Finding Comfort Through Palliative Radiation: A Guide for Patients, Families, and Healthcare Providers
Published on November 26, 2025
Updated on November 26, 2025
Published on November 26, 2025
Updated on November 26, 2025
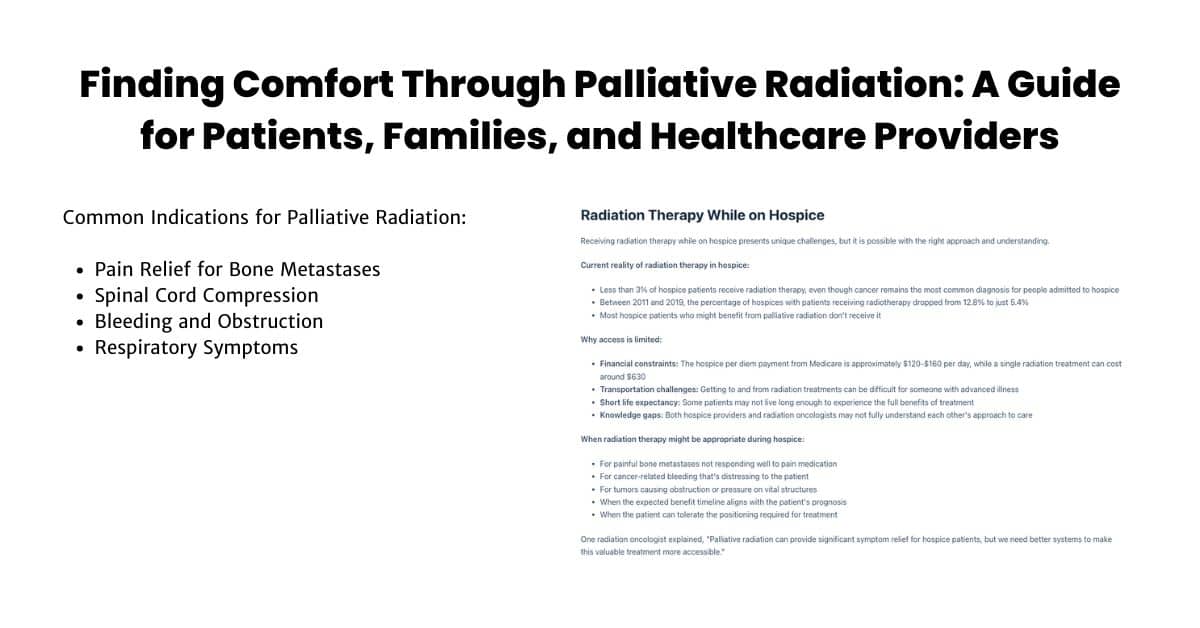
Table of Contents
When someone you care for has advanced cancer, finding ways to improve their comfort becomes a top priority. Palliative radiation therapy is one important option that can help relieve distressing symptoms and improve quality of life. Let’s explore what this treatment involves and how it might benefit your loved one.
Palliative radiation therapy is a specialized treatment that uses high-energy X-rays to target specific areas affected by cancer. Unlike curative radiation treatments that aim to eliminate cancer, palliative radiation focuses on managing symptoms and improving comfort.
Key features of palliative radiation therapy include:
Palliative radiation is part of a broader approach called palliative care, which the World Health Organization defines as care that “improves the quality of life of patients and their families facing problems associated with life-threatening illness.” This approach addresses physical, emotional, and spiritual needs to provide comprehensive comfort.
The primary purpose of palliative radiation is to help your loved one feel better and maintain the best possible quality of life. While it doesn’t aim to cure cancer, it can make a significant difference in how someone feels day-to-day.
The main goals of palliative radiation include:
When discussing palliative radiation with your healthcare team, it’s essential to have clear expectations. The focus is on comfort rather than extending life, though sometimes improved comfort can lead to better overall well-being and function.
Radiation therapy plays a crucial role in managing many distressing symptoms caused by advanced cancer. It’s particularly effective for certain situations that may not respond well to pain medications alone.
