Dealing with a loved one in an end-stage coma can be an emotionally challenging and overwhelming experience. As an experienced nurse with years of experience, I understand the importance of providing compassionate care and support during this difficult journey. This article will explore what to expect during the disease, changes you might see in your loved one, and essential tips for caring for them from onset until death.
What is an End-Stage Coma?
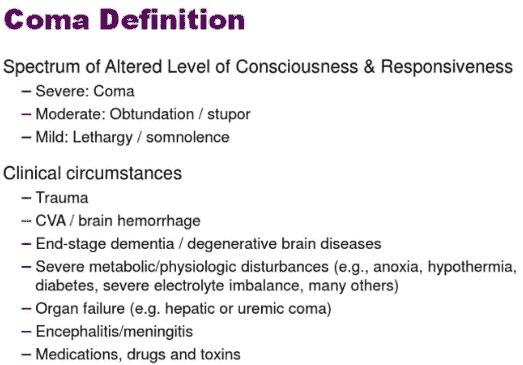
End-stage coma refers to the final stage of a prolonged unconscious state where a person shows no signs of being awake or aware of their surroundings. It often occurs because of severe brain injury, stroke, or a progressive neurological condition. During this stage, the brain’s functions are significantly impaired, and the patient requires specialized care and support.
Signs and Symptoms
In the end stage of the coma, your loved one may display various signs and symptoms that indicate the progression of the condition:
- Unresponsiveness means that your loved one will not react to anything that happens around them. They will not open their eyes, talk, or move when you touch them, speak to them, or shine a light on them.
- No Purposeful Movements: This means that your loved one will not move their body in a way that shows they have a goal or a plan. They may only move because of a reflex, such as blinking, coughing, or muscle spasm.
- Altered Breathing: Your loved one’s breathing may not be normal. They may breathe too fast or slow or stop breathing for a few seconds and then start again. This can happen because brain injury affects the part of the brain that controls breathing.
- Changes in Vital Signs: Your loved one’s blood pressure, heart rate, and body temperature may increase. These are important signs that show how well the body is working. They can change because brain injury affects the part of the brain that regulates the body’s functions.
- Skin Changes: Your loved one’s skin may feel cold and look different. It may lose its normal color and become pale or blotchy. This can happen because the blood flow to the skin is reduced or uneven.
- Changes in Urine Output: Your loved one may make less urine and be darker than usual. This can happen because the kidneys are not working well or the body is losing fluid.
- Difficulty Swallowing: Your loved one may have trouble swallowing food or liquids. They may choke, cough, or spit out what they try to swallow. This can happen because brain injury affects the part of the brain that controls swallowing.
Providing Comfort and Care
During this sensitive time, providing comfort and support for your loved one is essential. Here are some guidelines to help you in caring for them:
- Maintain a Calm Environment: You should try to make the room where your loved one stays as peaceful and relaxing as possible. You can use soft lights, play gentle music, and keep the noise low. This can help your loved one feel more comfortable and less stressed.
- Frequent Position Changes: You should help your loved one move their body every few hours. You can do this by gently lifting and turning them or using pillows or cushions to support them. This can help prevent pressure sores and painful wounds when the skin is pressed against a hard surface for too long.
- Oral Care: Keep your loved one’s mouth and lips wet with a damp cloth or sponge. You can do this by gently wiping their mouth and lips with a moist cloth or sponge or using a special spray or gel. This can help prevent dryness, which can cause cracking, bleeding, or infection.
- Pain Management: You should look for signs that your loved one feels pain or discomfort. Some signs are frowning, grimacing, moaning, sweating, or tensing up. You can do this by watching their face and body and gently touching them. If you see any signs of pain, you should tell the hospice team, who can give your loved one medicine or other treatments to make them feel better.
- Hydration and Nutrition: You should offer your loved one water or ice chips if they can swallow them. You can do this by holding a cup or spoon to their lips and letting them sip or suck slowly. You should not force them to drink or eat, as this can cause choking or vomiting. You should make them feel comfortable rather than worrying about how much they drink or eat.
