Enhancing Patient Care: Recognizing Subtle Changes in Level of Consciousness for Hospice and Palliative Nurses
Published on August 22, 2025
Updated on August 14, 2025
Published on August 22, 2025
Updated on August 14, 2025
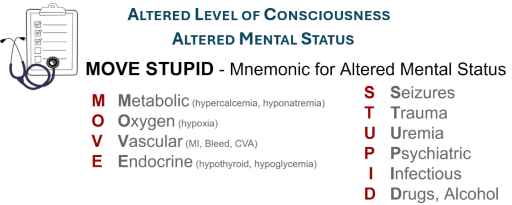
Table of Contents
As hospice and palliative care nurses, you play a crucial role in providing compassionate, high-quality care to patients during some of the most challenging times of their lives. One of the most critical aspects of your role is monitoring your patient’s level of consciousness (LOC). This skill is fundamental to providing effective care and ensuring patient comfort.
The level of consciousness is a crucial indicator of a patient’s neurological status and overall well-being. Regularly assessing LOC is vital for several reasons:
While monitoring LOC is crucial, it can be challenging, especially when changes are subtle. Here are some common difficulties you may encounter:
To help you track these subtle changes over time, consider using a detailed LOC assessment chart:
| Time | Eye Opening | Verbal Response | Motor Response | Pupillary Response | Notes |
|---|---|---|---|---|---|
| 8:00 AM | |||||
| 2:00 PM | |||||
| 8:00 PM |
Remember, your expertise in detecting these subtle changes is invaluable. Your observations can significantly impact patient care quality and family support. Always trust your instincts, and don’t hesitate to communicate your concerns to the interdisciplinary team.
In the following sections, we’ll explore specific assessment techniques, interpretation of changes, and best practices for documentation and communication. This knowledge will empower you to provide your patients with the highest standard of care and support their families during this sensitive time.
As hospice and palliative care nurses, your ability to accurately assess and interpret a patient’s level of consciousness (LOC) is crucial. Let’s explore what LOC means and the tools you can use to assess it effectively.
Level of consciousness refers to a person’s awareness of themselves and their environment. It’s a spectrum that ranges from fully alert to completely unresponsive. LOC has several key components:
In your role, you’ll often encounter patients at various points along this spectrum. Common states of consciousness include:
The Glasgow Coma Scale is a widely used tool for assessing LOC. While it was initially designed for traumatic brain injury patients, it can be helpful in hospice and palliative care settings as well. The GCS evaluates three aspects of responsiveness:
Here’s a breakdown of the GCS scoring:
| Response | Score |
|---|---|
| Eye Opening (E) | |
| Spontaneous | 4 |
| To verbal stimuli | 3 |
| To pain | 2 |
| No response | 1 |
| Verbal Response (V) | |
| Oriented | 5 |
| Confused | 4 |
| Inappropriate words | 3 |
| Incomprehensible sounds | 2 |
| No response | 1 |
| Motor Response (M) | |
| Obeys commands | 6 |
| Localizes pain | 5 |
| Withdraws from pain | 4 |
| Abnormal flexion | 3 |
| Abnormal extension | 2 |
| No response | 1 |
The total GCS score ranges from 3 (completely unresponsive) to 15 (fully alert and oriented). Remember, in hospice and palliative care, the goal isn’t always to achieve the highest score but to use this information to guide comfort-focused care.
While the GCS is valuable, other tools may be more appropriate in hospice and palliative care settings:
When choosing an assessment tool, consider:
Remember, while these tools are valuable, they should always be used with your clinical judgment and knowledge of the patient. Your observations of subtle changes, even those not captured by formal assessments, are invaluable in providing personalized, compassionate care.
In the following sections, we’ll explore how to interpret LOC changes and use this information to enhance patient care and family support. Your skill in this area is critical to the high-quality, empathetic care that defines hospice and palliative nursing.
As hospice and palliative care nurses, understanding the common causes of changes in level of consciousness (LOC) is crucial for optimal care. Let’s explore these causes in detail, remembering that our goal is to enhance patient comfort and quality of life.
Disease progression is often a primary cause of LOC changes in hospice and palliative care patients. Different conditions can affect LOC in various ways:
Remember, LOC changes may signal a transition to end-of-life stages as diseases progress.