Common symptoms managed with palliative radiation include:
| Symptom | How Radiation Helps | Typical Response Time |
|---|---|---|
| Bone pain | Reduces tumor size in bones, decreasing pressure on nerves | Often within 1-2 weeks |
| Headaches from brain metastases | Shrinks tumors in the brain, reducing pressure | Within 1-3 weeks |
| Difficulty breathing | Reduces tumor size in lungs or airways | Can improve within days to weeks |
| Bleeding | Helps heal ulcerated tumors and reduces bleeding | Often within 1-2 weeks |
| Spinal cord compression | Reduces tumor size, relieving pressure on the spinal cord | May require urgent treatment |
| Swallowing difficulties | Shrinks tumors blocking the esophagus | Within 1-2 weeks |
How palliative radiation works:
About two-thirds of patients experience moderate to significant symptom improvement after palliative radiation. Some people notice relief within days of their first treatment, while others may take a few weeks. The benefits can last from several weeks to many months.
Palliative radiation is often combined with other approaches for maximum comfort, including:
When considering palliative radiation for your loved one, remember that the treatment schedule is designed to be convenient and minimize disruption to daily life. Treatment is usually brief, typically lasting only a few minutes, though preparation time may be longer. The radiation oncology team will work with you to create a schedule that balances effective symptom relief with quality-of-life considerations.
Understanding palliative radiation therapy can help you advocate effectively for your loved one and make informed decisions about their care. Always discuss any questions or concerns with your healthcare team, who can provide guidance specific to your situation.
When your loved one is facing cancer, understanding the different types of radiation therapy can help you make informed decisions about their care. Palliative and curative radiation are approaches with very different goals, schedules, and considerations. Let’s explore these differences to help you better understand what to expect.
The most fundamental difference between palliative and curative radiation is the goal of treatment.
Curative radiation therapy aims to:
Palliative radiation therapy aims to:
As one radiation oncologist explained, “Palliative-intent radiation is meant to alleviate symptoms rather than cure the disease.” This distinction is crucial because it shapes every aspect of the treatment approach.
When discussing treatment options with your healthcare team, clarify what matters most to your loved one. If their priority is comfort and quality of remaining life rather than extending life at all costs, palliative radiation may be the more appropriate choice.
The dosing and scheduling of radiation treatments differ significantly between curative and palliative approaches.
| Aspect | Curative Radiation | Palliative Radiation |
|---|---|---|
| Total radiation dose | Higher (50-80 Gy) | Lower (7-35 Gy) |
| Number of treatments | More (often 20-40 sessions) | Fewer (1-10 sessions) |
| Treatment duration | Longer (4-8 weeks) | Shorter (1 day to 2 weeks) |
| Daily dose size | Smaller (1.8-2.0 Gy per day) | Larger (2.5-8 Gy per day) |
| Treatment frequency | Usually 5 days per week | Varies; can be daily or weekly |
This difference in approach is intentional. Curative treatments use smaller daily doses over a more extended period to maximize cancer cell killing while giving normal tissues time to recover. Palliative treatments use larger doses over a shorter time to provide quick symptom relief with minimal disruption to the patient’s life.
For someone with limited life expectancy, a shorter treatment schedule means:
One patient shared, “I didn’t want to spend my remaining time traveling to and from the cancer center. I wanted to be home with my family.”
The approach to side effects differs significantly between curative and palliative radiation.
In curative treatment:
In palliative treatment:
Common short-term side effects of palliative radiation may include:
Your healthcare team should discuss potential side effects and how they’ll be managed. Remember that palliative radiation is designed to minimize these effects while maximizing comfort.
Perhaps the most crucial difference is palliative radiation’s emphasis on quality of life.
Quality of life considerations in palliative radiation include:
When considering palliative radiation, it’s crucial to have honest conversations about what matters most to your loved one. For some, like a 38-year-old nurse with metastatic breast cancer who had only weeks to live, avoiding treatment and spending time with family was the right choice. For others, like a 78-year-old gentleman with multiple myeloma, palliative radiation offered significant symptom relief that improved his quality of life.
Remember that there’s no one-size-fits-all approach. The right decision depends on your loved one’s unique situation, values, and wishes. Your healthcare team can help you weigh the potential benefits against the burdens of treatment to make the choice that best supports your loved one’s comfort and dignity.
By understanding these key differences between palliative and curative radiation, you’ll be better equipped to advocate for care that aligns with your loved one’s goals and values during this challenging time.
When cancer spreads to different parts of the body, it can cause various uncomfortable symptoms that affect your loved one’s quality of life. Palliative radiation therapy can help manage these symptoms and provide relief. Let’s explore the common situations where palliative radiation might be recommended.
When cancer spreads to the bones, it often causes significant pain that can be difficult to control with medications alone. Bone metastases are one of the most common reasons for palliative radiation.
How palliative radiation helps with bone pain:
What to expect with treatment:
The American Society for Radiation Oncology (ASTRO) recommends a single 8 Gy treatment for most patients with painful bone metastases. This approach is just as effective as longer courses of treatment while being more convenient for patients with limited life expectancy.
As one caregiver shared, “My mother’s hip pain from her breast cancer was keeping her awake at night. After one radiation treatment, she felt so much better within two weeks. It made her final months much more comfortable.”
When cancer spreads to the brain, it can cause headaches, nausea, seizures, weakness, and cognitive changes. Palliative radiation can help manage these symptoms and improve quality of life.
Types of radiation for brain metastases:
| Treatment Type | Description | Best For |
|---|---|---|
| Whole Brain Radiation Therapy (WBRT) | Treats the entire brain | Multiple metastases or widespread disease |
| Stereotactic Radiosurgery (SRS) | Precisely targets individual tumors | Limited number of small metastases |
Benefits of palliative radiation for brain metastases:
Treatment decisions depend on several factors, including:
For patients with multiple brain metastases or lesions that are too large or numerous for surgery, whole-brain radiation therapy (WBRT) is typically recommended. This treatment usually involves 5-10 sessions over 1-2 weeks.
Spinal cord compression is considered an emergency situation that requires prompt treatment. It occurs when a tumor puts pressure on the spinal cord, potentially causing permanent paralysis if not addressed quickly.
Warning signs of spinal cord compression include:
Treatment approach:
Palliative radiation for spinal cord compression is well-tolerated and effective in improving neurological symptoms. Studies show that many patients experience pain reduction and neurological improvement after treatment.
Important note: If your loved one develops symptoms of spinal cord compression, seek medical attention immediately. Early treatment is crucial for preventing permanent damage.
Some tumors can cause bleeding or block essential pathways in the body. Palliative radiation can also help in these situations.
Radiation for bleeding:
Research shows that palliative radiation is highly effective for controlling bleeding, with short and longer treatment schedules showing similar effectiveness. However, shorter treatments (fewer than five sessions) are often preferred to minimize the treatment burden and relieve symptoms.
Radiation for obstruction:
A hospice nurse explained, “We had a patient with advanced esophageal cancer who couldn’t swallow even liquids. After a few radiation treatments, he could eat soft foods again, which meant so much to him and his family.”
Cancer affecting the lungs or airways can cause distressing symptoms such as shortness of breath, coughing, or coughing up blood. Palliative radiation can help manage these symptoms.
Benefits for respiratory symptoms:
What to expect:
For someone struggling with breathing difficulties due to cancer, even modest improvements can significantly enhance comfort and quality of life. Palliative radiation offers a way to achieve these improvements with minimal burden.
Remember that palliative radiation is just one tool in the comfort care toolbox. It works best as part of a comprehensive approach that includes medications, emotional support, and other therapies tailored to your loved one’s needs. Always discuss the potential benefits and burdens of treatment with your healthcare team to determine if palliative radiation is the right choice for your specific situation.
If you notice your loved one developing any of the symptoms mentioned above, promptly bring them to the attention of their healthcare team. Early intervention often leads to better symptom control and improved quality of life.
Understanding how palliative radiation works can help you feel more comfortable with this treatment option for your loved one. While the science may seem complex, the basic concepts are straightforward, and knowing them can help you make informed care decisions.
Palliative radiation uses high-energy beams to target cancer cells in specific areas of the body. Unlike treatments aimed at curing cancer, palliative radiation focuses on managing symptoms and improving comfort.