- Emotional Support: You should talk to your loved one, play their favorite music, or read stories aloud to them. You can do this by speaking softly and kindly, telling them how much you love them, and reminding them of happy memories. You can also play music they like or read books they enjoy. This can help your loved one feel more connected and less lonely.
- Personal Hygiene means gently cleaning and caring for your loved one’s body. You can do this by washing your face, hands, and feet with a warm cloth, brushing your hair, and trimming your nails. You can change your loved one’s clothes, diapers, or pads. This can help your loved one feel more comfortable and cleaner.
- Eye Care: Keep your loved one’s eyes clean and moist. You can do this by gently wiping their eyes with a damp cloth or cotton ball and using eye drops or ointment as the doctor prescribes. This can help prevent dryness, irritation, or infection in the eyes.
- Communication: You should try communicating with your loved one, even if they don’t seem to hear you or respond. You can do this by speaking their name, telling them what day it is, and updating them on what is happening around them. You can also use touch, such as holding their hand, stroking their hair, or hugging them. This can help your loved one feel more aware and less isolated.
- Spiritual Care: Respect your loved one’s spiritual beliefs and needs. You can do this by praying with them, reading from their holy book, or playing their religious music. You can also invite their spiritual leader, such as a priest, rabbi, or imam, to visit them and offer guidance and support. This can help your loved one feel more peaceful and hopeful.
Coping as a Family
Taking care of a loved one in an end-stage coma can be challenging for the entire family. Remember to take care of yourselves and seek support from friends, family, or a counselor if needed. Acknowledging and sharing your feelings, fears, and concerns is crucial. Here are some more ideas on how to cope as a family:
- Talk to each other: This means you should try to communicate with your family members about how you are feeling and what you are going through. You can do this by listening to each other, expressing your emotions, and offering support and comfort. You can also talk about your good memories with your loved one and what they mean. This can help you feel more connected and less alone.
- Take breaks: This means that you should try to do something for yourself every day, even if it’s just for a few minutes. You can do this by doing something you enjoy, like reading, listening to music, or playing a game. You can also do something relaxing, like walking, meditating, or breathing deeply. This can help you feel calmer and more refreshed.
- Ask for help: This means you should try to get help from other people when needed. You can ask your friends, relatives, or neighbors to help you cook, clean, or shop. You can also ask your doctor, nurse, or hospice team to help you with any questions or concerns about your loved one’s care. You can also seek professional help from a counselor, therapist, or support group if you feel overwhelmed or depressed. This can help you feel more supported and less stressed.
- Be gentle with yourself: You should try to be kind and compassionate to yourself. You can do this by not blaming yourself or feeling guilty for anything that happens to your loved one. You can also do this by not comparing yourself to others or expecting too much from yourself. You can also do this by recognizing your strengths and achievements and giving yourself credit for doing your best. This can help you feel more confident and hopeful.
Understanding the Dying Process
As the end stage progresses, your loved one may show signs of nearing death. These signs are a normal part of the body’s natural process:
- Decreased Responsiveness means that your loved one will not react to anything that happens around them. They will not open their eyes, talk, or move when you touch them, speak to them, or shine a light on them. This can happen because brain injury affects the part of the brain that makes them aware and alert.
- Changes in Breathing: Your loved one’s breathing may not be normal. They may breathe too fast or slow or stop breathing for a few seconds and then start again. This is called Cheyne-Stokes breathing. This can happen because brain injury affects the part of the brain that controls breathing.
- Cool Extremities: Your loved one’s hands and feet may feel cold when you touch them. This can happen because the blood flow to the hands and feet is reduced as the body tries to keep the vital organs warm and working.
- Changes in Heart Rate: Your loved one’s heart rate may slow down. This can happen because brain injury affects the part of the brain that regulates the heart rate. This can also happen because the body is shutting down and needs less oxygen and blood.