Many medications used in palliative care can affect LOC. Be particularly vigilant with:
Always consider recent medication changes or dosage adjustments when assessing LOC changes.
Metabolic issues can significantly impact LOC. Critical imbalances to watch for include:
Regularly monitoring lab values can help identify these issues early when appropriate.
Infections can cause rapid changes in LOC, especially in vulnerable hospice patients. Be alert for:
Remember, classic signs of infection may be absent in hospice patients, so trust your instincts if you suspect an infection.
To help you quickly assess potential causes of LOC changes, use the mnemonic MOVE STUPID:
MOVE:
STUPID:
Let’s break this down further:
| Category | Potential Causes | Assessment Considerations |
|---|---|---|
| Metabolic | Electrolyte imbalances, acid-base disorders | Recent lab results, hydration status |
| Oxygenation | Hypoxia, CO2 retention | Respiratory rate, pulse oximetry |
| Vascular | MI, stroke, bleeding | Vital signs, neurological checks |
| Endocrine | Thyroid dysfunction, diabetes | Blood glucose, recent thyroid tests |
| Seizure | Epilepsy, brain tumors | Witness accounts, post-ictal state |
| Trauma | Falls, subdural hematoma | Recent fall history, physical exam |
| Uremia | Kidney failure | Urine output, recent creatinine levels |
| Psychiatric | Delirium, psychosis | Behavioral changes, hallucinations |
| Infection | UTI, pneumonia, sepsis | Temperature, subtle signs of infection |
| Drugs/Alcohol | Medication side effects, withdrawal | Medication review, substance use history |
When assessing LOC changes, consider:
Remember, your role is to identify the cause of LOC changes and use this information to enhance patient comfort and support families through transitions. Always communicate your findings clearly with the interdisciplinary team to ensure coordinated, compassionate care.
In the following sections, we’ll explore specific strategies for assessing and responding to LOC changes in hospice and palliative care settings. Your expertise in this area is invaluable in providing your patients with the highest quality of care and support to their families during this sensitive time.
As hospice and palliative care nurses, your ability to detect subtle changes in a patient’s level of consciousness (LOC) is crucial. These changes can be early indicators of various issues and significantly impact patient care and comfort. Let’s explore how to recognize these subtle changes effectively.
Establishing a solid baseline is critical to recognizing subtle changes. Here are some techniques to help you create a comprehensive baseline assessment:
Remember to document your baseline assessment thoroughly. This will serve as a crucial reference point for detecting future changes.
Subtle changes in LOC can manifest in various ways. Here are some key red flags to watch for:
Here’s a quick reference table for these red flags:
| Red Flag | What to Look For | How to Assess |
|---|---|---|
| Increased Stimulation Required | • Louder voices needed • Longer response time • Decreased attention span | 1. Compare to baseline 2. Note stimuli intensity 3. Document response quality |
| Sleep-Wake Changes | • More daytime sleeping • Difficulty waking • Day-night reversal | 1. Keep a sleep log 2. Observe sleep quality 3. Note changes in wakefulness |
| Sudden Agitation | • Increased restlessness • Mood changes • Attempts to leave bed | 1. Use the RASS scale (Richmond Agitation-Sedation Scale) 2. Document specific behaviors 3. Identify triggers/patterns |
Understanding a patient’s history is crucial for interpreting LOC changes accurately. Consider the following:
To effectively use a patient’s history:
Remember, your role is to identify and understand changes in the context of the patient’s overall situation. This holistic approach allows for more personalized and effective care.
By mastering these techniques for recognizing subtle LOC changes, you’ll be better equipped to provide timely, compassionate care that addresses your patients’ changing needs. In the following sections, we’ll explore how to respond to these changes and communicate effectively with the care team and family members.
As hospice and palliative care nurses, your ability to perform thorough and accurate assessments is crucial. These advanced techniques will help you gather more detailed information about your patient’s level of consciousness (LOC) and overall neurological status.
Pupillary response can provide valuable insights into a patient’s neurological status. Here’s how to perform and interpret this assessment:
Remember, certain medications (e.g., opioids) can affect pupillary response. Always interpret findings in the context of the patient’s overall condition and medication regimen.
Evaluating motor function can help you assess the patient’s level of responsiveness and identify any neurological deficits.
Here’s a quick reference table for motor responses:
| Response | Description | Significance |
|---|---|---|
| Obeys Commands | The patient follows verbal instructions | Highest level of motor response |
| Localizes Pain | Attempts to remove painful stimulus | Indicates purposeful movement |
| Withdraws from Pain | Pulls away from painful stimulus | Reflex response, lower level of consciousness |
| Abnormal Flexion | Decorticate posturing | Indicates severe brain dysfunction |
| Abnormal Extension | Decerebrate posturing | Indicates very severe brain dysfunction |
| No Response | No movement to any stimulus | Lowest level of motor response |
Evaluating a patient’s verbal response can provide insights into their cognitive function and level of consciousness.
Consider any baseline communication difficulties or language barriers when interpreting verbal responses.
While full cognitive assessments may not always be appropriate in hospice and palliative care settings, simple tests can provide valuable information about a patient’s mental status.
When conducting these tests, always:
Here’s a simple cognitive assessment chart you can use:
| Domain | Task | Patient’s Response | Notes |
|---|---|---|---|
| Orientation | Ask: Name, Place, Date. | ||
| Attention | Spell “WORLD” backwards. | ||
| Memory | Recall three words after 5 minutes. | ||
| Calculation | 100 – 7. |
Remember, the goal of these assessments in hospice and palliative care is not to diagnose cognitive disorders but to:
By mastering these advanced assessment techniques, you’ll be better equipped to provide comprehensive, personalized patient care. Always interpret these assessments in the context of the patient’s overall condition, remembering that the primary goal is to enhance comfort and quality of life.
As hospice and palliative care nurses, your documentation and communication skills are crucial in ensuring quality patient care, supporting continued service eligibility, and informing all stakeholders. Let’s explore these essential aspects of your role further.
In hospice care, documenting changes in level of consciousness (LOC) requires a specific approach focused on demonstrating decline to support continued eligibility. Here are the key principles to follow:
Here’s a table contrasting less effective vs. more effective charting examples:
| Less Effective Charting | More Effective Charting |
|---|---|
| The patient was confused at times. | The patient demonstrates persistent disorientation to time and place and cannot recognize familiar surroundings or identify the current year. This disorientation now impacts safety, with the patient attempting to leave the bed unassisted three times in the past 24 hours, a new behavior since the last assessment. |
| The patient’s speech is slow. | The patient demonstrates persistent disorientation to time and place and cannot recognize familiar surroundings or identify the current year. This disorientation now impacts safety, with the patient attempting to leave the bed unassisted three times in the past 24 hours, a new behavior since the last assessment. |
| The patient’s speech is slow. | The patient was sleepy during the visit. |
Remember to document the presence of new symptoms and the absence or worsening of previous abilities. This clearly shows the patient’s declining trajectory, supporting continued hospice eligibility.
Effective communication within the interdisciplinary team is vital for coordinated care. Here are some strategies to enhance team communication:
Consider using a shared communication board or digital platform to keep all team members informed of key updates:
| Date | LOC Change Observed | Impact on Care | Action Taken | Follow-up Needed |
|---|---|---|---|---|
| 7/18/24 | Monitor response to med changes; reassess in 24 hours; provide family education on aspiration risk. | Unable to participate in PT exercises; difficulty with oral intake. | Adjusted medication schedule; notified physician; speech therapy consult for swallowing assessment. | There is a new onset of agitation during brief wakefulness, attempting to remove oxygen. |
| 7/20/24 | A social worker will assess the family’s coping and consider alternative oxygen delivery methods. | Increased fall risk; compromised oxygen therapy. | Implemented safety precautions; educated family on redirection techniques; consulted with MD re: anxiety management. | There is a new onset of agitation during brief wakefulness, attempting to remove oxygen. |
Engaging and educating family members about LOC changes is crucial to hospice and palliative care. Here’s how to approach this sensitive task:
Create a simple guide for families to track LOC changes:
| Observation | What it Might Mean | How to Respond | When to Contact the Nurse |
|---|---|---|---|
| Sleeping more than usual | It may indicate disease progression or medication effect. | Ensure a quiet, comfortable environment; plan activities during alert periods. | If sleep increases by more than 2 hours per day. |
| Confusion or disorientation | This could be due to various factors, including medication, infection, or disease progression. | Speak calmly, reorient gently, and ensure a safe environment. | Any sudden change in mental status. |
| Difficulty speaking or finding words | This may indicate neurological changes. | Be patient, offer simple choices, and use nonverbal communication. | If communication becomes severely impaired. |
Remember, family education is an ongoing process. Regularly check in with family members to:
Focusing on thorough documentation, effective team communication, and compassionate family involvement ensures that LOC changes are accurately tracked, promptly addressed, and sensitively managed. This approach supports continued hospice eligibility and enhances the quality of care and support provided to patients and their families during this critical time. Your role in this process is invaluable, bridging the clinical aspects of care and the deeply personal experience of patients and their loved ones.