Here’s how radiation helps relieve symptoms:
The effects of palliative radiation aren’t usually immediate. While some patients notice improvement within days, most experience relief within 1-2 weeks after treatment. The benefits can last for months, providing significant comfort during this critical time.
One radiation oncologist explains, “Palliative radiation works by shrinking the tumor or slowing its growth, thereby reducing the pressure it places on surrounding tissues and organs. This leads to symptom relief as the tumor no longer presses on critical structures or causes pain.”
Several methods can deliver palliative radiation, each with specific benefits for different situations. Your healthcare team will recommend the most appropriate approach based on your loved one’s needs.
External Beam Radiation Therapy (EBRT)
This is the most common type of palliative radiation. It delivers radiation from outside the body using a machine called a linear accelerator.
Key features of EBRT include:
Advanced forms of EBRT include:
| Type | Description | Best Used For |
|---|---|---|
| Volumetric Arc Therapy (VMAT) | Delivers radiation while rotating around the patient | Complex tumor shapes, areas near sensitive organs |
| Stereotactic Body Radiotherapy (SBRT) | Delivers high doses with extreme precision | Small, well-defined tumors, especially in the spine, liver, or lung |
| 3D Conformal Radiation | Shapes beams to match the tumor outline | Most common palliative treatments |
Brachytherapy
While less common in palliative care, brachytherapy involves placing radioactive sources directly inside or next to the tumor.
Benefits of brachytherapy:
Your radiation oncologist will explain the most appropriate delivery method for your loved one’s situation. The goal is always to choose the approach that will provide the most symptom relief with the least burden.
Planning palliative radiation treatment involves several steps to ensure the radiation targets the right areas while minimizing exposure to healthy tissues.
The typical planning process includes:
What to expect during planning and treatment:
Important considerations for hospice patients:
For patients receiving hospice care, the radiation oncology team will work closely with the hospice team to coordinate care. Transportation to and from treatments can often be arranged through hospice services. The radiation oncology team understands the importance of minimizing treatment burden while maximizing comfort.
One caregiver shared, “The planning process seemed complicated, but the radiation team explained everything clearly. They were so kind and made sure my father was comfortable throughout. The actual treatments were quick, and he started feeling relief from his bone pain after just a few sessions.”
Remember that the radiation team, including radiation oncologists, therapists, nurses, and support staff, is committed to providing compassionate care focused on your loved one’s comfort and quality of life. Don’t hesitate to ask questions or share concerns at any point in the process.
When considering palliative radiation for your loved one, knowing what to expect can help ease anxiety and prepare everyone involved. This section will walk you through the entire process from initial consultation to post-treatment care, helping you understand what your loved one will experience and how to support them best.
The journey begins with a consultation with a radiation oncologist, a doctor specializing in treating cancer with radiation. This first meeting is crucial for determining if palliative radiation is appropriate and developing a personalized treatment plan.
What happens during the consultation:
Questions to ask during consultation:
Bringing support to the consultation:
It’s helpful to bring someone to this appointment who can:
One caregiver shared, “I was so glad I brought a notebook to my husband’s consultation. There was so much information; writing it down helped us discuss our options later when we were less overwhelmed.”
Palliative radiation schedules are designed to provide symptom relief while minimizing treatment burden. The schedule depends on your loved one’s condition, symptoms, and treatment goals.
Common treatment schedules for palliative radiation:
| Condition | Typical Schedule | Total Sessions | Duration |
|---|---|---|---|
| Bone metastases | Single 8 Gy treatment | 1 | One day |
| Bone metastases (alternative) | 4 Gy per treatment | 5 | One week |
| Brain metastases | 3 Gy per treatment | 10 | Two weeks |
| Spinal cord compression | 4 Gy per treatment | 5 | One week |
| Bleeding/obstruction | 3-4 Gy per treatment | 5-10 | 1-2 weeks |
What influences the treatment schedule?
For hospice patients, radiation oncologists typically recommend the shortest effective schedule to minimize treatment burden while maximizing quality time at home.
While palliative radiation is designed to minimize side effects, some may still occur. Understanding potential side effects and how to manage them can help you provide better support for your loved one.
