice services and the unique challenges faced by undocumented immigrants during these tender moments.

When caring for a loved one with dementia, it's important to approach their needs with empathy and understanding. Dementia is a progressive condition that affects memory, thinking, and communication. As a caregiver or family member, it's crucial to adapt your communication style and strategies to best support your loved one. This article will guide you through the stages of dementia, address common symptoms like anxiety and agitation, provide techniques to reduce caregiver burnout, create a calm environment, and effectively respond to repetitive questions.
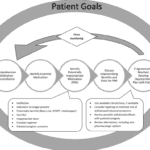
In the world of healthcare, when a provider writes an order to "Eval and Treat" for hospice, they are asking for a thorough evaluation and a tailored treatment plan. This is specifically meant for patients who are being considered for hospice care. Let's delve into what this means and why it's crucial.
What Does "Eval and Treat" for Hospice Mean?

Dealing with a loved one's diagnosis of pancreatic cancer can feel overwhelming but remember that you are not alone in this journey. As an experienced hospice nurse specializing in compassionate care, I am here to support and guide you through the process, providing you with the information you need to understand what to expect as the disease progresses and how to provide the best care for your loved one at every stage.
When someone you love is extremely sick and needs hospice care, you may feel scared, sad, or angry. You may not know what to do or how to help them. You are not alone. Many people go through this challenging time.
As a hospice nurse, I have met many families who have loved ones in hospice. Some of them are continually active and involved in their care. They ask questions, make decisions, and speak up for their needs. Others are more passive and trusting. They let the doctors, nurses, and staff do whatever they think is best. They don’t say much or ask for anything.
Who do you think gets better care for their loved ones? The active ones or the passive ones?
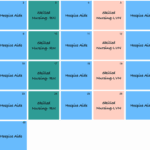
As a hospice nurse, determining the appropriate frequency of scheduled nurse visits for your patients is essential to providing effective and compassionate end-of-life care. Patients and their families often rely on your expertise to ensure comfort and well-being during this sensitive time. In this article, we'll discuss suggested starting scheduled nurse visit frequencies, when to decrease or increase frequencies, and factors to consider based on patient acuity and changes in their condition.
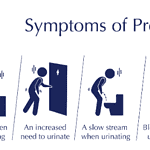
Navigating the path of prostate cancer can be challenging for both patients and their families. As a hospice registered nurse case manager specializing in end-of-life care, I offer you crucial information, guidance, and unwavering support. In this article, we will delve into the journey of prostate cancer, equipping you with insights about what to anticipate, how to identify changes in your loved one's condition and the optimal approaches to caregiving from diagnosis to end-of-life. Throughout this article, I aim to present information clearly and empathetically that resonates with your needs and comprehension.
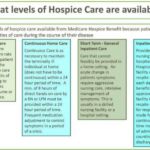
Caring for a loved one who has a terminal illness can be extremely rewarding but also particularly challenging. You may feel exhausted, overwhelmed, or isolated by the demands of caregiving. You may also feel guilty or anxious about taking a break from your loved one. But you deserve time to rest, recharge, and care for yourself. That is why hospice respite care can be a great option for you and your loved one.
Hospice respite care is a service that allows you to temporarily place your loved one in a facility, such as a hospital, nursing home, or hospice house, where they can receive professional care and support. You can use this time to do whatever you need or want, such as sleeping, working, running errands, visiting friends, or enjoying a hobby. Respite care can last up to five days at a time.

Lung cancer presents a difficult path for both individuals facing illness and their loved ones. As a dedicated hospice registered nurse case manager specializing in end-of-life care, my purpose is to equip you with essential insights. This guide aims to enlighten you about the stages of the disease, detecting crucial shifts in your dear one's condition, and delivering optimal care from inception to closure. By sharing this knowledge, my intention is to empower you to provide tender and considerate assistance throughout this profound journey.

Discover compassionate approaches to nourishing terminally ill loved ones. Learn about appetite changes, feeding techniques, and the importance of emotional support during meals. This guide offers practical tips for caregivers to ensure comfort and dignity while addressing nutritional needs in end-of-life care.
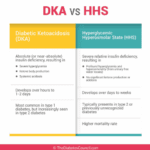
As an experienced hospice nurse, I understand that managing diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) at end of life can be challenging, especially when patients choose to stop taking their diabetic medications or when those medications are no longer an option. In this article, I will provide information on recognizing the signs and symptoms of hyperglycemic crises and outline comfort-based treatment options that align with hospice goals of care.

Discover how hospice patients can safely travel and create lasting memories with loved ones. Learn about essential preparations, medical considerations, and tips for a smooth journey. Explore ways to make the most of precious moments together while ensuring comfort and care during travel.

Caring for a loved one with dementia can be challenging. One common struggle caregivers face is ensuring their loved one takes their medications. Dementia can make understanding and remembering medications difficult. In this guide, we'll explore effective strategies for encouraging your loved ones with dementia to take their medications, considering their unique needs.
Discover the future of hospice care in 2024. This comprehensive guide explores cutting-edge pain management techniques, telemedicine integration, personalized care plans, and enhanced caregiver support. Learn how hospice services evolve to provide more compassionate and effective end-of-life care for patients and their families.

Explore the natural shift in nutritional needs during hospice care. This guide offers insights into managing reduced calorie intake, ensuring comfort and dignity in the end-of-life journey.

Facing the reality of a loved one's terminal illness can be a challenging and emotional journey. As a hospice registered nurse case manager, I understand the importance of providing compassionate and clear information to empower patients, caregivers, and families. In this article, we'll explore how you, as a family member, can use your own observations and senses to recognize the signs that your loved one may be in the terminal stage of their illness. Remember, while medical professionals have their tools, your observations and intuition significantly matter.
Coping with a loved one's stomach cancer diagnosis can feel overwhelming. As a hospice registered nurse case manager, I am here to provide you with vital information to navigate this journey. This guide is designed to equip you with knowledge, allowing you to care for your loved one with empathy and compassion, prioritizing their comfort and overall well-being.

One of the tools doctors uses is called an FDG PET scan. It’s a special kind of test that takes pictures of the brain. FDG is a type of sugar, and PET stands for Positron Emission Tomography. When someone has a PET scan, they get a tiny amount of this sugar injected into their body. Because the brain uses sugar as fuel, the scan can show which parts are working well and which parts aren’t.
This is super helpful because in people with dementia, some parts of the brain don’t use sugar the same way healthy parts do. So, the scan can show doctors these changes and help them understand what’s going on.

I know that the journey you and your loved one are on can be challenging, especially when facing a terminal illness. As an experienced hospice nurse caring for terminally ill patients, I want to provide you with some valuable insights on a common issue that may arise during this time: contractures.
In this article, we will discuss how to use the Beers Criteria to identify PIMs and potential prescribing omissions (PPOs) in hospice patients. PPOs are medications that are indicated but not prescribed for a specific patient or population, or that are prescribed at a suboptimal dose or duration. We will also present 10 case studies to illustrate the medication reconciliation and deprescribing process and the outcomes of medication changes in different scenarios.