As hospice and palliative care nurses, your role in managing changes in levels of consciousness (LOC) is crucial. Your interventions can significantly impact patient comfort and quality of life. Let’s explore the critical aspects of managing LOC changes.
Quick and appropriate action is essential when you observe acute changes in LOC. Follow these steps:
Here’s a quick reference table for immediate actions:
| LOC Change | Immediate Actions |
|---|---|
| Sudden Unresponsiveness | • Ensure patient safety (remove hazards, implement fall precautions). • Attempt gentle reorientation. • Assess for underlying causes (pain, full bladder, etc.). • Consider the need for medication per order. |
| Acute Confusion/Agitation | • Assess for oversedation from medications. • Check for signs of infection or metabolic imbalance. • Adjust the care schedule to maximize alert periods. • Educate the family on changes and implications. |
| Increased Sleepiness | • Assess for oversedation from medications. • Check for signs of infection or metabolic imbalance. • Adjust the care schedule to maximize alert periods. • Educate the family on changes and implications. |
As LOC changes occur, it’s crucial to adapt the care plan to meet the patient’s evolving needs:
Medication management is critical when dealing with LOC changes. Consider the following:
Here’s a table of common medications used in LOC changes:
| Symptom | Medication Options | Considerations |
|---|---|---|
| Agitation/Delirium | Haloperidol, Risperidone, Quetiapine | Start with low doses; monitor for extrapyramidal side effects. |
| Terminal Restlessness | Midazolam, Lorazepam | It may cause further sedation; discuss goals with family. |
| Pain in Unresponsive Patient | Morphine, Hydromorphone | Continue scheduled doses; use non-verbal pain scales. |
Alongside medication management, non-pharmacological interventions play a crucial role:
Here’s a table summarizing non-pharmacological interventions:
| Intervention | Benefits | Implementation Tips |
|---|---|---|
| Calming Environment | Reduces agitation and promotes relaxation. | Dim lights, minimize noise and use soft music. |
| Therapeutic Touch | It provides comfort and reduces anxiety. | Gentle hand massage, light stroking of arms. |
| Family Presence | Emotional support, familiar voices. | Dim lights, minimize noise and use soft music. |
Remember, your role in managing LOC changes extends beyond clinical interventions. You’re also a guide and support for families navigating this challenging time. Your compassionate care and clear communication can significantly impact the patient and family experience.
By skillfully combining pharmacological and non-pharmacological approaches, adjusting care plans promptly, and responding effectively to acute changes, you can ensure that patients receive optimal comfort and care as their level of consciousness changes. Your expertise in this area is invaluable in providing dignified, patient-centered care in the final stages of life.
As hospice and palliative care nurses, you support patients and families during one of life’s most challenging journeys. Understanding the subtle changes in a patient’s level of consciousness (LOC) is essential for providing compassionate and effective care.
At the end of life, patients often experience changes in their level of consciousness. These changes can be confusing or distressing for family members, so explaining that they are a normal part of the dying process is essential. Some common LOC changes include:
The transitioning phase is a critical time when patients begin to show signs that death is approaching. During this phase, you may observe:
| Sign | Description | Nursing Interventions |
|---|---|---|
| Lethargy | Increased sleepiness and difficulty staying awake. | Ensure comfort, manage symptoms, and educate family. |
| Rallies | Brief periods of increased alertness. | Support family and encourage meaningful interactions. |
| Terminal restlessness | Agitation, confusion in final hours/days. | Assess for underlying causes and provide a calming environment. |
| Agitation | Restless movements, pulling at bedsheets. | Ensure safety, and consider medication if distressing. |
One of the most challenging aspects of hospice and palliative care is finding the right balance between keeping patients comfortable and maintaining their level of consciousness. This balance is crucial for:
When considering medications for symptom management, it’s essential to:
Caring for patients at the end of life often involves complex ethical considerations. Some key points to remember:
| Ethical Principle | Application in Hospice/Palliative Care |
|---|---|
| Respect autonomy | Follow advance directives and involve the patient in decision-making when possible. |
| Non-maleficence | Avoid unnecessary interventions that may cause distress. |
| Beneficence | Provide comfort care and manage symptoms effectively. |
| Justice | Provide equal access to care and resources for all patients. |
As hospice and palliative care nurses, you may face challenging situations such as:
In these situations, it’s essential to:
Remember, your role is to provide compassionate care that aligns with the patient’s wishes and values while supporting their loved ones through this difficult journey.
As hospice and palliative care nurses, your ability to assess a patient’s level of consciousness (LOC) is crucial. Let’s explore ways to improve these vital skills:
Staying up-to-date with the latest knowledge and techniques is essential in our field. Here are some ways to continue your education:
Remember, many of these opportunities offer continuing education units (CEUs) that can help maintain your nursing license.
Simulation training is a powerful way to practice your skills in a safe environment. Here’s what you need to know:
| Type of Simulation | Description | Benefits |
|---|---|---|
| Role-playing | Nurses act out scenarios with colleagues or trained actors. | Improves communication skills and empathy. |
| High-fidelity mannequins | Advanced, lifelike mannequins that can simulate various conditions. | Provides realistic physical assessment practice. |
| Virtual reality (VR) | Computer-generated scenarios experienced through VR headsets. | Allows for diverse scenario practice without physical setup. |
| Case studies | Detailed patient scenarios for analysis and discussion. | Enhances critical thinking and decision-making skills. |
Learning from experienced colleagues can significantly enhance your skills. Here’s how to make the most of mentorship and peer learning:
Remember, enhancing your LOC assessment skills is an ongoing process. By taking advantage of these learning opportunities, you’ll be better equipped to provide the best possible care for your patients. Your commitment to improving these skills shows your dedication to your patients and profession.
As we wrap up our discussion on recognizing subtle changes in level of consciousness (LOC), let’s review the key points and consider the significant impact of your vigilant monitoring on patient care quality.
Let’s revisit the crucial aspects of LOC assessment we’ve covered:
| Evaluate eye response, motor response, brainstem reflexes, and respiration | Key Features | Best Used For |
|---|---|---|
| Glasgow Coma Scale (GCS) | Assesses eye opening, verbal response, and motor response | General LOC assessment, especially in trauma situations |
| FOUR Score | Evaluate eye response, motor response, brainstem reflexes, and respiration | Detailed neurological assessment, useful for intubated patients |
| Richmond Agitation-Sedation Scale (RASS) | Measures agitation and sedation levels | Assessing sedated patients or those with fluctuating agitation |
| Confusion Assessment Method (CAM) | Detailed neurological assessment, practical for intubated patients | Quick assessment for delirium, especially in older adults |
Your careful attention to changes in LOC can significantly improve patient care in several ways:
Remember, your role in assessing LOC is crucial. Each time you perform an assessment, you’re not just checking boxes on a form – you’re gathering vital information that can make a real difference in your patient’s care and comfort.
Your dedication to mastering these skills shows your commitment to providing the best possible care for your patients during some of the most challenging times of their lives. Keep learning, stay observant, and never underestimate the importance of your assessments. Your patients and their families rely on your expertise and compassion.
The D.O.G.I. At The Window Case Study
Nursing Center Assessing Level of Consciousness
Nursing Journal: Documenting level of consciousness
National Library of Medicine: Chapter 57 Level of Consciousness
American Association of Critical Care Nurses: Ongoing Neurological Assessments Reveal Subtle Changes
Daily Nurse Journal: Ongoing Neurological Assessments Reveal Subtle Changes
Neurology: Altered States of Consciousness (PDF)
American Nurse: Evaluating the neurologic status of unconscious patients
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.