Common side effects and management strategies:
Important note about pain flare:
Some patients (about 30-40%) experience a temporary increase in pain within the first few days after radiation to bone metastases. This “pain flare” typically resolves within a few days and is often followed by pain relief. Your doctor may prescribe a short course of steroids or adjust pain medications to help manage this temporary symptom.
Knowing what happens during and after radiation treatments can help reduce anxiety and prepare everyone involved.
During treatment days:
Weekly check-ins:
For treatments lasting more than a week, the radiation oncology team will typically schedule weekly check-ins to:
After completing treatment:
Signs of improvement to watch for:
As one family member shared, “My mother’s bone pain improved dramatically about ten days after her radiation treatment. She went from being unable to move without wincing to being able to sit comfortably in her favorite chair again. Those moments of comfort were precious to all of us.”
Remember that the entire healthcare team, including radiation oncologists, therapists, nurses, and your hospice team, is committed to supporting you and your loved one through this process. Don’t hesitate to reach out with questions or concerns at any point during or after treatment.
Understanding the financial aspects of palliative radiation for your loved one is crucial. The costs and coverage options can seem overwhelming, but having this knowledge will help you make informed decisions and advocate effectively for your loved one’s care.
Medicare does cover palliative radiation therapy, but how it’s covered depends on your loved one’s specific situation and which part of Medicare they have.
For patients NOT on hospice:
Medicare coverage for palliative radiation works as follows:
For patients on hospice:
The situation becomes more complex for patients elected to the Medicare hospice benefit. Under Medicare rules, hospice care is expected to cover all treatments related to the terminal illness, including palliative radiation if appropriate.
The Centers for Medicare & Medicaid Services (CMS) has been testing a new payment approach, the Radiation Oncology (RO) Model, that affects how radiation therapy services are paid for under Medicare.
Key features of the RO Model:
This payment model aims to improve the quality of radiation therapy while making costs more predictable. However, there have been concerns about how the model handles palliative cases, particularly for patients with advanced cancer who may need treatment for multiple sites of metastasis.
Some radiation oncologists have expressed concern that the RO Model’s bundled payment approach may inadvertently discourage the use of palliative radiation for patients with multiple metastatic sites, as treating additional sites within the 90-day episode period would not result in extra payment.
When a patient elects the Medicare hospice benefit, the hospice becomes responsible for covering all care related to the terminal illness, including palliative radiation if appropriate. However, this creates significant financial challenges.
The financial challenge:
| Factor | Details |
|---|---|
| Hospice daily rate | Medicare pays hospices approximately $160 per day for routine home care |
| Radiation costs | A single radiation treatment can cost around $630 |
| Multiple treatments | A typical course might cost $1,500-$2,200 |
| Hospice responsibility | Hospices must cover these costs from their daily payment |
This financial reality has led to a significant decline in palliative radiation use for hospice patients. Between 2011 and 2019, the percentage of hospices with patients receiving radiotherapy dropped from 12.8% to just 5.4%. Only about one in twenty hospices has at least one patient per year receive radiotherapy under the hospice benefit.
Potential solutions include:
If you believe your loved one would benefit from palliative radiation, there are several steps you can take to advocate for this care.
For patients NOT on hospice:
For patients on hospice:
Essential considerations when advocating:
Remember that CMS has acknowledged that some hospice-eligible patients would benefit from palliative treatments such as radiation, and is exploring payment mechanisms for high-intensity palliative care services. Advocacy at the individual and system levels is essential to improve access to these beneficial treatments.
As one hospice nurse explained, “When we can coordinate palliative radiation for our patients with painful bone metastases, the relief they experience is remarkable. It often means they can reduce pain medications and enjoy better quality time with their families. We need better systems to make this possible for more patients.”
By understanding the coverage landscape and advocating effectively, you can help ensure your loved one can access the most appropriate comfort-focused treatments during this challenging time.
When someone you love receives hospice care, your role as an advocate becomes especially important. Understanding when palliative radiation might help and how to navigate the healthcare system can make a significant difference in your loved one’s comfort and quality of life.
Not everyone on hospice will benefit from palliative radiation, but for those who do, it can provide meaningful symptom relief. Knowing who might benefit helps you advocate more effectively.
Good candidates for palliative radiation typically have:
Reanne Booker, a nurse practitioner specializing in palliative care, explains, “We must consider a patient’s goals and wishes and ensure that our treatment aligns with what matters most to them.
Situations where palliative radiation might NOT be appropriate include:
Having a thoughtful conversation with healthcare providers helps ensure that palliative radiation is the right choice for your loved one. Consider asking these questions:
Questions about treatment benefits:
Questions about treatment details:
Questions about side effects:
Questions about logistics:
Questions about costs and coverage:
Remember to ask about the Michigan Oncology Quality Consortium pathway or similar programs in your area that might help facilitate palliative radiation for hospice patients with cancer-related bleeding or other symptoms.
Effective coordination between your hospice team and radiation oncology providers is essential for seamless care. Here’s how to help facilitate this coordination:
First steps in coordination:
Important hospice considerations:
Hospice patients can access emergency care without losing their hospice benefits if they follow certain guidelines. However, understanding how radiation therapy fits within hospice care requires special attention:
The healthcare system can be complex, especially when coordinating hospice and radiation oncology services. Here are strategies to help you navigate effectively:
Practical navigation tips:
Overcoming common barriers:
| Barrier | Potential Solutions |
|---|---|
| Financial constraints | Ask about single-fraction treatment, special hospice programs, and financial assistance |
| Distance to treatment facility | Inquire about closer facilities, transportation assistance, or virtual options when possible |
| Coordination challenges | Request a case conference between the hospice and radiation teams, and identify a care coordinator |
| Urgent symptom needs | Ask about expedited pathways, same-day treatment options, and emergency protocols |
| Limited provider knowledge | Bring information about palliative radiation pathways, and request consultation with specialists |
When to seek additional help:
If you encounter significant barriers to accessing appropriate palliative radiation, consider:
Remember that as of May 2025, many healthcare systems are working to improve access to palliative radiation for hospice patients. The Michigan Oncology Quality Consortium pathway and similar programs demonstrate that collaborative approaches can effectively provide this necessary comfort care.
By understanding who might benefit from palliative radiation, asking the right questions, coordinating effectively with your hospice team, and navigating the healthcare system strategically, you can be a powerful advocate for your loved one’s comfort and quality of life during this critical time.
When a loved one enters hospice care, the focus shifts to comfort and quality of life. While many people don’t realize it, palliative radiation therapy can sometimes be an essential part of that comfort care. However, there are special considerations when someone is receiving hospice services.
Receiving radiation therapy while on hospice presents unique challenges, but it is possible with the right approach and understanding.
Current reality of radiation therapy in hospice:
Why is access limited?
When radiation therapy might be appropriate during hospice:
One radiation oncologist explained, “Palliative radiation can provide significant symptom relief for hospice patients, but we need better systems to make this valuable treatment more accessible.”
New approaches to care are emerging that help bridge the gap between hospice and radiation oncology services, making palliative radiation more accessible to those who need it.
Elements of successful collaborative care models:
The Palliative Radiation Oncology Consult (PROC) service model implemented at some institutions has shown impressive results, including:
These collaborative approaches recognize that hospice providers and radiation oncologists share the same goals: relieving symptoms, improving quality of life, and minimizing treatment burden.
One of the most promising models for improving palliative radiation access for hospice patients comes from Michigan. The Michigan Oncology Quality Consortium (MOQC) has developed a specific pathway for hospice patients with cancer-related bleeding.
Key features of the MOQC pathway:
This pathway represents a significant step in ensuring hospice patients have access to effective symptom management through radiation therapy. The MOQC has also developed a similar path for hospice patients with bone metastases.
As one hospice medical director noted, “The MOQC pathway has allowed us to offer radiation therapy to patients who previously would have suffered without it. The streamlined process makes it feasible within our hospice model.”
When considering palliative radiation for someone on hospice, carefully weighing potential benefits against burdens becomes especially important.
Potential benefits to consider:
Potential burdens to evaluate:
Questions to help with decision-making:
Shared decision-making approach:
Remember that what’s right for one person may not be right for another. The decision should always center on the individual’s unique situation, values, and wishes.
