Tag: Comfort Care
Articles about comfort care for the terminally ill patient seeing a good death.
Articles about comfort care for the terminally ill patient seeing a good death.

Considering tube feeding for a loved one who is in the last year of life. This intervention may not improve quality of life and can lead to discomfort, reduced mobility, and complications. Learn about the risks and make informed decisions for their end-of-life care.

I have worked with countless terminally ill patients and their families. One of the most important aspects of hospice care is ensuring that the patient and their loved ones are prepared for the end of life.
In this article, I will cover the topics that hospice nurses should discuss with patients and caregivers to ensure a good death.
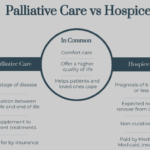
As an experienced hospice nurse, I understand how overwhelming and emotional it can be for terminally ill patients and their loved ones to navigate the hospice process. Hospice care is a compassionate and comprehensive approach to end-of-life care, designed to provide comfort, pain management, and emotional support to patients and their families. However, many people have questions about hospice eligibility and hospice recertification. In this article, I will provide a generalized guide to help you understand these important aspects of hospice care.

I’ve seen firsthand how important it is to understand comfort and discomfort in hospice care. Let’s dive into these terms and how they relate to end-of-life care.

Hospice comfort medications play a vital role in managing end-of-life symptoms. From morphine for pain and breathing difficulties to lorazepam for anxiety and restlessness, these medications are carefully administered to enhance quality of life while ensuring patient comfort and dignity.
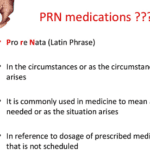
Hey there, my friend! As an experienced hospice nurse, I understand that managing symptoms for comfort is crucial for terminally ill patients. One of the ways we do this is through PRN medications. Today, I want to help you understand PRN medications and how they can be used in conjunction with scheduled medications.
Understanding Hospice Care: A Guide for Families
If you or your loved one is facing a serious illness and needs extra care and support, hospice care may be the right choice. Hospice is a special kind of care that helps people who are nearing the end of their lives feel as comfortable and peaceful as possible.
A review of the implications of each choice for the terminally ill patient as well as the loved ones of those who are terminally ill. This form comes into practice typically under two conditions… no pulse and is not breathing OR has a pulse and/or is breathing (but while not mentioned is typically in the last two weeks of life if no measures are taken with the understanding that any and all measures do not guarantee a longer time frame). Let’s review the form below:

When a loved one nears the end of life, it’s natural to worry about their nutrition and hydration. This article explains why they may not need food or water and how you can provide comfort during this time.
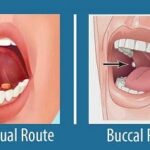
Your dying patient has lost their gag reflex as part of the dying process. One of the questions I implore you to ask yourself is what’s the safest route to administer liquid medications? Well, before even going to answer this question, unless contraindicated, make sure the patient’s head of the bed is at least at a 30 to 45-degree angle (I prefer the latter).
The buccal route is the safest route to administer liquid medications at the end of life in my experience. In practice, I strongly encourage you as well as the families we mutually teach to give any liquid medications on the side of the mouth least likely to have spillage — this depends on the position of the patient — and slowly over time giving the medication in 0.25 ml increments allowing for the absorption of the medication switching cheeks as applicable.

Navigating conversations about Do Not Resuscitate (DNR) orders with terminally ill patients and their families can be challenging yet crucial for ensuring that the patient's wishes and comfort are prioritized. The decision between opting for DNR or full code often involves delicate emotions, medical considerations, and ethical concerns. In this article, we will delve into a methodology that has proven effective in facilitating these discussions, particularly in the context of hospice care. Drawing from years of experience and successful outcomes, we'll explore approaches that prioritize compassion, clarity, and patient-centered care. Additionally, we'll reference valuable resources to enhance understanding and guide these critical conversations.