Introduction
This article will explore Limbic-Predominant Age-Related TDP-43 Encephalopathy (LATE), a disease that affects memory, thinking, and social skills and is often mistaken for Alzheimer’s. We aim to empower caregivers and families who are new to dealing with LATE. We’ll cover what to expect during the disease, changes in your loved one, and how to provide the best care.
What is LATE?
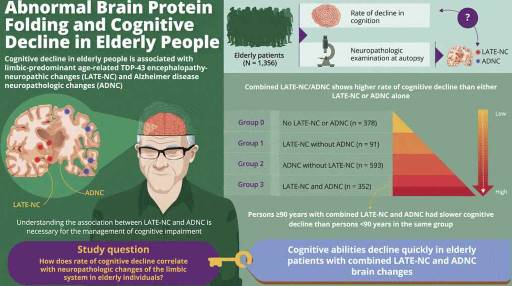
LATE is a newly recognized disease primarily affecting older adults. It involves the accumulation of TDP-43 protein in the brain’s limbic system, responsible for emotions, memory, and behavior. Often coexisting with Alzheimer’s, LATE is frequently missed in clinical diagnosis.
What to Expect Throughout LATE
LATE is a disease that damages the brain and causes problems with memory, thinking, and behavior. It usually starts with mild forgetfulness and confusion but gets worse over time. People with LATE may have trouble remembering facts, conversations, and events. They may also have trouble finding and understanding words. LATE can make it hard to do everyday things like dressing, cooking, or paying bills. LATE can also affect how people act and feel. Some people with LATE may become angry or restless, which can be hard for them and their caregivers. Others may lose interest in things they used to enjoy or have trouble recognizing faces and emotions. LATE can also affect the body, making it harder for people to move around and care for themselves. LATE is a severe disease that has no cure, but there are ways to help people with LATE and their families cope with the challenges.
- Progressive Cognitive Decline: Brain functions that help people learn, remember, and think worsen over time. People with LATE may be unable to recall recent events or follow instructions. They may also have problems with language, such as naming objects or expressing themselves. They may get confused about time, place, or people. These problems can affect their daily lives and communication.
- Behavioral Changes: The disease changes how people act or feel. People with LATE may show different emotions or moods than before. They may become more irritable, anxious, or depressed. They may also have trouble controlling their impulses or emotions. They may act out of character, such as being rude, aggressive, or paranoid. These changes can be stressful for the person with LATE and their caregivers.
- Social Skill Impairment: The disease worsens the ability to interact with others. People with LATE may have trouble understanding social situations, such as what is appropriate or polite. They may also have trouble recognizing the faces or emotions of others. They may lose interest in social activities or withdraw from others. These problems can make them feel lonely or isolated.
- Physical Decline: This means that the body functions that help people move and care for themselves worsen because of the disease. People with LATE may have trouble walking, balancing, or coordinating their movements. They may also have trouble swallowing, eating, or drinking. They may need more help with personal hygiene, such as bathing, dressing, or toileting. These problems can affect their health and quality of life.
Changes in Your Loved One
- Memory Loss: People with LATE may have trouble remembering recent things, such as conversations, appointments, or names. They may also get confused about where they are or what day it is. They may repeat themselves often or ask the same questions over and over. Memory loss is one of the first signs of LATE and worsens over time.
- Language Difficulties: People with LATE may have trouble finding the right words to say what they want. They may also have trouble making sentences or understanding what others are saying. They may mix up words or use words that do not make sense. Language difficulties can make it hard for people with LATE to communicate with their family and friends.
- Personality Changes: People with LATE may act differently than they used to. They may have mood swings, meaning they can get angry, sad, or happy for no reason. They may also be irritable, meaning they get annoyed easily by small things. They may lose interest in things they used to enjoy, such as hobbies, music, or social activities. They may also become more fearful, paranoid, or depressed. Personality changes can affect how people with LATE relate to their family and friends.
- Loss of Independence: People with LATE may need more help with daily tasks as the disease progresses. They may need help dressing, bathing, eating, or taking medications. They may also need help managing their finances, paying bills, or making decisions. They may not be able to drive safely or use public transportation. They may need someone to always watch over them to prevent them from wandering, getting lost, or hurting themselves. Loss of independence can be hard for people with LATE and their family and friends.
How to Best Care for Your Loved One
- Establish a Routine: A consistent schedule provides structure and reduces confusion for people with LATE. It can also help them feel more secure and calm. Keep the same daily routine for waking up, eating, bathing, dressing, and going to bed. Plan activities that the person enjoys and can do safely, such as listening to music, reading, or gardening. Avoid changes that can cause stress or confusion, such as traveling, moving, or introducing new caregivers.
- Create a Safe Environment: Remove hazards, install safety features, and secure cleaning supplies and medications to prevent accidents or injuries for people with LATE. Ensure the person has enough lighting, especially at night, to avoid falls or wandering. Use locks, alarms, or sensors to keep doors and windows secure. Remove or hide objects that can be dangerous, such as knives, scissors, or guns. Store cleaning supplies and medications in a locked cabinet or out of reach: label faucets and appliances with clear instructions. Install grab bars, handrails, and nonslip mats in the bathroom.
- Provide Support: Help with daily activities, like dressing, bathing, and eating, while maintaining the person’s independence and dignity. Allow the person to do as much as possible by themselves but help when needed. Use gentle reminders, cues, or prompts to guide the person through the steps. For example, you can say, “It’s time to brush your teeth. Here is your toothbrush and toothpaste. Can you put some toothpaste on the brush?” Provide choices when possible, such as what to wear or eat, but limit the options to avoid overwhelming the person. Use clothing that is easy to put on and take off, such as Velcro or elastic. Use utensils and dishes that are easy to hold and use, such as spoons and bowls. Cut food into small pieces and check the temperature before serving.
- Seek Support for Yourself: Caregiving is demanding, so connect with support groups, forums, or professional caregivers for advice, emotional support, and respite. You are not alone in this journey; you must care for yourself and the person with LATE. Join a support group, either online or in person, where you can share your experiences and feelings with others who understand. You can also learn from other caregivers’ tips and strategies. Visit websites, such as the Alzheimer’s Association or the National Institute on Aging, for more information and resources on LATE and caregiving. Seek help from professionals, such as social workers, counselors, or home health aides, who can provide information, advice, or assistance. Arrange for respite care at home or in a facility where you can take a break from caregiving and recharge your energy.
- Communicate Effectively: Use simple, plain language, break tasks into steps, and offer visual cues to communicate with the person with LATE. Speak slowly and clearly, using short and simple sentences. Avoid using pronouns, such as he, she, or they, and use the person’s name instead. Avoid asking open-ended questions, such as “What do you want to do today?” and use yes-or-no questions, such as “Do you want to go for a walk?” instead. Break tasks into steps and give one instruction at a time. For example, instead of saying, “Let’s get ready for bed,” you can say, “First, let’s take off your shoes.” Use visual cues, such as pointing, gesturing, or showing, to help the person understand what you mean. For example, you can point to the clock and say, “It’s time for lunch.” Use nonverbal communication, such as eye contact, facial expressions, and touch, to convey your message and emotions. Smile, nod, and hug the person to show your affection and encouragement.
- Ensure Proper Medical Care: Work with the healthcare team to manage symptoms, regular check-ups, medication management, and therapy for the person with LATE. Keep a list of the person’s medical conditions, medications, allergies, and contact information of the doctors and pharmacies. Follow the doctor’s instructions on how and when to give medications and watch for any side effects or interactions. Keep track of the person’s symptoms, such as pain, agitation, or depression, and report any changes or concerns to the doctor. Schedule regular check-ups and tests to monitor the person’s health and adjust the treatment plan. Ask the doctor about therapies that may help the person with LATE, such as physical therapy, occupational therapy, speech therapy, or music therapy.
Signs and Symptoms that Indicate Hospice Care May Be Appropriate for Someone with LATE
Hospice care may be appropriate for someone with LATE if:
- They have a life expectancy of six months or less, as determined by a doctor
- They have frequent or severe infections, falls, or other complications
- They have trouble swallowing, eating, or drinking
- They have lost a lot of weight or muscle strength
- They have difficulty breathing or speaking
- They are bedridden or unable to move without help
- They are not responsive or aware of their surroundings
- They or their family have decided to stop aggressive treatments and focus on comfort care
If you think your loved one with LATE may benefit from hospice care, talk to their doctor about your options. You can also contact a local hospice provider to learn more about their services and eligibility criteria. Hospice care is covered by Medicare, Medicaid, and most private insurance plans.
Hospice care can help your loved one with LATE live with dignity and peace in their final days. It can also help you and your family cope with the challenges and emotions of caring for someone with dementia. Hospice care is not giving up on your loved one but giving them the best possible care at the end of life.
The Importance of Hospice Care for People with Dementia and Their Families
Hospice care can make a difference for people with dementia and their families in the final stages of the disease. Hospice care can help improve the person’s comfort and dignity and reduce their suffering and stress. Hospice care can also help the family cope with the emotional and practical challenges of caring for a loved one with dementia and provide them with guidance and support. Hospice care can help the family prepare for the end of life and the grief process and offer them bereavement services after the death of their loved one.
If you think that hospice care may be right for your loved one with dementia, you should talk to your physician and hospice team about your options and preferences. They can help you determine the eligibility and availability of hospice care and explain the benefits and services that hospice care can provide. They can also help you find and select a hospice provider that meets your needs and expectations.
There are many resources and contact information that you can use to learn more about hospice care and find a hospice provider near you. Some of them are:
Hospice care can be a valuable option for your loved one with dementia and your family. Hospice care can help you make the most of the time you have left with your loved one and provide you with comfort and support. Hospice care can help you honor your loved one’s wishes and values and celebrate their life and legacy. Hospice care can help you say goodbye to your loved one with peace and grace.
Conclusion
Caring for a loved one with LATE is challenging, but understanding the disease and adapting your approach can improve their quality of life. Seek support, maintain a compassionate and structured approach, and remember these keys to providing the best care.
Resources
Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report
Penn Medicine Memory Center: More than half of people with Alzheimer’s also have this brain disease
Alzheimer’s Society LATE-NC
National Insitute on Aging: What Is Limbic-Predominant Age-Related TDP-43 Encephalopathy (LATE)?
TDP-43: From Alzheimer’s Disease to Limbic-Predominant Age-Related TDP-43 Encephalopathy
TDP-43 and Limbic-Predominant Age-Related TDP-43 Encephalopathy
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Caregiver Support Book Series
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Trivia Games – Caregiver Activities for Alzheimer’s and Dementia
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
The 36-Hour Day: A Family Guide to Caring for People Who Have Alzheimer’s Disease and Other Dementias
Caregiver Support Book Series
Dementia Caregiver Essentials: Comprehensive Guide for Dementia Care (one book that contains the ten books below for less than one-third the price of all ten)
Holistic Nurse: Skills for Excellence book series
The Validation Breakthrough: Simple Techniques for Communicating with People with ‘Alzheimer’s-Type Dementia’
Dementia Home Care: How to Prepare Before, During, and After
Atypical Dementias: Understanding Mid-Life Language, Visual, Behavioral, and Cognitive Changes
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Fading Reflection: Understanding the complexities of Dementia
Dementia Caregiving: A Self Help Book for Dementia Caregivers Offering Practical Coping Strategies and Support to Overcome Burnout, Increase Awareness, and Build Mental & Emotional Resilience
Navigating the Dementia Journey: A Compassionate Guide to Understanding, Supporting, and Living With Dementia
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
Four Common Mistakes by Caregivers of Loved Ones with Dementia and What Do Differently (video)
My Loved One with Dementia
Understanding Dementia (Alzheimer’s & Vascular & Frontotemporal & Lewy Body Dementia) (Video)
How Do I Know Which Dementia I’m Looking At? (Video)
Dementia Training material (Free)
Promoting Meaningful Relationships with Dementia Patients through Validation Therapy
Unlocking the Power of Validation Therapy in Compassionate End-of-Life Care
Validation Therapy: A Valuable Tool for Families and Healthcare Teams
Best Practices for Approaching Combative Dementia Patients
Dementia Insights: The Validation Method for Dementia Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
The Validation Breakthrough: Simple Techniques for Communicating with People with Alzheimer’s Disease and Other Dementias
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
How Do I Know You? Dementia at the End of Life
The Dementia Caregiver: A Guide to Caring for Someone with Alzheimer’s Disease and Other Neurocognitive Disorders (Guides to Caregiving)
Sundown Dementia, Vascular Dementia and Lewy Body Dementia Explained
The Caregiver’s Guide to Dementia: Practical Advice for Caring for Yourself and Your Loved One (Caregiver’s Guides)
Ahead of Dementia: A Real-World, Upfront, Straightforward, Step-by-Step Guide for Family Caregivers
The Dementia Caregiver’s Survival Guide: An 11-Step Plan to Understand the Disease and How To Cope with Financial Challenges, Patient Aggression, and Depression Without Guilt, Overwhelm, or Burnout
Dementia Care Companion: The Complete Handbook of Practical Care from Early to Late Stage