As one family member shared, “My father’s bone pain was excruciating despite high doses of pain medication. The single radiation treatment he received through the hospice program made his final weeks so much more comfortable. For him, the brief discomfort of going for treatment was worth the relief it provided.”
Understanding these special considerations for hospice patients allows you to better advocate for appropriate care that aligns with your loved one’s goals and values during this vital time.
When you or your loved one is facing advanced cancer and considering palliative radiation, having access to reliable resources can make a significant difference in your journey. This section provides valuable information about organizations, educational materials, and essential questions to help you navigate this challenging time with greater confidence and support.
Several organizations offer specialized support for cancer patients and their caregivers, providing services ranging from emotional support to financial assistance. These resources can be invaluable during your palliative care journey.
National cancer support organizations:
Local support resources:
Online support communities:
Remember that support organizations can help with various aspects of the cancer journey, including emotional support, practical assistance, and financial guidance. Don’t hesitate to reach out; these organizations exist to help people in your situation.
Access to clear, reliable information about palliative radiation can help you make informed decisions and know what to expect. Here are some valuable educational resources.
Print and online materials:
Multimedia resources:
Practical tools:
When reviewing educational materials, look for resources that:
Your radiation oncology team may provide personalized educational materials for your loved one’s treatment plan. If you need more information or clarification, don’t hesitate to ask for additional resources.
Knowing what questions to ask can help you gather the information you need to make informed decisions about palliative radiation. Here are essential questions organized by stage of care.
Questions about treatment options:
Questions about treatment details:
Questions about side effects:
Questions about skin care during radiation:
Questions about insurance and financial concerns:
Questions about coordination of care:
Remember to write down these questions before appointments and take notes during discussions with your healthcare team. Consider bringing a support person to help listen and remember important information. Many patients and caregivers find keeping a dedicated notebook for medical appointments helpful.
One caregiver shared, “I was overwhelmed at first, but having a list of questions helped me stay focused during appointments. The healthcare team was patient and took time to explain everything. Don’t be afraid to ask for clarification if something isn’t clear.”
These resources, support organizations, educational materials, and key questions can help you navigate the palliative radiation journey with greater confidence and support. Remember that you don’t have to face this challenging time alone; help is available every step of the way.
Discussions Around Palliative Radiation Are Key To Improving Both Patient and Provider Understanding at https://www.oncnursingnews.com/view/discussions-around-palliative-radiation-are-key-to-improving-both-patient-and-provider-understanding
Palliative Radiation Treatment: For Better Quality of Life at https://www.parkwaycancercentre.com/sg/news-events/news-articles/news-articles-details/palliative-radiation-treatment-for-better-quality-of-life_
Episode 204: How Radiation Is Used in Palliative Care (YouTube) at https://www.youtube.com/watch?v=rAYPvyjmqlg
Palliative Radiotherapy Treatment and when should it be used? at https://www.linkedin.com/pulse/palliative-radiotherapy-treatment-when-should-used-roy-r-t-t–aii5f/
Palliative care: Understanding side effects of radiotherapy at https://radiotherapy.org.uk/patients-families/side-effects/palliative-radiotherapy-side-effects/
Palliative radiation therapy pathway for patients on hospice in a statewide quality improvement collaborative at https://ascopubs.org/doi/10.1200/JCO.2022.40.28_suppl.201
Can Hospice Patients Receive Chemotherapy or Radiation? at https://www.1800hospice.com/blog/palliative-chemotherapy-radiotherapy-hospice/
Classification System May Identify QOL Benefit with Palliative Radiotherapy at https://www.cancernetwork.com/view/classification-system-may-identify-qol-benefit-with-palliative-radiotherapy
MOOC Palliative Radiation Pathway at https://moqc.org/project/palliative-radiation-pathway-summer-2022/
Cancer Caregiving A-to-Z: An At-Home Guide for Patients and Families
Things I Wish I’d Known: Cancer Caregivers Speak Out
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
Remember that there is currently no official accrediting body for end-of-life doula programs. Certification only means one graduated from a program. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.