Compassionate Care: Managing Nausea, Vomiting, and Dry Heaving in End-of-Life Patients
Published on March 5, 2025
Updated on December 3, 2025
Published on March 5, 2025
Updated on December 3, 2025
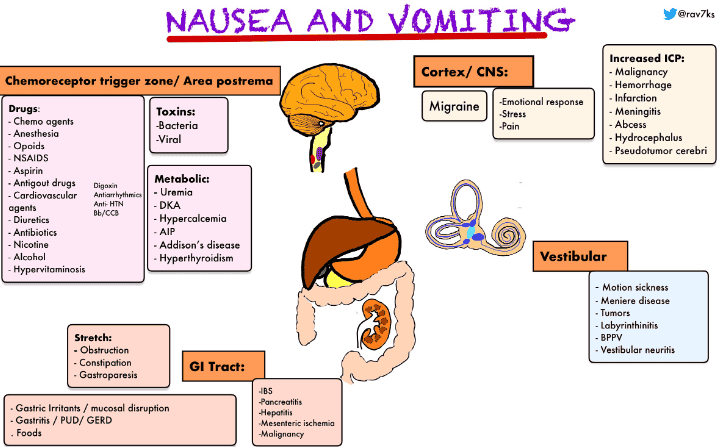
Table of Contents
As hospice nurses, caregivers, and family members, we understand that caring for terminally ill patients can be both rewarding and challenging. One of the most common and distressing symptoms we encounter is nausea and vomiting. Let’s explore this topic together, with compassion and understanding for the patients and those caring for them.
Nausea and vomiting are, unfortunately, very common in terminally ill patients. Studies show that up to 70% of patients with advanced cancer experience these symptoms. This high prevalence isn’t limited to cancer patients, though. Many other terminal illnesses can cause nausea and vomiting, including:
It’s important to remember that each patient’s experience is unique. Some may have occasional mild nausea, while others might struggle with severe, persistent symptoms. As caregivers, we recognize these symptoms and help manage them effectively.
The impact of nausea and vomiting on a terminally ill patient’s quality of life cannot be overstated. These symptoms can affect nearly every aspect of a person’s well-being:
To illustrate the impact, consider this comparison:
| Aspect of Life | Without Nausea/Vomiting | With Severe Nausea/Vomiting |
|---|---|---|
| Eating | Enjoyable, social activity | Dreaded, avoided task |
| Daily Activities | Able to participate | Limited by symptoms |
| Mood | Generally stable | Anxious, irritable |
| Family Time | Engaged and present | Withdrawn, uncomfortable |
As caregivers, we must recognize the profound impact these symptoms can have. By doing so, we can approach our patients with empathy and work diligently to manage their symptoms, improving their comfort and quality of life. Remember: Every effort to alleviate nausea and vomiting can significantly improve our patients’ final days or weeks. Your compassionate care makes a real difference in their lives and the lives of their loved ones. In the following sections, we’ll explore various strategies to help manage these challenging symptoms, always keeping in mind the comfort and dignity of our patients.
As we care for our terminally ill loved ones or patients, it’s essential to understand the symptoms they’re experiencing. Let’s break down nausea, vomiting, and dry heaving to understand better what our patients are experiencing and how we can help.
Nausea, vomiting, and dry heaving are related but distinct experiences:
Understanding that a patient can experience any of these symptoms independently or in combination is crucial. For example, someone might feel nauseous without vomiting, or they might dry heave after an episode of vomiting.
In terminally ill patients, nausea, vomiting, and dry heaving can have various causes. Understanding these can help us provide better care:
The emetic pathway is the sequence of events in the body that leads to vomiting. Understanding this can help us see why certain treatments work:
Here’s a simplified table of the emetic pathway:
| Step | Process | Relevance to Care |
|---|---|---|
| 1. Stimulation | Triggers activate the vomiting center | Identifying and managing triggers can prevent episodes |
| 2. Signaling | The brain communicates with the body | Some medications work by blocking these signals |
| 3. Physical response | Muscles contract to expel stomach contents | Positioning can help make this process less uncomfortable |
Why is this relevant to our care? Understanding the emetic pathway helps us:
Remember: Every patient’s experience is unique. What triggers nausea or vomiting in one person might not affect another. It’s our job to observe, listen to our patients, and work with the healthcare team to find the best solutions for each individual. By understanding these concepts, we can provide more informed, compassionate care to our terminally ill patients. In the following sections, we’ll explore how to assess and manage these symptoms effectively.
As caregivers and healthcare professionals, we strive to deliver the highest quality care to our terminally ill patients. Conducting a thorough assessment is a crucial part of managing nausea, vomiting, and dry heaving. Let’s explore the critical components of this process.
Taking a detailed history is the foundation of understanding our patients’ experience. Here’s what we need to focus on:
Remember: Listen actively and empathetically. Your patient’s words can provide valuable clues about the underlying causes.
A gentle yet thorough physical exam can reveal necessary information:
Tip: Always explain what you’re doing and why. This helps keep the patient comfortable and involved in their care.
While we want to minimize discomfort, some tests may be necessary to guide treatment:
| Investigation | Purpose | When to Consider |
|---|---|---|
| Blood tests | Check for electrolyte imbalances, infection, organ function | In most cases, unless very end-stage |
| Urinalysis | Rule out urinary tract infection | If infection suspected |
| Abdominal X-ray | Check for constipation or bowel obstruction | If abdominal symptoms present |
| CT scan | Identify tumors or metastases | If new neurological symptoms |
Important: Always weigh the benefits of any investigation against the potential discomfort it may cause. Discuss options with the patient and their family. CT Scans may not be covered by hospice.
After gathering all this information, we can begin to piece together what is causing our patient’s symptoms. Here’s a simple approach:
Final thought: Your thorough assessment is the key to effective symptom management. By fully understanding your patient’s experience, you’re laying the groundwork for improved comfort and quality of life.
As caregivers and healthcare professionals, understanding the medications used to manage nausea and vomiting in terminally ill patients is crucial. Let’s explore the various aspects of pharmacological management with empathy and clarity.
There are several classes of antiemetic medications available. Each works in a different way to help control nausea and vomiting:
Selecting the appropriate antiemetic depends on several factors:
Here’s a simple guide to help understand which medications might be considered for different causes:
| Cause of Nausea/Vomiting | First-line Medications to Consider |
|---|---|
| Chemotherapy-induced | Serotonin antagonists, NK1 antagonists |
| Opioid-induced | Haloperidol, metoclopramide |
| Bowel obstruction | Octreotide, dexamethasone |
| Raised intracranial pressure | Dexamethasone |
| Vestibular causes | Antihistamines |
Proper dosing and administration are crucial for effective symptom control:
Remember: Always follow the prescriber’s instructions and consult with the healthcare team before making any changes.
While antiemetics can provide significant relief, they may also cause side effects:
Important interactions to watch for:
Tips for managing side effects:
Final thoughts: Pharmacological management of nausea and vomiting in terminally ill patients requires a thoughtful, individualized approach. As caregivers, your observations and feedback are invaluable in helping the healthcare team fine-tune the treatment plan. Remember, the goal is to provide comfort and improve the quality of life for your loved one or patient.
As caregivers and loved ones, we understand that managing nausea and vomiting in terminally ill patients goes beyond medication. Many gentle, non-pharmacological approaches can significantly affect your patient or family member’s comfort. Let’s explore these methods together.
What we eat and drink can have a significant impact on nausea and vomiting. Here are some helpful strategies:
It’s best to steer clear of:
Here’s a table of foods and drinks that are often well-tolerated:
| Food Category | Recommended Options |
|---|---|
| Proteins | Lean meats, eggs, cold cuts |
| Starches | Crackers, toast, pretzels, rice |
| Fruits | Bananas, applesauce, melon |
| Vegetables | Well-cooked, non-fibrous options |
| Beverages | Clear broths, ginger ale, herbal teas |
Remember: Every person is different. Pay attention to what works best for your loved one.
The surroundings can make a big difference in managing nausea:
Stress and anxiety can worsen nausea. Try these relaxation methods:
While these should not replace prescribed treatments, they can be helpful additions:
Some scents that may help include:
Note: Always check with the healthcare team before using essential oils, as some patients may be sensitive to strong scents.
This involves using the imagination to create calming mental images. It can be:
Final Thoughts: These non-pharmacological approaches can be used in conjunction with prescribed medications to provide comprehensive relief. Always communicate with the healthcare team about what you’re trying and how it’s working. Your observations and care make a difference in your loved one’s comfort. Remember, your compassionate presence is one of the most powerful tools in managing these challenging symptoms. Take care of yourself, too, as you provide this invaluable support.
Managing nausea and vomiting in terminally ill patients involves more than just medications. Simple lifestyle changes can significantly affect comfort and quality of life. Let’s explore some practical strategies.
Rest and proper positioning can help reduce nausea and vomiting. Here are some tips:
Maintaining good oral hygiene is crucial, especially when dealing with nausea and vomiting. It helps keep the mouth clean and can reduce unpleasant tastes that might trigger nausea.
Identifying and avoiding triggers can significantly reduce the frequency and severity of nausea and vomiting.
| Trigger Type | Examples | How to Avoid |
|---|---|---|
| Smells | Cooking odors, perfumes | Ventilate room, use unscented products |
| Foods | Greasy, spicy, heavy foods | Offer bland, easy-to-digest foods |
| Lights | Bright or flickering lights | Use dim lighting, avoid screens |
| Stress | Anxiety, loud noises | Create a calm, quiet environment |
Incorporating these lifestyle changes can help manage nausea and vomiting more effectively. Every patient is unique, so it’s important to tailor these strategies to their needs and preferences. Your compassionate care and attention to these details can significantly affect their comfort and quality of life.
As caregivers and loved ones of terminally ill patients, understanding and managing dehydration is crucial for providing comfort and quality care. Let’s explore this important topic together with compassion and practical insights.
Dehydration can be challenging to identify in terminally ill patients, as some symptoms may overlap with the progression of their illness. However, being aware of these signs can help you provide timely care:
Common signs of dehydration:
Important note: In end-of-life care, it’s natural for patients to reduce their fluid intake as their bodies’ needs change. Not all of these symptoms necessarily indicate a need for increased hydration.
When appropriate, there are several gentle ways to help maintain hydration:
Here’s a helpful table of hydration strategies:
| Method | Description | Benefits |
|---|---|---|
| Ice chips | Small pieces of ice to suck on | Provides hydration without large volumes |
| Mouth swabs | Sponge-tipped swabs moistened with water | Helps relieve dry mouth |
| Lip balm | Apply regularly to lips | Prevents cracking and discomfort |
| Flavored water | Add a slice of lemon or cucumber | May encourage more intake |
Remember: The goal is comfort, not necessarily to achieve a specific fluid intake.
Managing hydration in terminally ill patients is about balancing comfort and medical needs. Your loving care and attention to these details can have a profoundly positive impact on your loved one’s final days. Remember, you’re not alone in this journey – don’t hesitate to contact the hospice team for support and guidance.
Caring for terminally ill patients involves more than just managing physical symptoms. It requires a holistic approach that balances symptom management with patient comfort, addresses emotional and psychological needs, and supports caregivers. Let’s explore these aspects in detail.
Balancing symptom management with patient comfort is a delicate task. Here are some key points to consider:
Example Table: Balancing Symptom Management and Comfort
| Symptom | Management Strategy | Comfort Measures |
|---|---|---|
| Pain | Opioids, NSAIDs | Soft bedding, gentle massage |
| Nausea/Vomiting | Antiemetics, diet | Small, frequent meals, cool room |
| Anxiety | Benzodiazepines | Calm environment, soothing music |
Emotional and psychological support is crucial for terminally ill patients. Here are some strategies:
Example Table: Addressing Emotional and Psychological Needs
| Need | Strategy | Example Actions |
|---|---|---|
| Emotional | Counseling, support groups | Arrange sessions with a counselor |
| Psychological | Medication for anxiety/depression | Prescribe appropriate medications |
| Spiritual | Chaplain services, personal rituals | Facilitate visits from spiritual advisors |
Caregivers play a vital role in end-of-life care, and their well-being is crucial. Here are ways to support them:
Example Table: Supporting Caregivers
| Support Type | Strategy | Example Actions |
|---|---|---|
| Practical | Help with chores, respite care | Arrange for a volunteer to assist with housework |
| Emotional | Counseling, support groups | Connect caregivers with local support groups |
| Educational | Training, resources | Provide pamphlets and training sessions on caregiving |
Balancing symptom management with patient comfort, addressing emotional and psychological needs, and supporting caregivers are all critical components of end-of-life care. By focusing on these areas, we can provide compassionate and comprehensive care that honors the dignity and wishes of our patients and supports their loved ones through this challenging time.
As caregivers and healthcare professionals, it’s crucial to know when to seek additional help for managing nausea, vomiting, and dry heaving in terminally ill patients. Recognizing red flags, effectively communicating with the healthcare team, and understanding emergencies are vital components of comprehensive care.
Certain symptoms indicate that a patient may need immediate medical attention. These red flags can signal serious underlying issues that require prompt intervention:
Common red flags to watch for:
Example Table: Red Flags and Warning Signs
| Symptom | Description | Action Needed |
|---|---|---|
| Persistent vomiting | It lasts more than 48 hours | Contact healthcare provider |
| Dehydration signs | Dry mouth, sunken eyes, confusion | Seek medical attention |
| Vomiting blood/bile | Blood or greenish bile in vomit | Immediate medical help |
| Severe abdominal pain | Intense or worsening stomach pain | Urgent medical evaluation |
| Neurological symptoms | Severe headache, confusion, fever | Emergency medical care |
Effective communication with the healthcare team is crucial for managing symptoms and ensuring optimal care for the patient. Here are some tips:
Example Table: Communicating with the Healthcare Team
| Communication Tip | Description | Example |
|---|---|---|
| Be clear and concise | Accurate symptom description | “Patient has been vomiting every 2 hours for the past 24 hours.” |
| Keep a symptom diary | Record episodes and triggers | “Noticed increased nausea after meals.” |
| Ask questions | Clarify treatment plans | “What can we do to manage the side effects of this medication?” |
| Share observations | Report new symptoms | “Patient is now experiencing severe abdominal pain.” |
In some cases, immediate medical intervention is necessary. Recognizing these emergencies can save lives and improve patient outcomes:
Common palliative care emergencies:
Example Table: Emergency Situations
| Emergency Situation | Symptoms | Action Needed |
|---|---|---|
| Spinal cord compression | Severe back pain, leg weakness | Seek emergency medical care |
| Superior vena cava obstruction | Swelling of face/neck, breathing issues | Immediate medical attention |
| Hypercalcemia | Nausea, vomiting, confusion | Urgent medical evaluation |
| Neutropenic sepsis | Fever, chills, rapid heart rate | Emergency medical care |
| Severe hemorrhage | Heavy bleeding, dizziness | Call emergency services |
Knowing when to seek additional help is vital for the well-being of terminally ill patients. Caregivers can provide timely and effective care by recognizing red flags, maintaining clear communication with the healthcare team, and understanding emergencies. Your attentiveness and compassion are crucial in ensuring the best possible quality of life for your loved ones.
As we conclude our discussion on managing nausea, vomiting, and dry heaving in end-of-life patients, let’s reflect on the key points and emphasize the importance of individualized care and ongoing assessment.
Throughout this article, we’ve covered several crucial aspects of managing these challenging symptoms:
Every patient’s journey is unique, and this is especially true in end-of-life care. Individualized care is crucial for several reasons:
Table: Benefits of Individualized Care
| Aspect | Benefit |
|---|---|
| Patient comfort | Tailored interventions lead to better symptom control |
| Quality of life | Addressing individual needs improves overall well-being |
| Family satisfaction | Personalized care helps families feel heard and supported |
| Resource utilization | Targeted interventions can be more cost-effective |
Managing symptoms in end-of-life care is not a one-time task but an ongoing process. Here’s why continuous assessment and adjustment are vital:
Steps for ongoing assessment:
As caregivers and healthcare professionals, your compassionate and attentive care makes a world of difference to patients and their families during this challenging time. Remember that managing nausea, vomiting, and dry heaving is just one part of providing comprehensive, person-centered end-of-life care. By staying informed, responsive, and empathetic, you can help ensure your patients experience the best possible quality of life in their final days. Your dedication to individualized care and ongoing assessment is a testament to the profound impact of hospice and palliative care. I appreciate your commitment to this vital and meaningful work. Your efforts bring comfort and dignity to those who need it most.
Managing nausea and vomiting in the last days of life
Nausea and Vomiting, Sources and Palliative Management
The Management of Nausea at the End of Life (PDF)
Nausea, Vomiting, and Retching: Complex Problems in Palliative Care
Managing Common Gastrointestinal Symptoms at the End of Life (PDF)
Nausea and vomiting in palliative care
Crisis Management at End-of-Life
Articles on Advance Directives
CaringInfo – Caregiver support and much more!
The Hospice Care Plan (guide) and The Hospice Care Plan (video series)
Surviving Caregiving with Dignity, Love, and Kindness
Caregivers.com | Simplifying the Search for In-Home Care
Geri-Gadgets – Washable, sensory tools that calm, focus, and connect—at any age, in any setting
Healing Through Grief and Loss: A Christian Journey of Integration and Recovery
📚 This site uses Amazon Associate links, which means I earn a small commission when you purchase books or products through these links—at no extra cost to you. These earnings help me keep this website running and free from advertisements, so I can continue providing helpful articles and resources at no charge.
💝 If you don’t see anything you need today but still want to support this work, you can buy me a cup of coffee or tea. Every bit of support helps me continue writing and sharing resources for families during difficult times. 💙
VSED Support: What Friends and Family Need to Know
Take Back Your Life: A Caregiver’s Guide to Finding Freedom in the Midst of Overwhelm
The Conscious Caregiver: A Mindful Approach to Caring for Your Loved One Without Losing Yourself
Everything Happens for a Reason: And Other Lies I’ve Loved
Final Gifts: Understanding the Special Awareness, Needs, and Communications of the Dying
Between Life and Death: A Gospel-Centered Guide to End-of-Life Medical Care
Providing Comfort During the Last Days of Life with Barbara Karnes RN (YouTube Video)
Preparing the patient, family, and caregivers for a “Good Death.”
Velocity of Changes in Condition as an Indicator of Approaching Death (often helpful to answer how soon? or when?)
The Dying Process and the End of Life
Gone from My Sight: The Dying Experience
The Eleventh Hour: A Caring Guideline for the Hours to Minutes Before Death
By Your Side, A Guide for Caring for the Dying at Home
Top 30 FAQs About Hospice: Everything You Need to Know
Understanding Hospice Care: Is it Too Early to Start Hospice?
What’s the process of getting your loved one on hospice service?
Picking a hospice agency to provide hospice services
National Hospice Locator and Medicare Hospice Compare
Holistic Nurse: Skills for Excellence book series
Empowering Excellence in Hospice: A Nurse’s Toolkit for Best Practices book series
Tips for Hospice Nurses – Numerous Articles
Bridges to Eternity: The Compassionate Death Doula Path book series:
Additional Books for End-of-Life Doulas
VSED Support: What Friends and Family Need to Know
Find an End-of-Life Doula
At present, no official organization oversees end-of-life doulas (EOLDs). Remember that some EOLDs listed in directories may no longer be practicing, so it’s important to verify their current status.
End-of-Life Doula Schools
The following are end-of-life (aka death doula) schools for those interested in becoming an end-of-life doula:
The International End-of-Life Doula Association (INELDA)
University of Vermont. End-of-Life Doula School
Kacie Gikonyo’s Death Doula School
Laurel Nicholson’s Faith-Based End-of-Life Doula School
National End-of-Life Doula Alliance (NEDA) – not a school, but does offer a path to certification
Remember that there is currently no official accrediting body for end-of-life doula programs. It’s advisable to conduct discovery sessions with any doula school you’re considering—whether or not it’s listed here—to verify that it meets your needs. Also, ask questions and contact references, such as former students, to assess whether the school offered a solid foundation for launching your own death doula practice.