- Restlessness or Agitation means that your loved one might show signs of being restless or agitated. They might move their arms or legs, make noises, or grimace. This can happen because brain injury affects the part of the brain that controls emotions and behavior. This can also happen because they are feeling pain, discomfort, or anxiety.
- Mottled Skin: Your loved one’s skin might have a mottled appearance, with patches of different colors, such as purple, blue, or red. This can happen because the blood circulation in the skin is uneven as the body tries to keep the vital organs warm and working.
Preparing for the Final Moments
As your loved one approaches their final moments, remember that providing a peaceful and loving presence is your most valuable gift. Consider the following:
- Be Present: This means that you should try to stay with your loved one as much as you can, especially when they are close to dying. You can do this by gently holding their hand, touching their face, and talking to them. You can also tell them who you are and who else is with them. This can help your loved one feel safer and more loved.
- Comfort Measures: You should make your loved one feel more comfortable and less painless. You can do this by moistening their mouth and lips with a damp cloth or sponge or using a special spray or gel. You can also keep them clean by washing their face, hands, and feet with a warm cloth and changing their clothes, diapers, or pads. This can help your loved one feel more relaxed and dignified.
- Express Your Love: You should tell your loved one how much you love and care for them. You can do this by saying words of love and reassurance, such as “I love you,” “You are not alone,” or “You did a great job.” You can also thank them for being a part of your life and say goodbye if ready. This can help your loved one feel more peaceful and happier.
- Seek Support: This means that you should try to get help from others when you feel sad, scared, or tired. You can do this by leaning on the hospice team or other support networks, such as your friends, family, or a counselor. They can help you with your loved one’s care, answer your questions, and listen to your feelings. You can also join a support group or read books or articles about coping with grief. This can help you feel more supported and less alone.
Conclusion
Understanding end-stage coma is crucial for families caring for a loved one in this condition. It is a challenging and emotionally overwhelming experience, but with the right knowledge and support, families can provide compassionate care during this difficult journey. End-stage coma refers to the final stage of a prolonged unconscious state, often resulting from severe brain injury, stroke, or progressive neurological conditions. The patient’s brain functions are significantly impaired during this stage, requiring specialized care and support.
The signs and symptoms of end-stage coma include unresponsiveness, lack of purposeful movements, altered breathing, changes in vital signs, skin changes, changes in urine output, difficulty swallowing, and more. Providing comfort and care during this sensitive time is essential. Families can maintain a calm environment, ensure frequent position changes, provide oral care, manage pain, offer hydration and nutrition, provide emotional support, maintain personal hygiene, offer eye care, communicate, and respect the patient’s spiritual beliefs and needs.
Coping as a family is also crucial. Communication, taking breaks, asking for help, and being gentle with oneself are important strategies. Understanding the dying process is also vital, as the patient may show signs of nearing death, such as decreased responsiveness, changes in breathing, cool extremities, changes in heart rate, and restlessness or agitation.
By understanding these aspects, families can navigate the challenges of end-stage coma with empathy, compassion, and the necessary knowledge to provide the best possible care for their loved one.
Resources
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
The Last Hours of Life
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
Eldercare Locator: a nationwide service that connects older Americans and their caregivers with trustworthy local support resources
CaringInfo – Caregiver support and much more!
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
As an Amazon Associate, I earn from qualifying purchases. The amount generated from these “qualifying purchases” helps to maintain this site.
Caregiver Support Book Series
My Aging Parent Needs Help!: 7-Step Guide to Caregiving with No Regrets, More Compassion, and Going from Overwhelmed to Organized [Includes Tips for Caregiver Burnout]
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Dear Caregiver, It’s Your Life Too: 71 Self-Care Tips To Manage Stress, Avoid Burnout, And Find Joy Again While Caring For A Loved One
Everything Happens for a Reason: And Other Lies I’ve Loved
The Art of Dying
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying